Abstract
Purpose
Indicators to assess early liver damage and disease progression in nonalcoholic fatty liver disease (NAFLD) remain unsatisfactory. Albumin binding function has been reported to be an early indicator of liver damage in hepatitis and liver cirrhosis. However, its role in NAFLD patients is unknown.
Methods
An age/sex-matched, case-control study was performed. Albumin-binding capacity (ABiC) and albumin metal ion binding ability, assessed by ischemia modified albumin (IMA), were measured. Correlation analysis was performed to assess the association of albumin binding function with liver function enzymes and noninvasive liver fibrosis markers.
Results
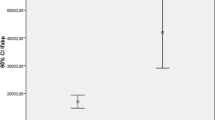
A total of 80 NAFLD patients and 41 healthy controls were included. Albumin binding function was significantly lower in NAFLD (ABiC: 196.00%, p < 0.001; IMA transformed (IMAT): 0.461, p < 0.001; and IMAT/albumin: 0.947 × 10−2, p < 0.001) than controls (ABiC: 211.00%; IMAT: 0.575; and IMAT/albumin: 1.206 × 10−2). Albumin binding function was also found to be significantly different among healthy participants and different severity groups of NAFLD (p < 0.001). Besides, albumin binding function showed positive correlation with BMI (ABiC: r = −0.247, p = 0.011; IMAT: r = −0.243, p = 0.013; IMAT/albumin: r = −0.254, p = 0.009) and FIB-4 index (ABiC: r = 0.230, p = 0.029). The ROC curve suggested that albumin binding function combined with BMI and triglyceride may predict the presence of NAFLD (area under ROC (AUROC) = 0.935, p < 0.001).
Conclusion
Our findings suggest albumin binding function is a novel biomarker for early liver damage and disease progression in NAFLD.



Similar content being viewed by others
References
Z. Younossi, Q.M. Anstee, M. Marietti, T. Hardy, L. Henry, M. Eslam, J. George, E. Bugianesi, Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat. Rev. Gastroenterol. Hepatol. 15(1), 11–20 (2018). https://doi.org/10.1038/nrgastro.2017.109
L.J. Alferink, J.C. Kiefte-de Jong, N.S. Erler, B.J. Veldt, J.D. Schoufour, R.J. de Knegt, M.A. Ikram, H.J. Metselaar, H. Janssen, O.H. Franco, S. Darwish Murad, Association of dietary macronutrient composition and non-alcoholic fatty liver disease in an ageing population: the Rotterdam Study. Gut 68(6), 1088–1098 (2019). https://doi.org/10.1136/gutjnl-2017-315940
F.M. Trovato, P. Castrogiovanni, L. Malatino, G.J.H.S. Musumeci, Nutrition: nonalcoholic fatty liver disease (NAFLD) prevention: role of Mediterranean diet and physical activity. Hepatobiliary Surg. Nutr. 8(2), 167–169 (2018). https://doi.org/10.21037/hbsn.2018.12.05
F. De Chiara, S. Heeboll, G. Marrone, C. Montoliu, S. Hamilton-Dutoit, A. Ferrandez, F. Andreola, K. Rombouts, H. Gronbaek, V. Felipo, J. Gracia-Sancho, R.P. Mookerjee, H. Vilstrup, R. Jalan, K.L. Thomsen, Urea cycle dysregulation in non-alcoholic fatty liver disease. J. Hepatol. 69(4), 905–915 (2018). https://doi.org/10.1016/j.jhep.2018.06.023
K. Thanapirom, E.A.J.H.S. Tsochatzis, Nutrition: non-alcoholic fatty liver disease (NAFLD) and the quest for effective treatments. Hepatobiliary Surg. Nutr. 8(1), 77–79 (2018). https://doi.org/10.21037/hbsn.2018.11.06
D. Sleep, Albumin and its application in drug delivery. Expert Opin. Drug Deliv. 12(5), 793–812 (2015). https://doi.org/10.1517/17425247.2015.993313
R. Garcia-Martinez, P. Caraceni, M. Bernardi, P. Gines, V. Arroyo, R. Jalan, Albumin: pathophysiologic basis of its role in the treatment of cirrhosis and its complications. Hepatology 58(5), 1836–1846 (2013). https://doi.org/10.1002/hep.26338
R. Jalan, M. Bernardi, Effective albumin concentration and cirrhosis mortality: from concept to reality. J. Hepatol. 59(5), 918–920 (2013). https://doi.org/10.1016/j.jhep.2013.08.001
L. Sun, H. Yin, M. Liu, G. Xu, X. Zhou, P. Ge, H. Yang, Y. Mao, Impaired albumin function: a novel potential indicator for liver function damage? Ann. Med. 51(7-8), 333–344 (2019). https://doi.org/10.1080/07853890.2019.1693056
E.A. Bormotova, T.V. Gupalova, The relationship between albumin-binding capacity of recombinant polypeptide and changes in the structure of albumin-binding domain. Bull. Exp. Biol. Med. 159(3), 393–397 (2015). https://doi.org/10.1007/s10517-015-2972-z
P. Ge, H. Yang, J. Lu, W. Liao, S. Du, Y. Xu, H. Xu, H. Zhao, X. Lu, X. Sang, S. Zhong, J. Huang, Y. Mao, Albumin binding function: the potential earliest indicator for liver function damage. Gastroenterol. Res. Pract. 2016, 5120760 (2016). https://doi.org/10.1155/2016/5120760
D. Roy, J.C. Kaski, Ischemia-modified albumin: the importance of oxidative stress. J. Am. Coll. Cardiol. 49(24), 2375–2376 (2007). https://doi.org/10.1016/j.jacc.2007.04.010 ; author reply 2376-2377
K. Oettl, R. Birner-Gruenberger, W. Spindelboeck, H.P. Stueger, L. Dorn, V. Stadlbauer, C. Putz-Bankuti, P. Krisper, I. Graziadei, W. Vogel, C. Lackner, R.E. Stauber, Oxidative albumin damage in chronic liver failure: relation to albumin binding capacity, liver dysfunction and survival. J. Hepatol. 59(5), 978–983 (2013). https://doi.org/10.1016/j.jhep.2013.06.013
R. Jalan, K. Schnurr, R.P. Mookerjee, S. Sen, L. Cheshire, S. Hodges, V. Muravsky, R. Williams, G. Matthes, N.A. Davies, Alterations in the functional capacity of albumin in patients with decompensated cirrhosis is associated with increased mortality. Hepatology 50(2), 555–564 (2009). https://doi.org/10.1002/hep.22913
G.C. Farrell, S. Chitturi, G.K. Lau, J.D. Sollano, Guidelines for the assessment and management of non-alcoholic fatty liver disease in the Asia-Pacific region: executive summary. J. Gastroenterol. Hepatol. 22(6), 775–777 (2007). https://doi.org/10.1111/j.1440-1746.2007.05002.x
M.D. Zeng, J.G. Fan, L.G. Lu, Y.M. Li, C.W. Chen, B.Y. Wang, Y.M. Mao, Guidelines for the diagnosis and treatment of nonalcoholic fatty liver diseases. J. Dig. Dis. 9(2), 108–112 (2008). https://doi.org/10.1111/j.1751-2980.2008.00331.x
E. Vilar-Gomez, N. Chalasani, Non-invasive assessment of non-alcoholic fatty liver disease: Clinical prediction rules and blood-based biomarkers. J. Hepatol. 68(2), 305–315 (2018). https://doi.org/10.1016/j.jhep.2017.11.013
S. Klammt, H.J. Wojak, A. Mitzner, S. Koball, J. Rychly, E.C. Reisinger, S. Mitzner, Albumin-binding capacity (ABiC) is reduced in patients with chronic kidney disease along with an accumulation of protein-bound uraemic toxins. Nephrol. Dial. Transpl. 27(6), 2377–2383 (2012). https://doi.org/10.1093/ndt/gfr616
M. Domenicali, M. Baldassarre, F.A. Giannone, M. Naldi, M. Mastroroberto, M. Biselli, M. Laggetta, D. Patrono, C. Bertucci, M. Bernardi, P. Caraceni, Posttranscriptional changes of serum albumin: clinical and prognostic significance in hospitalized patients with cirrhosis. Hepatology 60(6), 1851–1860 (2014). https://doi.org/10.1002/hep.27322
M. Maciazek-Jurczyk, A. Szkudlarek, M. Chudzik, J. Pozycka, A. Sulkowska, Alteration of human serum albumin binding properties induced by modifications: a review. Spectrochim. Acta Part A, Mol. Biomol. Spectrosc. 188, 675–683 (2018). https://doi.org/10.1016/j.saa.2017.05.023
M. Naldi, M. Baldassarre, M. Domenicali, M. Bartolini, P. Caraceni, Structural and functional integrity of human serum albumin: analytical approaches and clinical relevance in patients with liver cirrhosis. J. Pharm. Biomed. Anal. 144, 138–153 (2017). https://doi.org/10.1016/j.jpba.2017.04.023
M. Pawlak, P. Lefebvre, B. Staels, Molecular mechanism of PPARalpha action and its impact on lipid metabolism, inflammation and fibrosis in non-alcoholic fatty liver disease. J. Hepatol. 62(3), 720–733 (2015). https://doi.org/10.1016/j.jhep.2014.10.039
Acknowledgements
The authors appreciate the help of other teammates.
Author contributions
Y.M. and J.Z. proposed the study. L.S. and M.L. wrote the first manuscript. M.L. and H.Y. conducted the experiments. Q.W. and G.X. collected the data and performed the analysis. D.W., F.X. and B.J. made charts and illustrations. Y.J. helped with the methodology. H.Y., J.Z. and Y.M. revised the manuscript. All authors contributed to the design and interpretation of the study and to further drafts.
Funding
This work was funded by grants from CAMS Innovation Fund for Medical Sciences (CIFMS) (No.2016-I2M-1-001) and Tsinghua University-Peking Union Medical College Hospital Cooperation Project (PTQH201904552).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the Ethics Committee of Peking Union Medical College Hospital.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary material
Rights and permissions
About this article
Cite this article
Sun, L., Wang, Q., Liu, M. et al. Albumin binding function is a novel biomarker for early liver damage and disease progression in non-alcoholic fatty liver disease. Endocrine 69, 294–302 (2020). https://doi.org/10.1007/s12020-020-02319-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-020-02319-z