Abstract
Purpose
Primary aldosteronism (PA) remains, to a large extent, an under-diagnosed disease. We aimed to develop and validate a novel clinical nomogram to predict PA based on routine biochemical variables including new ones, calcium-phosphorus product.
Methods
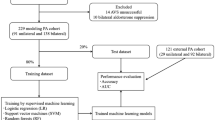
Records from 806 patients with hypertension were randomly divided into 70% (n = 564) as the training set and the remaining 30% (n = 242) as the validation set. Predictors for PA were extracted to construct a nomogram model based on regression analysis of the training set. An internal validation was performed to assess the nomogram model’s discrimination and consistency using the area under the curve for receiver operating characteristic curves and calibration plots. The diagnostic accuracy was compared between nomogram and other known prediction models, using receiver operating characteristics (ROC) and decision curve analyses (DCA).
Results
Female gender, serum potassium, serum calcium-phosphorus product, and urine pH were adopted as predictors in the nomogram. The nomogram resulted in an area under the curve of 0.73 (95% confidence interval: 0.68–0.78) in the training set and an area under the curve of 0.68 (0.59–0.75) in the validation set. Predicted probability and actual probability matched well in the nomogram (p > 0.05). Based on ROC and DCA, 21–70% threshold to predict PA in the nomogram model was clinically useful.
Conclusions
We have developed a novel nomogram to predict PA in hypertensive individuals based on routine biochemical variables. External validation is needed to further demonstrate its predictive ability in primary care settings.



Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Code availability
SPSS Statistics v.22.0 (IBM, Armonk, NY) or R Software v.4.0.2 (The R Project for Statistical Computing, www.r-project.org).
References
L. Mosso, C. Carvajal, A. González, A. Barraza, F. Avila, J. Montero, A. Huete, A. Gederlini, C.E. Fardella, Primary aldosteronism and hypertensive disease. Hypertension 42(2), 161–165 (2003). https://doi.org/10.1161/01.HYP.0000079505.25750.11
S. Monticone, J. Burrello, D. Tizzani, C. Bertello, A. Viola, F. Buffolo, L. Gabetti, G. Mengozzi, T.A. Williams, F. Rabbia, F. Veglio, P. Mulatero, Prevalence and Clinical Manifestations of Primary Aldosteronism Encountered in Primary Care Practice. J. Am. Coll. Cardiol. 69(14), 1811–1820 (2017). https://doi.org/10.1016/j.jacc.2017.01.052
Z. Xu, J. Yang, J. Hu, Y. Song, W. He, T. Luo, Q. Cheng, L. Ma, R. Luo, P.J. Fuller, J. Cai, Q. Li, S. Yang, Chongqing Primary Aldosteronism Study (CONPASS) Group. Primary Aldosteronism in Patients in China With Recently Detected Hypertension. J. Am. Coll. Cardiol. 75(16), 1913–1922 (2020). https://doi.org/10.1016/j.jacc.2020.02.052.
G.P. Rossi, G. Bernini, C. Caliumi, G. Desideri, B. Fabris, C. Ferri, C. Ganzaroli, G. Giacchetti, C. Letizia, M. Maccario, F. Mallamaci, M. Mannelli, M.J. Mattarello, A. Moretti, G. Palumbo, G. Parenti, E. Porteri, A. Semplicini, D. Rizzoni, E. Rossi, M. Boscaro, A.C. Pessina, F. Mantero, PAPY Study Investigators. A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients. J. Am. Coll. Cardiol. 48(11), 2293–3000 (2006). https://doi.org/10.1016/j.jacc.2006.07.059
S. Monticone, F. D’Ascenzo, C. Moretti, T.A. Williams, F. Veglio, F. Gaita, P. Mulatero, Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 6(1), 41–50 (2018). https://doi.org/10.1016/S2213-8587(17)30319-4
M. Parasiliti-Caprino, C. Lopez, N. Prencipe, B. Lucatello, F. Settanni, G. Giraudo, D. Rossato, G. Mengozzi, E. Ghigo, A. Benso, M. Maccario, Prevalence of primary aldosteronism and association with cardiovascular complications in patients with resistant and refractory hypertension. J. Hypertens. 38(9), 1841–1848 (2020). https://doi.org/10.1097/HJH.0000000000002441
G.L. Hundemer, Primary Aldosteronism: cardiovascular Outcomes Pre- and Post-treatment. Curr. Cardiol. Rep. 21(9), 93 (2019). https://doi.org/10.1007/s11886-019-1185-x
A. Vaidya, P. Mulatero, R. Baudrand, G.K. Adler, The Expanding Spectrum of Primary Aldosteronism: Implications for Diagnosis, Pathogenesis, and Treatment. Endocr. Rev. 39(6), 1057–1088 (2018). https://doi.org/10.1210/er.2018-00139
F. Buffolo, S. Monticone, J. Burrello, M. Tetti, F. Veglio, T.A. Williams, P. Mulatero, Is Primary Aldosteronism Still Largely Unrecognized? Horm. Metab. Res. 49(12), 908–914 (2017). https://doi.org/10.1055/s-0043-119755
B.C. Ruhle, M.G. White, S. Alsafran, E.L. Kaplan, P. Angelos, R.H. Grogan, Keeping primary aldosteronism in mind: Deficiencies in screening at-risk hypertensives. Surgery 165(1), 221–227 (2019). https://doi.org/10.1016/j.surg.2018.05.085
P. Mulatero, S. Monticone, J. Burrello, F. Veglio, T.A. Williams, J. Funder, Guidelines for primary aldosteronism: uptake by primary care physicians in Europe. J. Hypertens. 34(11), 2253–2257 (2016). https://doi.org/10.1097/HJH.0000000000001088
J.M. Brown, M. Siddiqui, D.A. Calhoun, R.M. Carey, P.N. Hopkins, G.H. Williams, A. Vaidya, The Unrecognized Prevalence of Primary Aldosteronism: a Cross-sectional Study. Ann. Intern. Med. 173(1), 10–20 (2020). https://doi.org/10.7326/M20-0065. Epub 2020 May 26
J.W. Funder, R.M. Carey, F. Mantero, M.H. Murad, M. Reincke, H. Shibata, M. Stowasser, W.F. Young Jr, The Management of Primary Aldosteronism: Case Detection, Diagnosis, and Treatment: an Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 101(5), 1889–1916 (2016). https://doi.org/10.1210/jc.2015-4061
S.C. Käyser, T. Dekkers, H.J. Groenewoud, G.J. van der Wilt, J. Carel Bakx, M.C. van der Wel, A.R. Hermus, J.W. Lenders, J. Deinum, Study Heterogeneity and Estimation of Prevalence of Primary Aldosteronism: a Systematic Review and Meta-Regression Analysis. J. Clin. Endocrinol. Metab. 101(7), 2826–2835 (2016). https://doi.org/10.1210/jc.2016-1472
R.J. Auchus, Primary aldosteronism and a Texas two-step. Rev. Endocr. Metab. Disord. 12(1), 37–42 (2011). https://doi.org/10.1007/s11154-011-9157-5.
T. Yamashita, S. Shimizu, M. Koyama, K. Ohno, T. Mita, T. Tobisawa, A. Takada, N. Togashi, Y. Ohnuma, T. Hasegawa, A. Tsuchida, T. Endo, T. Ando, H. Yoshida, S. Fukuma, S. Fukuhara, N. Moniwa, T. Miura, Screening of primary aldosteronism by clinical features and daily laboratory tests: combination of urine pH, sex, and serum K. J. Hypertens. 36(2), 326–334 (2018). https://doi.org/10.1097/HJH.0000000000001511
N. Kietsiriroje, R. Wonghirundecha, O. Suntornlohanakul, R.D. Murray, Construction of a predictive scoring system as a guide to screening and confirmation of the diagnosis of primary aldosteronism. Clin. Endocrinol. (Oxf.) 92(3), 196–205 (2020). https://doi.org/10.1111/cen.14142
Y. Jiang, C. Zhang, L. Ye, T. Su, W. Zhou, L. Jiang, Y. Zhang, W. Wang, Factors affecting parathyroid hormone levels in different types of primary aldosteronism. Clin. Endocrinol. (Oxf.) 85(2), 267–274 (2016). https://doi.org/10.1111/cen.12981
J.W. Funder, R.M. Carey, C. Fardella, C.E. Gomez-Sanchez, F. Mantero, M. Stowasser, W.F. Young Jr, V.M. Montori, Endocrine Society. Case detection, diagnosis, and treatment of patients with primary aldosteronism: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 93(9), 3266–3281 (2008). https://doi.org/10.1210/jc.2008-0104
Y. Song, S. Yang, W. He, J. Hu, Q. Cheng, Y. Wang, T. Luo, L. Ma, Q. Zhen, S. Zhang, M. Mei, Z. Wang, H. Qing, D. Bruemmer, B. Peng, Q. Li, Chongqing Primary Aldosteronism Study (CONPASS) Group†. Confirmatory Tests for the Diagnosis of Primary Aldosteronism: a Prospective Diagnostic Accuracy Study. Hypertension 71(1), 118–124 (2018). https://doi.org/10.1161/HYPERTENSIONAHA.117.10197
G.P. Rossi, R.J. Auchus, M. Brown, J.W. Lenders, M. Naruse, P.F. Plouin, F. Satoh, W.F. Young Jr, An expert consensus statement on use of adrenal vein sampling for the subtyping of primary aldosteronism. Hypertension 63(1), 151–160 (2014). https://doi.org/10.1161/HYPERTENSIONAHA.113.02097
M.K. Kwak, J.Y. Lee, B.J. Kim, S.H. Lee, J.M. Koh, Effects of Primary Aldosteronism and Different Therapeutic Modalities on Glucose Metabolism. J. Clin. Med. 8(12), 2194 (2019). https://doi.org/10.3390/jcm8122194
A.M.A. Berends, E. Buitenwerf, E.G. Gruppen, W.J. Sluiter, S.J.L. Bakker, M.A. Connelly, M.N. Kerstens, R.P.F. Dullaart, Primary aldosteronism is associated with decreased low-density and high-density lipoprotein particle concentrations and increased GlycA, a pro-inflammatory glycoprotein biomarker. Clin. Endocrinol. (Oxf.) 90(1), 79–87 (2019). https://doi.org/10.1111/cen.13891
M. Namba, K. Kikuchi, H. Komura, S. Suzuki, N. Satoh, T. Ohtomo, T. Takada, S. Marusaki, O. Iimura, Study on uric acid metabolism in patients with primary aldosteronism. Nihon Naibunpi Gakkai Zasshi 68(1), 51–61 (1992). https://doi.org/10.1507/endocrine1927.68.1_51
H.H. Loh, A. Yee, H.S. Loh, Bone health among patients with primary aldosteronism: a systematic review and meta-analysis. Minerva Endocrinol. 44(4), 387–396 (2019). https://doi.org/10.23736/S0391-1977.18.02867-5
R. Shioji, S. Abe, S. Rikimaru, Effects of Salt Restriction, Spironolactone, and Ammonium Chloride on Acid-base Relations in a Case of Primary Aldosteronism. Tohoku J. Exp. Med. 84(4), 339–348 (1965). https://doi.org/10.1620/tjem.84.339
Z.R. Zhou, W.W. Wang, Y. Li, K.R. Jin, X.Y. Wang, Z.W. Wang, Y.S. Chen, S.J. Wang, J. Hu, H.N. Zhang, P. Huang, G.Z. Zhao, X.X. Chen, B. Li, T.S. Zhang, In-depth mining of clinical data: the construction of clinical prediction model with R. Ann. Transl. Med. 7(23), 796 (2019). https://doi.org/10.21037/atm.2019.08.63
K.G.M. Moons, R.F. Wolff, R.D. Riley, P.F. Whiting, M. Westwood, G.S. Collins, J.B. Reitsma, J. Kleijnen, S. Mallett, PROBAST: A Tool to Assess Risk of Bias and Applicability of Prediction Model Studies: Explanation and Elaboration. Ann. Intern. Med. 170(1), W1–W33 (2019). https://doi.org/10.7326/M18-1377
D. Goltzman, M. Mannstadt, C. Marcocci, Physiology of the Calcium-Parathyroid Hormone-Vitamin D Axis. Front. Horm. Res. 50, 1–13 (2018). https://doi.org/10.1159/000486060
T.H. Toh, C.V. Tong, H.C. Chong, Primary aldosteronism-not just about potassium and blood pressure. QJM 110(3), 175–177 (2017). https://doi.org/10.1093/qjmed/hcw224.
A.S. Salcuni, V. Carnevale, C. Battista, S. Palmieri, C. Eller-Vainicher, V. Guarnieri, F. Pugliese, G. Guglielmi, G. Desina, S. Minisola, I. Chiodini, A. Scillitani, Primary aldosteronism as a cause of secondary osteoporosis. Eur. J. Endocrinol. 177(5), 431–437 (2017). https://doi.org/10.1530/EJE-17-0417
L. Petramala, L. Zinnamosca, A. Settevendemmie, C. Marinelli, M. Nardi, A. Concistrè, F. Corpaci, G. Tonnarini, G. De Toma, C. Letizia, Bone and mineral metabolism in patients with primary aldosteronism. Int J. Endocrinol. 2014, 836529 (2014). https://doi.org/10.1155/2014/836529
C. Maniero, A. Fassina, T.M. Seccia, A. Toniato, M. Iacobone, M. Plebani, R. De Caro, L.A. Calò, A.C. Pessina, G.P. Rossi, Mild hyperparathyroidism: a novel surgically correctable feature of primary aldosteronism. J. Hypertens. 30(2), 390–395 (2012). https://doi.org/10.1097/HJH.0b013e32834f0451.
G. Jacquillet, R.J. Unwin, Physiological regulation of phosphate by vitamin D, parathyroid hormone (PTH) and phosphate (Pi). Pflug. Arch. 471(1), 83–98 (2019). https://doi.org/10.1007/s00424-018-2231-z
B. Zhang, A.T. Umbach, H. Chen, J. Yan, H. Fakhri, A. Fajol, M.S. Salker, D. Spichtig, A. Daryadel, C.A. Wagner, M. Föller, F. Lang, Up-regulation of FGF23 release by aldosterone. Biochem. Biophys. Res. Commun. 470(2), 384–390 (2016). https://doi.org/10.1016/j.bbrc.2016.01.034
N. Li, M. Wang, H. Wang, D. Zhang, X. Wang, F. Zu, G. Chang, K. Zhou, Prevalence of primary aldosteronism in hypertensive subjects with hyperglycemia. Clin. Exp. Hypertens. 35(3), 175–182 (2013). https://doi.org/10.3109/10641963.2012.712175
M. Tancredi, G. Johannsson, B. Eliasson, R. Eggertsen, U. Lindblad, S. Dahlqvist, H. Imberg, M. Lind, Prevalence of primary aldosteronism among patients with type 2 diabetes. Clin. Endocrinol. (Oxf.) 87(3), 233–241 (2017). https://doi.org/10.1111/cen.13370
Y. Hu, J. Zhang, W. Liu, X. Su, Determining the Prevalence of Primary Aldosteronism in Patients With New-Onset Type 2 Diabetes and Hypertension. J. Clin. Endocrinol. Metab. 105(4), dgz293 (2020). https://doi.org/10.1210/clinem/dgz293
W. Chen, F. Li, C. He, Y. Zhu, W. Tan, Elevated prevalence of abnormal glucose metabolism in patients with primary aldosteronism: a meta-analysis. Ir. J. Med. Sci. 183(2), 283–291 (2014). https://doi.org/10.1007/s11845-013-1007-x
C.H. Chang, Y.H. Hu, K.H. Huang, Y.H. Lin, Y.C. Tsai, C.H. Wu, S.Y. Yang, C.C. Chang, C.C. Lu, K.D. Wu, V.C. Wu, Higher Screening Aldosterone to Renin Ratio in Primary Aldosteronism Patients with Diabetes Mellitus. J. Clin. Med. 7(10), 360 (2018). https://doi.org/10.3390/jcm7100360
Acknowledgements
This study was feasible because of the support of our clinical PA team. We thank Dr. Ting Wu from the Hypertension Institute of Xinjiang for her assistance in endocrine monitoring.
Funding
This work was supported by the Non-profit Central Research Institute Fund of the Chinese Academy of Medical Sciences [Grant No. 2019PT330003].
Author information
Authors and Affiliations
Contributions
All authors have read and agreed to the final version of the paper. Conceptualization, N-f.L. and M-h.W.; Methodology, M-h.W., Q.L. and L.W.; Resources and data curation, L.W. and W-w.Z.; Writing—original draft preparation, M-h.W. and M.H.; Software, G-l.W. and L.W.; Project administration and funding acquisition, N-f.L.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, Mh., Li, Nf., Luo, Q. et al. Development and validation of a novel diagnostic nomogram model to predict primary aldosteronism in patients with hypertension. Endocrine 73, 682–692 (2021). https://doi.org/10.1007/s12020-021-02745-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-021-02745-7