Abstract
Purpose
Replicating the physiological cortisol secretion is key in the treatment of glucocorticoid insufficient individuals and optimization may enhance quality of life. The study investigates fatigue measured by ecological momentary assessments in patients treated with conventional hydrocortisone compared with once-daily dual-release hydrocortisone (Plenadren).
Methods
A 21-week open-label switch pilot trial included 30 patients with adrenal insufficiency due to hypopituitarism. Fatigue was assessed four times daily for 20 days using a momentary item version of the Multidimensional Fatigue Inventory on patients’ usual hydrocortisone regimen. Participants switched treatment to an identical daily dose of Plenadren for 16 weeks where fatigue assessments were repeated. Change in fatigue and diurnal variation of fatigue was analyzed using mixed models for repeated measurements.
Results
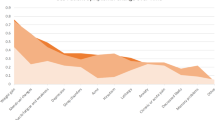
In four out of five fatigue subscales fatigue was significantly reduced 0.7–1.1 points (scales ranging from 4 to 20), when treated with Plenadren compared with conventional hydrocortisone, corresponding to small effect sizes below the scale-specific minimal important changes. However, 33% of the participants completing the study (9/27) experienced reductions in fatigue above the minimal important change. On Plenadren, we found larger between-person variances and smaller within-person variances. Finally, we identified diurnal fatigue curves for both treatments.
Conclusions
The Plenadren-related reduction in fatigue was significant but not necessarily of clinical importance when looking at a group level. However, there was a large interindividual variation in treatment effect, why patients with a large benefit in quality of life should be identified. Future RCTs should be powered to detect the effect magnitudes identified here.


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
References
H. Filipsson, J.P. Monson, M. Koltowska-Häggström, A. Mattsson, G. Johannsson, The impact of glucocorticoid replacement regimens on metabolic outcome and comorbidity in hypopituitary patients. J. Clin. Endocrinol. Metab. 91, 3954 (2006).
R. Giordano, S. Marzotti, M. Balbo, S. Romagnoli, E. Marinazzo, R. Berardelli, G. Migliaretti, A. Benso, A. Falorni, E. Ghigo, E. Arvat, Metabolic and cardiovascular profile in patients with Addison’s disease under conventional glucocorticoid replacement. J. Endocrinol. Investig. 32, 917 (2009).
L. Leelarathna, L. Breen, J.K. Powrie, S.M. Thomas, R. Guzder, B. McGowan, P.V. Carroll, Co-morbidities, management and clinical outcome of auto-immune Addison’s disease. Endocrine 38, 113 (2010).
J.W. Buning, M.Van. Faassen, P. Brummelman, R.P.F. Dullaart, G. Van Den Berg, M.M. Van Der Klauw, M.N. Kerstens, C.A. Stegeman, A.C.M. Kobold, I.P. Kema, B.H.R. Wolffenbuttel, A.P.Van. Beek, Effects of hydrocortisone on the regulation of blood pressure: results from a randomized controlled trial. J. Clin. Endocrinol. Metab. 101, 3691 (2016).
E. Charmandari, N.C. Nicolaides, G.P. Chrousos, Adrenal insufficiency. Lancet 383, 2152 (2014).
A. Mallappa, M. Debono, Endocrine development: workshop, Rome, October 2014. Endocr. Dev. 30, 42 (2016).
S.R. Bornstein, B. Allolio, W. Arlt, A. Barthel, A. Don-Wauchope, G.D. Hammer, E.S. Husebye, D.P. Merke, M.H. Murad, C.A. Stratakis, D.J. Torpy, Diagnosis and treatment of primary adrenal insufficiency: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 101, 364 (2016).
K. Løvås, J.H. Loge, E.S. Husebye, Subjective health status in Norwegian patients with Addison’s disease*: Subjective health status in Addison’s disease. Clin. Endocrinol. (Oxf.) 56, 581 (2002).
S. Hahner, M. Loeffler, M. Fassnacht, D. Weismann, A.C. Koschker, M. Quinkler, O. Decker, W. Arlt, B. Allolio, Impaired subjective health status in 256 patients with adrenal insufficiency on standard therapy based on cross-sectional analysis. J. Clin. Endocrinol. Metab. 92, 3912 (2007).
B. Bleicken, S. Hahner, M. Loeffler, M. Ventz, B. Allolio, M. Quinkler, Impaired subjective health status in chronic adrenal insufficiency: Impact of different glucocorticoid replacement regimens. Eur. J. Endocrinol. 159, 811 (2008).
B. Bleicken, S. Hahner, M. Loeffler, M. Ventz, O. Decker, B. Allolio, M. Quinkler, Influence of hydrocortisone dosage scheme on health-related quality of life in patients with adrenal insufficiency. Clin. Endocrinol. (Oxf.) 72, 297 (2010).
M. Forss, G. Batcheller, S. Skrtic, G. Johannsson, Current practice of glucocorticoid replacement therapy and patient-perceived health outcomes in adrenal insufficiency-a worldwide patient survey. BMC Endocr. Disord. 12, 8 (2012).
G. Johannsson, A.G. Nilsson, R. Bergthorsdottir, P. Burman, P. Dahlqvist, B. Ekman, B.E. Engström, T. Olsson, O. Ragnarsson, M. Ryberg, J. Wahlberg, B.M.K. Biller, J.P. Monson, P.M. Stewart, H. Lennernäs, S. Skrtic, Improved cortisol exposure-time profile and outcome in patients with adrenal insufficiency: a prospective randomized trial of a novel hydrocortisone dual-release formulation. J. Clin. Endocrinol. Metab. 97, 473 (2012).
V. Guarnotta, A. Ciresi, G. Pillitteri, C. Giordano, Improved insulin sensitivity and secretion in prediabetic patients with adrenal insufficiency on dual-release hydrocortisone treatment: a 36-month retrospective analysis. Clin. Endocrinol. (Oxf.). 88, 665 (2018).
V. Guarnotta, C. Di Stefano, A. Santoro, A. Ciresi, A. Coppola, C. Giordano, Dual-release hydrocortisone vs conventional glucocorticoids in adrenal insufficiency. Endocr. Connect. 8, 853 (2019).
R. Giordano, F. Guaraldi, E. Marinazzo, F. Fumarola, A. Rampino, R. Berardelli, I. Karamouzis, M. Lucchiari, T. Manetta, G. Mengozzi, E. Arvat, E. Ghigo, Improvement of anthropometric and metabolic parameters, and quality of life following treatment with dual-release hydrocortisone in patients with Addison’s disease. Endocrine 51, 360 (2016).
A.M. Isidori, M.A. Venneri, C. Graziadio, C. Simeoli, D. Fiore, V. Hasenmajer, E. Sbardella, D. Gianfrilli, C. Pozza, P. Pasqualetti, S. Morrone, A. Santoni, F. Naro, A. Colao, R. Pivonello, A. Lenzi, Effect of once-daily, modified-release hydrocortisone versus standard glucocorticoid therapy on metabolism and innate immunity in patients with adrenal insufficiency (DREAM): a single-blind, randomised controlled trial. Lancet Diabetes Endocrinol. 6, 173 (2018).
M. Quinkler, R.M. Nilsen, K. Zopf, M. Ventz, M. Øksnes, Modified-release hydrocortisone decreases BMI and HbA1c in patients with primary and secondary adrenal insufficiency. Eur. J. Endocrinol. 172, 619 (2015).
A.G. Nilsson, R. Bergthorsdottir, P. Burman, P. Dahlqvist, B. Ekman, B.E. Engström, O. Ragnarsson, S. Skrtic, J. Wahlberg, H. Achenbach, S. Uddin, C. Marelli, G. Johannsson, Long-Term safety of once-daily, dual-release hydrocortisone in patients with adrenal insufficiency: A phase 3b, open-label, extension study. Eur. J. Endocrinol. 176, 715 (2017).
F. Ceccato, E. Selmin, C. Sabbadin, M. Dalla Costa, G. Antonelli, M. Plebani, M. Barbot, C. Betterle, M. Boscaro, C. Scaroni, Improved salivary cortisol rhythm with dual-release hydrocortisone. Endocr. Connect. 7, 965 (2018).
M. Øksnes, S. Bensing, A.L. Hulting, O. Kam̈pe, A. Hackemann, G. Meyer, K. Badenhoop, C. Betterle, A. Parolo, R. Giordano, A. Falorni, L. Papierska, W. Jeske, A.A. Kasperlik-Zaluska, V.K.K. Chatterjee, E.S. Husebye, K. Løvas, Quality of life in European patients with Addison’s disease:Validity of the disease-specific questionnaire AddiQoL. J. Clin. Endocrinol. Metab. 97, 568 (2012).
A. Stone, S. Shiffman, A. Atienza, L. Nebeling, The science of real-time data capture: self-reports in health research (Oxford University Press, Oxford; 2007).
V.B. Boesen, U. Feldt-Rasmussen, J. Bue Bjorner, P. Cramon, M. Groenvold, B. Nygaard, Å.K. Rasmussen, T. Vilsbøll, T. Watt, How should thyroid-related quality of life be assessed? Recalled patient-reported outcomes compared to here-and-now measures. Thyroid 28, 1561 (2018).
P. Lorenz, L. Schindler, S. Steudte-Schmiedgen, K. Weidner, C. Kirschbaum, J. Schellong, Ecological momentary assessment in posttraumatic stress disorder and coping. An eHealth study protocol. Eur. J. Psychotraumatol. 10, 1654064 (2019)
P. Solk, K. Gavin, J. Fanning, W. Welch, G. Lloyd, A. Cottrell, A. Nielsen, C.A.Santa. Maria, W. Gradishar, S.A. Khan, S. Kulkarni, J. Siddique, S.M. Phillips, Feasibility and acceptability of intensive longitudinal data collection of activity and patient-reported outcomes during chemotherapy for breast cancer. Qual. Life Res 28, 3333 (2019).
M.J. Sliwinski, J.A. Mogle, J. Hyun, E. Munoz, J.M. Smyth, R.B. Lipton, Reliability and validity of ambulatory cognitive assessments. Assessment 25, 14 (2018).
S. Schneider, D.U. Junghaenel, F.J. Keefe, J.E. Schwartz, A.A. Stone, J.E. Broderick, Individual differences in the day-to-day variability of pain, fatigue, and well-being in patients with rheumatic disease: associations with psychological variables. Pain 153, 813 (2012).
V.B. Boesen, T. Christoffersen, T. Watt, S.W. Borresen, M. Klose, U. Feldt-Rasmussen, PlenadrEMA: effect of dual-release versus conventional hydrocortisone on fatigue, measured by ecological momentary assessments: a study protocol for an open-label switch pilot study. BMJ Open. 8, 19487 (2018).
E.M.A. Smets, B. Garssen, B. Bonke, J.C.J.M. De Haes, The multidimensional fatigue inventory (MFI) psychometric qualities of an instrument to assess fatigue. J. Psychosom. Res. 39, 315 (1995).
P. Cramon, Å.K. Rasmussen, S.J. Bonnema, J.B. Bjorner, U. Feldt-Rasmussen, M. Groenvold, L. Hegedüs, T. Watt, Development and implementation of PROgmatic: a clinical trial management system for pragmatic multi-centre trials, optimised for electronic data capture and patient-reported outcomes. Clin. Trials 11, 344 (2014).
J.D. Fisk, P.G. Ritvo, L. Ross, D.A. Haase, T.J. Marrie, W.F. Schlech, Measuring the functional impact of fatigue: initial validation of the fatigue impact scale. Clin. Infect. Dis. 18, 79 (1994).
J.E. Ware, C.D. Sherbourne, The MOS 36-ltem short-form health survey (SF-36): I. Conceptual framework and item selection. Med. Care 30, 473 (1992).
A. Purcell, J. Fleming, S. Bennett, B. Burmeister, T. Haines, Determining the minimal clinically important difference criteria for the multidimensional fatigue inventory in a radiotherapy population. Support. Care Cancer 18, 307 (2010).
J. Cohen, Statistical power analysis for the behavioral sciences (Taylor & Francis Inc, New York, 2013).
A.A. Stone, J.E. Schwartz, D. Schkade, N. Schwarz, A. Krueger, D. Kahneman, A population approach to the study of emotion: diurnal rhythms of a working day examined with the day reconstruction method. Emotion 6, 139 (2006).
Funding
This investigator-initiated research was supported by a grant (IST-DNK-000718) from Shire International GmbH, a member of the Takeda group of companies. The project emanated from the Department of Medical Endocrinology at Copenhagen University Hospital Rigshospitalet and the trial group assume responsibility for all aspects of the study. UFR’s research salary is sponsored by a grant from Novo Nordisk Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was performed in accordance with the Declarations of Helsinki and monitored by the Good Clinical Practice unit at Rigshospitalet. The study was approved by the Regional Scientific Ethical Committee in Copenhagen (ID: H-1-2014-073), the Danish Medicines Agency (ID: 2014070658), and the Danish Data Protection Agency (local identifier at Rigshospitalet: 30–1233). The study was registered at the EudraCT database (2014-002039-32). Informed consent was obtained from all individual participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Boesen, V.B., Borresen, S.W., Christoffersen, T. et al. The effect of dual-release versus conventional hydrocortisone on fatigue, measured by ecological momentary assessments. Endocrine 71, 467–475 (2021). https://doi.org/10.1007/s12020-020-02507-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-020-02507-x