Abstract
Purpose
To comparatively assess the performance of three sonographic classification systems, American Thyroid Association (ATA), the American College of Radiology Thyroid Imaging Reporting and Data System (ACR TI-RADS), and American Association of Clinical Endocrinologists (AACE)/American College of Endocrinology (ACE)/Associazione Medici Endocrinologi (AME) in identifying malignant nodules in an elderly population.
Methods
Cross-sectional study of patients referred for fine needle aspiration biopsy in an academic center for the elderly. One nodule/patient was considered. Nodules classified Bethesda V/VI were considered malignant. Receiver operating characteristics (ROC) curves were established and compared to evaluate diagnostic performance. Malignancy among biopsies below the size cutoff for each ultrasound classification was also compared.
Results
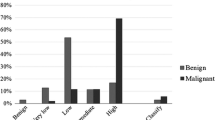
One thousand, eight hundred sixty-seven patients (92% females); median (Q1–Q3), age 71 (67–76) years, were studied showing 82.8% benign (Bethesda II) and 2.6% malignant cytology. The three classifications correctly identified malignancy (P < 0.01). Nonetheless, in the ATA and AACE/ACE/AME 16 and 2 malignant nodules, respectively, were unclassifiable. Including unclassified malignant nodules (n = 1234, malignant = 50), comparison of the ROC curves showed lower performance of ATA [area under the curve (AUC) = ATA (0.49) vs. ACR TI-RADS (0.62), p = 0.008 and ATA vs. AACE/ACE/AME (0.59), p = 0.022]. Proportion of below size cutoff biopsies for ATA, ACR TI-RADS, and AACE/ACE/AME was different [16, 42, and 29% (all p < 0.001)], but no differences in malignancy rate were observed in these nodules.
Conclusion
The present study is the first to validate in elderly patients these classifications showing that AACE/ACE/AME and ACR TI-RADS can predict thyroid malignancy more accurately than the ATA when unclassifiable malignant nodules are considered. Moreover, in this aged segment of the population, the use of ACR TI-RADS avoided more invasive procedures.

Similar content being viewed by others
References
C. Durante, G. Grani, L. Lamartina, S. Filetti, S.J. Mandel, D.S. Cooper, The diagnosis and management of thyroid nodules: a review. JAMA 319(9), 914–924 (2018). https://doi.org/10.1001/jama.2018.0898
C. Reiners, K. Wegscheider, H. Schicha, P. Theissen, R. Vaupel, R. Wrbitzky, P.M. Schumm-Draeger, Prevalence of thyroid disorders in the working population of Germany: ultrasonography screening in 96,278 unselected employees. Thyroid 14(11), 926–932 (2004). https://doi.org/10.1089/thy.2004.14.926
N. Kwong, M. Medici, T.E. Angell, X. Liu, E. Marqusee, E.S. Cibas, J.F. Krane, J.A. Barletta, M.I. Kim, P.R. Larsen, E.K. Alexander, The influence of patient age on thyroid nodule formation, multinodularity, and thyroid cancer risk. J. Clin. Endocrinol. Metab. 100(12), 4434–4440 (2015). https://doi.org/10.1210/jc.2015-3100
J.J. Diez,, Goiter in adult patients aged 55 years and older: etiology and clinical features in 634 patients. J. Gerontol. A Biol. Sci. Med. Sci. 60(7), 920–923 (2005). https://doi.org/10.1093/gerona/60.7.920
S. Sorrenti, E. Baldini, F. Tartaglia, A. Catania, S. Arcieri, D. Pironi, P.G. Calo, A. Filippini, S. Ulisse, Nodular thyroid disease in the elderly: novel molecular approaches for the diagnosis of malignancy. Aging Clin. Exp. Res. 29(Suppl 1), 7–13 (2017). https://doi.org/10.1007/s40520-016-0654-y
B.R. Haugen, E.K. Alexander, K.C. Bible, G.M. Doherty, S.J. Mandel, Y.E. Nikiforov, F. Pacini, G.W. Randolph, A.M. Sawka, M. Schlumberger, K.G. Schuff, S.I. Sherman, J.A. Sosa, D.L. Steward, R.M. Tuttle, L. Wartofsky, 2015 American Thyroid Association Management Guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association Guidelines Task Force on thyroid nodules and differentiated thyroid cancer. Thyroid 26(1), 1–133 (2016). https://doi.org/10.1089/thy.2015.0020
H. Gharib, E. Papini, J.R. Garber, D.S. Duick, R.M. Harrell, L. Hegedus, R. Paschke, R. Valcavi, P. Vitti, American Association of Clinical Endocrinologists, American College of Endocrinology, and Associazione Medici Endocrinologi Medical Guidelines for clinical practice for the diagnosis and management of thyroid nodules–2016 update. Endocr. Pract. 22(5), 622–639 (2016). https://doi.org/10.4158/EP161208.GL
F.N. Tessler, W.D. Middleton, E.G. Grant, J.K. Hoang, L.L. Berland, S.A. Teefey, J.J. Cronan, M.D. Beland, T.S. Desser, M.C. Frates, L.W. Hammers, U.M. Hamper, J.E. Langer, C.C. Reading, L.M. Scoutt, A.T. Stavros, ACR thyroid imaging, reporting and data system (TI-RADS): white paper of the ACR TI-RADS committee. J. Am. Coll. Radiol. 14(5), 587–595 (2017).https://doi.org/10.1016/j.jacr.2017.01.046
G. Grani, L. Lamartina, V. Cantisani, M. Maranghi, P. Lucia, C. Durante, Interobserver agreement of various thyroid imaging reporting and data systems. Endocr. Connect. 7(1), 1–7 (2018). https://doi.org/10.1530/EC-17-0336
E.S. Cibas, S.Z. Ali, The bethesda system for reporting thyroid cytopathology. Thyroid 19(11), 1159–1165 (2009). https://doi.org/10.1089/thy.2009.0274
G. Brenta, M. Schnitman, L. Bonnahon, S. Besuschio, C. Zuk, G. De Barrio, C. Peruzzotti, G. Saubidet, Evaluation of innovative skin-marking technique performed before thyroid ultrasound-guided fine-needle aspiration biopsies. Endocr. Pract. 8(1), 5–9 (2002). https://doi.org/10.4158/EP.8.1.5
E.R. DeLong, D.M. DeLong, D.L. Clarke-Pearson, Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44(3), 837–845 (1988)
X. Robin, N. Turck, A. Hainard, N. Tiberti, F. Lisacek, J.C. Sanchez, M. Muller, pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinform. 12, 77 (2011). https://doi.org/10.1186/1471-2105-12-77
Z. Wang, C.M. Vyas, O. Van Benschoten, M.A. Nehs, F.D. Moore Jr., E. Marqusee, J.F. Krane, M.I. Kim, H.T. Heller, A.A. Gawande, M.C. Frates, P.M. Doubilet, G.M. Doherty, N.L. Cho, E.S. Cibas, C.B. Benson, J.A. Barletta, A.M. Zavacki, P.R. Larsen, E.K. Alexander, T.E. Angell, Quantitative analysis of the benefits and risk of thyroid nodule evaluation in patients ≥70 years old. Thyroid 28(4), 465–471 (2018). https://doi.org/10.1089/thy.2017.0655
J.H. Yoon, H.S. Lee, E.K. Kim, H.J. Moon, J.Y. Kwak, Malignancy risk stratification of thyroid nodules: comparison between the thyroid imaging reporting and data system and the 2014 American Thyroid Association Management Guidelines. Radiology 278(3), 917–924 (2016). https://doi.org/10.1148/radiol.2015150056
A. Persichetti, E. Di Stasio, R. Guglielmi, G. Bizzarri, S. Taccogna, I. Misischi, F. Graziano, L. Petrucci, A. Bianchini, E. Papini, Predictive value of malignancy of thyroid nodule ultrasound classification systems: a prospective study. J. Clin. Endocrinol. Metab. 103(4), 1359–1368 (2018). https://doi.org/10.1210/jc.2017-01708
A. Lauria Pantano, E. Maddaloni, S.I. Briganti, G. Beretta Anguissola, E. Perrella, C. Taffon, A. Palermo, P. Pozzilli, S. Manfrini, A. Crescenzi, Differences between ATA, AACE/ACE/AME and ACR TI-RADS ultrasound classifications performance in identifying cytological high-risk thyroid nodules. Eur. J. Endocrinol. 178(6), 595–603 (2018). https://doi.org/10.1530/EJE-18-0083
M.I. Vera, T. Merono, M.A. Urrutia, C. Parisi, Y. Morosan, M. Rosmarin, M. Schnitman, F. Brites, S. Grisendi, M.S. Serrano, W. Luciani, L. Serrano, C. Zuk, G. De Barrio, C. Cejas, M.C. Faingold, G. Brenta, Differential profile of ultrasound findings associated with malignancy in mixed and solid thyroid nodules in an elderly female population. J. Thyroid Res. 2014, 761653 (2014). https://doi.org/10.1155/2014/761653
C. Shi, S. Li, T. Shi, B. Liu, C. Ding, H. Qin, Correlation between thyroid nodule calcification morphology on ultrasound and thyroid carcinoma. J. Int. Med. Res. 40(1), 350–357 (2012). https://doi.org/10.1177/147323001204000136
Z. Wang, H. Zhang, P. Zhang, L. He, W. Dong, Diagnostic value of ultrasound-detected calcification in thyroid nodules. Ann. Acad. Med. Singap. 43(2), 102–106 (2014)
G. Grani, L. Lamartina, V. Ascoli, D. Bosco, M. Biffoni, L. Giacomelli, M. Maranghi, R. Falcone, V. Ramundo, V. Cantisani, S. Filetti, C. Durante, Reducing the number of unnecessary thyroid biopsies while improving diagnostic accuracy: toward the “Right” TIRADS. J. Clin. Endocrinol. Metab. 104(1), 95–102 (2019). https://doi.org/10.1210/jc.2018-01674
T. Xu, Y. Wu, R.X. Wu, Y.Z. Zhang, J.Y. Gu, X.H. Ye, W. Tang, S.H. Xu, C. Liu, X.H. Wu, Validation and comparison of three newly-released thyroid imaging reporting and data systems for cancer risk determination. Endocrine 64(2), 299–307 (2019). https://doi.org/10.1007/s12020-018-1817-8
R.R. Tappouni, J.N. Itri, T.S. McQueen, N. Lalwani, J.J. Ou, ACR TI-RADS: pitfalls, solutions, and future directions. Radiographics 39(7), 2040–2052 (2019). https://doi.org/10.1148/rg.2019190026
Acknowledgements
To the technicians and fellows of the Radiology Department who assisted in filling out the US characteristics forms. We thank Dr. Pol Castellano Escuder for his support on ROC curve comparison and other statistical analyses.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary material
Rights and permissions
About this article
Cite this article
Di Fermo, F., Sforza, N., Rosmarin, M. et al. Comparison of different systems of ultrasound (US) risk stratification for malignancy in elderly patients with thyroid nodules. Real world experience. Endocrine 69, 331–338 (2020). https://doi.org/10.1007/s12020-020-02295-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-020-02295-4