Abstract
Background
Data on the prevalence and type of endocrine disorders in β-thalassemia intermedia (β-TI) patients are scarce. This multicenter study was designed to determine the prevalence of endocrine complications and the associated risk factors in a large group of β-TI patients.
Methods
In this cross-sectional multicenter study, 726 β-TI patients, aged 2.5–80 years, registered at 12 thalassemic centers, from nine countries, were enrolled during 2017. In a subgroup of 522 patients (mean age 30.8 ± 12.1; range: 2.5–80 years) from Qatar, Iran, Oman, Cyprus, and Jordan detailed data were available.
Results
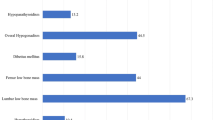
Overall, the most prevalent complications were osteopenia/osteoporosis (22.3%), hypogonadism (10.1%), and primary hypothyroidism (5.3%). In the subgroup multivariate analysis, older age was a risk factor for osteoporosis (Odds ratio: 7.870, 95% CI: 4.729–13.099, P < 0.001), hypogonadism (Odds ratio: 6.310, 95% CI: 2.944–13.521, P < 0.001), and non-insulin-dependent diabetes mellitus (NIDDM; Odds ratio: 17.67, 95% CI: 2.217–140.968, P = 0.007). Splenectomy was a risk factor for osteoporosis (Odds ratio: 1.736, 95% CI: 1.012–2.977, P = 0.045). Hydroxyurea was identified as a “protective factor” for NIDDM (Odds ratio: 0.259, 95% CI: 0.074–0.902, P = 0.034).
Conclusions
To the best of our knowledge, this is the largest cohort of β-TI patients with endocrine disorders evaluated in extremely heterogenic thalassemic populations for age, clinical, hematological, and molecular composition. The study demonstrates that endocrine complications are less common in patients with β-TI compared with β-TM patients. However, regular monitoring with timely diagnosis and proper management is crucial to prevent endocrine complications in β-TI patients.

Similar content being viewed by others
References
R. Galanello, R. Origa, Beta-thalassemia. Orphanet J. Rare Dis. 5(1), 11 (2010)
A. Taher, H. Isma’eel, M.D. Cappellini, Thalassemia intermedia: revisited. Blood Cells Molecules Dis. 37(1), 12–20 (2006)
K.M. Musallam, S. Rivella, E. Vichinsky, E.A. Rachmilewitz, Non-transfusion-dependent thalassemias. Haematologica 98(6), 833–844 (2013)
A. Taher, C. Hershko, M.D. Cappellini, Iron overload in thalassaemia intermedia: reassessment of iron chelation strategies. Br. J. Haematol. 147(5), 634–640 (2009)
M. Cappellini, A. Cohen, A. Eleftheriou, A. Piga, J. Porter, A. Taher, Guidelines for the Clinical Management of Thalassaemia. (Thalassaemia International Federation TIF, 2014)
M. Karimi, H. Darzi, M. Yavarian, Hematologic and clinical responses of thalassemia intermedia patients to hydroxyurea during 6 years of therapy in Iran. J. Pediatr. Hematol. Oncol. 27(7), 380–385 (2005)
P. Pootrakul, P. Sirankapracha, J. Sankote, U. Kachintorn, W. Maungsub, K. Sriphen, K. Thakernpol, K. Atisuk, S. Fucharoen, U. Chantraluksri, Clinical trial of deferiprone iron chelation therapy in β‐thalassaemia/haemoglobin E patients in Thailand. Br. J. Haematol. 122(2), 305–310 (2003)
R. Origa, R. Galanello, T. Ganz, N. Giagu, L. Maccioni, G. Faa, E. Nemeth, Liver iron concentrations and urinary hepcidin in β-thalassemia. Haematologica 92(5), 583–588 (2007)
H. Isma’eel, A.H. El Chafic, F. El Rassi, A. Inati, S. Koussa, R. Daher, W. Gharzuddin, S. Alam, A. Taher, Relation between iron-overload indices, cardiac echo-Doppler, and biochemical markers in thalassemia intermedia. Am. J. Cardiol. 102(3), 363–367 (2008)
A.T. Taher, K.M. Musallam, M. Karimi, A. El-Beshlawy, K. Belhoul, S. Daar, M.-S. Saned, A.-H. El-Chafic, M.R. Fasulo, M.D. Cappellini, Overview on practices in thalassemia intermedia management aiming for lowering complication rates across a region of endemicity: the OPTIMAL CARE study. Blood 115(10), 1886–1892 (2010)
A.U. Kurtoglu, E. Kurtoglu, A.K. Temizkan, Effect of iron overload on endocrinopathies in patients with beta-thalassaemia major and intermedia. Endokrynol. Pol. 63(4), 260–263 (2012)
M. Karimi, N. Cohan, V. De Sanctis, N.S. Mallat, A. Taher, Guidelines for diagnosis and management of Beta-thalassemia intermedia. Pediatr. Hematol. Oncol. 31(7), 583–596 (2014)
V. De Sanctis, C. Pintor, M. Gamberini, M. Ughi, A. Pinamonti, M. Aliquo, S. Anastasi, S. Andò, C. Brancati, M. Bruno, Multicentre study on prevalence of endocrine complications in thalassaemia major. Clin. Endocrinol. 42(6), 581–586 (1995)
S. Mohammadian, U. Bazrafshan, A. Sadeghi-Nejad, Endocrine gland abnormalities in thalassemia major: a brief review. J. Pediatr. Endocrinol. Metab. 16(7), 957–964 (2003)
P. De, R. Mistry, C. Wright, S. Pancham, W. Burbridge, K. Gangopadhayay, T. Pang, G. Das, A review of endocrine disorders in thalassaemia. Open J. Endocr. Metab. Dis. 4(02), 25 (2014)
V. De Sanctis, A.T. Soliman, H. Elsedfy, N. Skordis, C. Kattamis, M. Angastiniotis, M. Karimi, M.A.D.M. Yassin, A. El Awwa, I. Stoeva, Growth and endocrine disorders in thalassemia: the international network on endocrine complications in thalassemia (I-CET) position statement and guidelines. Indian J. Endocrinol. Metab. 17(1), 8 (2013)
N. Perera, N. Lau, S. Mathews, C. Waite, P. Ho, I. Caterson, Overview of endocrinopathies associated with β-thalassaemia major. Intern. Med. J. 40(10), 689–696 (2010)
A.T. Taher, K.M. Musallam, M.D. Cappellini, Thalassaemia intermedia: an update. Mediterr. J. Hematol. Infect. Dis. 1(1), e2009004 (2009)
Writing Group for the ISCD Position, Development Conference: indications and reporting for dual-energy x-ray absorptiometry. J. Clin. Densitom. 7(1), 37–44 (2004)
S.M. Petak, H. Nankin, R. Spark, R. Swerdloff, L. Rodriguez-Rigau, American Association of Clinical Endocrinologists Medical Guidelines for clinical practice for the evaluation and treatment of hypogonadism in adult male patients-2002 update. Endocr. Pract. 8(6), 440–456 (2002)
D.M. Nathan, J.B. Buse, M.B. Davidson, E. Ferrannini, R.R. Holman, R. Sherwin, B. Zinman, Medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 32(1), 193–203 (2009)
N.E. Cusano, N.M. Maalouf, P.Y. Wang, C. Zhang, S.C. Cremers, E.M. Haney, D.C. Bauer, E.S. Orwoll, J.P. Bilezikian, Normocalcemic hyperparathyroidism and hypoparathyroidism in two community-based nonreferral populations. J. Clin. Endocrinol. Metab. 98(7), 2734–2741 (2013)
B.B. Bercu, D. Shulman, A.W. Root, B.E. Spiliotis, Growth hormone (GH) provocative testing frequently does not reflect endogenous GH secretion. J. Clin. Endocrinol. Metab. 63(3), 709–716 (1986)
M.A. Yialamas, F.J. Hayes, Androgens and the ageing male and female. Best Pract. Res. Clin. Endocrinol. Metabol. 17(2), 223–236 (2003)
E.B. Fung, P.R. Harmatz, P.D. Lee, M. Milet, R. Bellevue, M.R. Jeng, K.A. Kalinyak, M. Hudes, S. Bhatia, E.P. Vichinsky, Increased prevalence of iron‐overload associated endocrinopathy in thalassaemia versus sickle‐cell disease. Br. J. Haematol. 135(4), 574–582 (2006)
C. Vullo, V. Sanctis, M. Katz, B. Wonke, A. Hoffbrand, B. Bagni, T. Torresani, G. Tolis, M. Masiero, A. Palma, Endocrine abnormalities in thalassemia. Ann. N. Y. Acad. Sci. 612(1), 293–310 (1990)
V. De Sanctis, A.T. Soliman, D. Canatan, H. Elsedfy, M. Karimi, S. Daar, H. Rimawi, S. Christou, N. Skordis, P. Tzoulis, An ICET—a survey on hypoparathyroidism in patients with thalassaemia major and intermedia: a preliminary report. Acta Bio Med. Atenei Parmensis 88(4), 435–444 (2017)
I. Kanbour, P, Chandra, A. Soliman, V. De Sanctis, A. Nashwan, S. Abusamaan, A. Moustafa, M.A. Yassin, Severe liver iron concentrations (LIC) in 24 patients with β-thalassemia major: correlations with serum ferritin, liver enzymes and endocrine complications. Mediterr. J. Hematol. Infect. Dis. 10(1), e2018062 (2018)
Z, Majd, S, Haghpanah, G.H. Ajami, S. Matin, H. Namazi, M. Bardestani, M. Karimi, Serum ferritin levels correlation with heart and liver MRI and LIC in patients with transfusion-dependent thalassemia. Iran. Red Crescent Med. J. 17(4), e24959 (2015)
A.T. Taher, J.B. Porter, V. Viprakasit, A. Kattamis, S. Chuncharunee, P. Sutcharitchan, N. Siritanaratkul, R. Galanello, Z. Karakas, T. Lawniczek, Deferasirox effectively reduces iron overload in non-transfusion-dependent thalassemia (NTDT) patients: 1-year extension results from the THALASSA study. Ann. Hematol. 92(11), 1485–1493 (2013)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The protocol of the study was approved by Shiraz University of Medical Sciences (Approval code: 1396-01-32-15525).
Informed consent
Written informed consent was obtained from the patients or their parents or legal guardian before participation in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Karimi, M., Zarei, T., Haghpanah, S. et al. Evaluation of endocrine complications in beta-thalassemia intermedia (β-TI): a cross-sectional multicenter study. Endocrine 69, 220–227 (2020). https://doi.org/10.1007/s12020-019-02159-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-019-02159-6