Abstract
Background
Selenium (Se) and iodine (Io) are important micronutrients for the proper functioning of the thyroid gland, as they are crucial for the synthesis and activation of the thyroid hormones (TH) triiodothyronine (T3) and thyroxine (T4).
Objective
To evaluate the Se and Io nutritional status among schoolchildren.
Methodology
Cross-sectional, descriptive and analytical study conducted in 982 schoolchildren aged 6–14 years from public schools in the state of Bahia, Brazil. Sociodemographic and anthropometric variables, as well as urinary Se (USC) and Io concentrations (UIC) using the inductively coupled plasma mass spectrometry (ICP-MS) method and thyroid-stimulating hormone (TSH) from filter paper blood collection, were evaluated.
Results
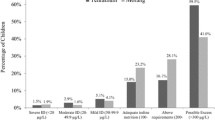
The median USC and UIC were 38.7 and 210.0 (IQR: 26.8–52.9 and 129.3–334.1 μg/L, respectively). The prevalence of iodine deficiency and excessive UIC were observed in 17.1% and 30.9% of schoolchildren, respectively. Concomitant low USC and IoD was found in 3.9% of schoolchildren. There was a positive correlation between USC and UIC (r = 0.60; p = 0.00). The median TSH was 0.95 (IQR: 0.69–1.30 µUI/L).
Conclusions
This study demonstrates that USC is a good biomarker for assessing Se status, meantime more studies are needed to establish cutoff USC in child population. Despite adequate median intake, a subgroup of schoolchildren had IoD and low USC. The correlation between UIC and USC point at the importance of two micronutrients, raising the question whether measuring Se should be included in monitoring programs that address the prevention of nutritional disturbances.



Similar content being viewed by others
Abbreviations
- UIC:
-
Urinary iodine concentration
- USC:
-
Urinary selenium concentration
- TH:
-
Thyroid hormones
- WHO:
-
World Health Organization
- IoD:
-
Iodine deficiency
- IDD:
-
Iodine deficiency disorder
- EII:
-
Excessive iodine intake
- SeD:
-
Selenium deficiency
- NIS:
-
Sodium-iodine symporter
- TSH:
-
Thyroid-stimulating hormone
References
S.M. O’Kane, M.S. Mulhern, L.K. Pourshahidi, J.J. Strain, A.J. Yeates, Micronutrients, iodine status and concentrations of thyroid hormones: a systematic review. Nutr. Rev. 76, 418–431 (2018)
WHO. World Health Organization. Trace elements in human nutrition and health. (Geneva, 1996). https://www.who.int/nutrition/publications/micronutrients/9241561734/en/. Accessed 20 June 2020.
WHO. World Health Organization. Organizacion Mundial de la Salud. Organizacion Panamericana de la Salud. Fondo de la Naciones Unidas para la Infancia. Consejo Internacional para la Lucha contra los Trantornos por Carencia de Yodo. Indicadores para evaluar los transtornos por carência de yodo y su control mediante la yodación de la sal. (Geneva, 1994). https://apps.who.int/iris/handle/10665/59446. Accessed 15 June 2020.
Brasil. Manual Técnico e Operacional do Pró-Iodo: Programa Nacional para a Prevenção e Controle dos Distúrbios por Deficiência de Iodo. Ministério da Saúde. (Brasília, 2007). http://189.28.128.100/dab/docs/portaldab/publicacoes/manual_iodo.pdf. Accessed 17 June 2020.
P.R. Larsen, A.M. Zavacki, The role of the iodothyronine deiodinases in the physiology and pathophysiology of thyroid hormone action. Eur. Thyroid. J. 1, 232–242 (2012)
R.O. Campos, I.S. Barreto, L.R.M. Jesus, S.C. Rebouças, T.L. Cerqueira, C.A. Oliveira et al. Iodine nutritional status in Brazil: a meta-analysis of all studies performed in the country pinpoints to an insufficient evaluation and heterogeneity. Arch. Endocrinol. Metab. 59, 13–22 (2015)
Brasil. Ministério da Saúde. Pesquisa Nacional para avaliação do impacto da iodação do sal (PNAISAL). (2016). http://189.28.128.100/dab/docs/portaldab/documentos/pnaisal_relatorio_final.pdf. Accessed 19 June 2020.
R.O. Campos, S.L. Rebouças, R. Beck, L.R.M. Jesus, Y.R. Ramos, I.S. Barreto et al. Iodine nutritional status in schoolchildren from public schools in Brazil: a cross-sectional study exposes association with socioeconomic factors and food insecurity. Thyroid 26, 972–979 (2016)
E. Zoidis, I. Seremelis, N. Kontopoulos, G.P. Danezis, Selenium-Dependent Antioxidant Enzymes: Actions and Properties of Selenoproteins. Antioxid. 7, 1–26 (2018)
M.B. Zimmermann, J: Köhrle, The impact of iron and selenium deficiencies on iodine and thyroid metabolism: biochemistry and relevance to public health. Thyroid 12, 867–878 (2002)
WHO. World Health Organization. United Nations Childrens Fund. International Council for the Control of Iodine Deficiency Disorders.: Assessment of iodine deficiency disorders and monitoring their elimination: a guide for programme managers. 3rd ed. (Geneva, 2007). https://www.who.int/nutrition/publications/micronutrients/iodine_deficiency/9789241595827/en/. Accessed 20 June 2020.
S.M. Hays, K. Macey, A. Nong, L.L. Aylward, Biomonitoring equivalents for selenium. Regul. Toxicol. Pharm. 70, 333–339 (2014)
D. Strich, S. Edri, D. Gillis, Current normal values for TSH and FT3 in children are too low: evidence from over 11.000 samples. JPEM 25, 245–248 (2012)
T. Çelik, N. Savaş, S. Kurtoğlu, Ö. Sangün, Z. Aydın, D. Mustafa et al. Iodine, copper, zinc, selenium and molybdenum levels in children aged between 6 and 12 years in the rural area with iodine deficiency and in the city center without iodine deficiency in Hatay. Turk. Pediatr. Ars 49, 111–116 (2014)
H. Skröder, M. Kippler, J. De Loma, R. Raqib, M. Vahter, Predictors of selenium biomarker kinetics in 4–9-year-old Bangladeshi children. Environ. Int. 121, 842–851 (2018)
I.B. Martens, B.R. Cardoso, D.J. Hare, M.M. Niedzwiecki, F.M. Lajolo, A. Martens, S.M. Cozzolino, Selenium status in preschool children receiving a Brazil nut–enriched diet. Nutrition 31, 1339–1343 (2015)
F.P. Phiri, E.L. Ander, R.M. Lark, E.H. Bailey, B. Chilima, J. Gondwe et al. Urine selenium concentration is a useful biomarker for assessing population level selenium status. Environ. Int 134, 105–218 (2019)
E. Khorasani, S.R. Mirhafez, S. Niroumand, Assessment of the Selenium Status in Hypothyroid Children from North East of Iran. J. Biol. Today’s World 6, 21–26 (2017)
P. Gać, N. Pawlas, R. Poręba, M. Poręba, I. Markiewicz-Górka, L. Januszewska, Z. Olszowy, K: Pawlas, Interaction between blood selenium concentration and a levels of oxidative stress and antioxidative capacity in healthy children. Environ. Toxicol. Pharmacol. 39, 137–144 (2015)
S.M. Hays, K. Macey, A. Nong, L.L. Aylward, Biomonitoring equivalents for selenium. Regul. Toxicol. Pharmacol. 70, 333–339 (2014)
C.D. Thomson, Assessment of requirements for selenium and adequacy of selenium status: a review. Eur. J. Clin. Nutr. 58, 391–402 (2004)
M. Santos, Y. Veneziani, A.L. Muccillo-Baisch, Da Silva Júnior, F.M.R.: Global survey of urinary selenium in children: a systematic review. J. Trace Elem. Med. Biol. 56, 1–5 (2019)
P. Milhoransa, R. Vanacor, Weber Furlanetto, T.: Intra- and interindividual iodine excretion in 24h in individuals in southern Brazil: a cross-sectional study. Ann. Nutr. Metab. 57, 260–264 (2010)
S. Andersen, J. Karmisholt, K.M. Pedersen, P. Laurberg, Reliability of studies of iodine intake and recommendations for number of samples in groups and in individuals. Br. J. Nutr. 99, 813–818 (2008)
D. Gashu, B.J. Stoecker, K. Bougma, A. Adish, G.D. Haki, G.S. Marquis, Stunting, selenium deficiency and anemia are associated with poor cognitive performance in preschool children from rural Ethiopia. Nutr. J. 15, 1–8 (2016)
H. El Bilali, C. Callenius, C. Strassner, L. Probst, Food and nutrition security and sustainability transitions in food systems. Food Energy Secur 8, 1–20 (2019)
K.H. Winther, M.P. Rayman, S.J. Bonnema, L. Hegedus, Selenium in thyroid disorders—essential knowledge for clinicians. Nat. Rev. Endocrinol. 16, 165–176 (2020)
M.B. Zimmermann, The role of iodine in human growth and development. Semin. Cell. Dev. Biol. 22, 645–652 (2011)
D. Gashu, G.S. Marquis, K. Bougma, B.J. Stoecker, Selenium inadequacy hampers thyroid response of young children after iodine repletion. J. Trace Elem. Med. Biol. 50, 291–295 (2018)
M. Kawai, Y. Shoji, S. Onuma, Y. Etani, S. Ida, Thyroid hormone status in patients with severe selenium deficiency. Clin. Pediatr. Endocrinol. 27, 67–74 (2018)
A.A. Tinkov, O.P. Ajsuvakova, T. Filippini, J.I.-Chang Zhou, XinGen Lei, E.R. Gatiatulina et al. Selenium and Selenoproteins in Adipose Tissue Physiology and Obesity. Biomolecules 10, 1–31 (2020)
S.F. Azab, S.H. Saleh, W.F. Elsaeed, M.A. Elshafie, L.M. Sherief, A.M. Esh et al. Serum trace elements in obese Egyptian children: a case–control study. Ital. J. Pediatr. 40, 1–7 (2014)
C. Tureck, G. Locateli, V.G. Corrêa, E.A. Koehnlein, Avaliação da ingestão de nutrientes antioxidantes pela população brasileira e sua relação com o estado nutricional. Rev. Bras. Epidemiol. J. 20, 30–42 (2017)
Funding
This study was supported by State of Bahia Research Foundation (FAPESB Edital 029/2012) grant (TOU PET0002/2013).
Author information
Authors and Affiliations
Contributions
RdeOC (data collection, USC and UIC analysis, anthropometric data and article writing), LMdeJ (data collection), DAM (USC and UIC analysis), WTdeSJ (USC and UIC analysis), VCdeOS (USC and UIC analysis), CAO (anthropometric data), FBJ (USC and UIC analysis), MM (text review), LH (text review) and HER (research coordinator and text review).
Corresponding author
Ethics declarations
Conflict of interest
The author declares no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Oliveira Campos, R., de Jesus, L.M., Morais, D.A. et al. Low urinary selenium levels are associated with iodine deficiency in Brazilian schoolchildren and adolescents. Endocrine 73, 609–616 (2021). https://doi.org/10.1007/s12020-021-02681-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-021-02681-6