Abstract
Objective
Although the focus of acromegaly treatment is the hormonal control of the disease, a new perspective must be given to the functional rehabilitation of these patients, especially when considering the recent increase in survival. The aim of this study was to evaluate the effects of therapist-oriented home rehabilitation (TOHR) on patients with acromegaly.
Patients and methods
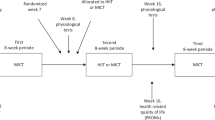
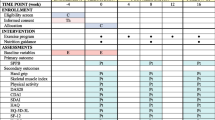
Seventeen adults with acromegaly followed an exercise programme from a booklet with instructions for each exercise prescribed, for 2 months, and were reassessed after 1 month of washout. At each of the 3 timepoints (before and after the intervention and at the 1-month follow-up), the participants were subjected to the following assessments: body composition through bioimpedance, health-related quality of life (HRQoL) using the Acromegaly Quality of Life (AcroQoL) questionnaire, general fatigue through the Functional Assessment of Chronic Illness Therapy-Fatigue scale, handgrip strength, lower extremity functionality using isometric dynamometry and the Lower Extremity Functional Scale (LEFS), body balance through stabilometry, and functional capacity through 6-minute walking distance (6MWD).
Results
After performing TOHR, improvements in general fatigue, quadriceps muscle strength, LEFS, 6MWD, balance control and all AcroQoL dimensions were observed (all P < 0.05). After 1 month of washout, however, these gains were lost for all parameters, except the LEFS and balance control.
Conclusions
In acromegaly, TOHR results in improvements in muscle function, functional capacity, general fatigue, body balance, and HRQoL. Large randomized controlled trials are needed to replicate these benefits and to recommend rehabilitation, especially for those with long-term illness.

Similar content being viewed by others
References
A. Lavrentaki, A. Paluzzi, J.A. Wass, N. Karavitaki, Epidemiology of acromegaly: review of population studies. Pituitary 20, 4–9 (2017)
F. Bolfi, A.F. Neves, C.L. Boguszewski, V.S. Nunes-Nogueira, Mortality in acromegaly decreased in the last decade: a systematic review and meta-analysis. Eur. J. Endocrinol. 179, 59–71 (2018)
M.R. Gadelha, L. Kasuki, D.S.T. Lim, M. Fleseriu, Systemic complications of acromegaly and the impact of the current treatment landscape: an update. Endocr. Rev. 40, 268–332 (2019)
S. AlDallal, Acromegaly: a challenging condition to diagnose. Int. J. Gen. Med. 11, 337–343 (2018)
M.J. Wassenaar, N.R. Biermasz, M. Kloppenburg, A.A. van der Klaauw, J. Tiemensma, J.W. Smit, A.M. Pereira, F. Roelfsema, H.M. Kroon, J.A. Romijn, Clinical osteoarthritis predicts physical and psychological QoL in acromegaly patients. Growth Horm. IGF Res. 20, 226–233 (2010)
A.J. Lopes, D.P. da Silva, L. Kasuki, M.R. Gadelha, G.B. Camilo, F.S. Guimarães, Posture and balance control in patients with acromegaly: results of a cross-sectional study. Gait Posture 40, 154–159 (2014)
T.S. Homem, F.S. Guimarães, M.S. Soares, L. Kasuki, M.R. Gadelha, A.J. Lopes, Balance control and peripheral muscle function in aging: a comparison between individuals with acromegaly and healthy subjects. J. Aging Phys. Act. 25, 218–227 (2017)
E. Hatipoglu, N. Topsakal, O.E. Atilgan, N. Alcalar, A.F. Camliguney, M. Niyazoglu, Impact of exercise on quality of life and body-self perception of patients with acromegaly. Pituitary 17, 38–43 (2014)
E. Hatipoglu, N. Topsakal, O. Erkut Atilgan, A.F. Camliguney, B. Ikitimur, S. Ugurlu, M. Niyazoglu, H.B. Cotuk, P. Kadioglu, Physical and cardiovascular performance in cases with acromegaly after regular short-term exercise. Clin. Endocrinol. 83, 91–97 (2015)
L. Katznelson, E.R. Laws Jr, S. Melmed, M.E. Molitch, M.H. Murad, A. Utz, J.A. Wass; Endocrine Society, Acromegaly: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 99, 3933–3951 (2014)
S. Matsudo, T. Araújo, V. Matsudo, D. Andrade, E. Andrade, L.C. Oliveira, G. Braggion, International physical activity questionnaire (IPAQ): study of validity and reliability in Brazil. Ativ. FíSci. Saúde. 6, 5–18 (2001)
J.A. Alison, Z.J. McKeough, Pulmonary rehabilitation for COPD: are programs with minimal exercise equipment effective? J. Thorac. Dis. 6, 1606–1614 (2014)
J. Baltich, C.A. Emery, D. Stefanyshyn, B.M. Nigg, The effects of isolated ankle strengthening and functional balance training on strength, running mechanics, postural control and injury prevention in novice runners: design of a randomized controlled trial. BMC Musculoskelet. Disord. 15, 407 (2014)
L. Ganderton, S. Jenkins, K. Gain, R. Fowler, P. Winship, D. Lunt, E. Gabbay, Short term effects of exercise training on exercise capacity and quality of life in patients with pulmonary arterial hypertension: protocol for a randomised controlled trial. BMC Pulm. Med. 23, 11–25 (2011)
M.N. Rodrigues, S.C. Silva, W.D. Monteiro, P.T.V. Farinatti, Comparison of body fat estimation by bioelectric impedance, skinfold thickness, and underwater weighing. Rev. Bras. Med. Esport. 7, 125–131 (2001)
S.M. Webb, X. Badia, N.L. Surinach, Validity and clinical applicability of the acromegaly quality of life questionnaire, AcroQoL: a 6-month prospective study. Eur. J. Endocrinol. 155, 269–277 (2006)
C.E. Mosher, K.N. Duhamel, An examination of distress, sleep, and fatigue in metastatic breast cancer patients. Psychooncology 21, 100–107 (2012)
T.R.L. Lima, L. Kasuki, M.R. Gadelha, A.J. Lopes, The effectiveness of a therapist-oriented home rehabilitation program for a patient with acromegaly: a case study. J. Bodyw. Mov. Ther. (2019) https://doi.org/10.1016/j.jbmt.2019.01.006
C.A. Crosby, M.A. Wehbe, B. Mawr, Hand strength: normative values. J. Hand. Surg. Am. 19, 665–670 (1994)
A.S. Ferreira, F.S. Guimarães, J.G. Silva, Aspectos metodológicos da eletromiografia de superfície: considerações sobre os sinais e processamentos para estudo da função neuromuscular. Rev. Bras. Cienc. Esport. 31, 11–30 (2010)
J.C. Ferreira, C.M. Patino, Randomization: beyond tossing a coin. J. Bras. Pneumol. 42, 310 (2016)
T.R. Lima, F.S. Guimarães, R.S. Neves, S.L. Menezes, A.J. Lopes, Scleroderma: assessment of posture, balance and pulmonary function in a cross-sectional controlled study. Clin. Biomech. 30, 438–443 (2015)
R.R. Britto, V.S. Probst, A.F. de Andrade, G.A. Samora, N.A. Hernandes, P.E. Marinho, M. Karsten, F. Pitta, V.F. Parreira, Reference equations for the six-minute walk distance based on a Brazilian multicenter study. Braz. J. Phys. Ther. 17, 556–563 (2013)
L.J. Woodhouse, A. Mukherjee, S.M. Shalet, S. Ezzat, The influence of growth hormone status on physical impairments, functional limitations, and health-related quality of life in adults. Endocr. Rev. 27, 287–317 (2006)
J. Tiemensma, A.A. Kaptein, A.M. Pereira, J.W. Smit, J.A. Romijn, N.R. Biermasz, Affected illness perceptions and the association with impaired quality of life in patients with long-term remission of acromegaly. J. Clin. Endocrinol. Metab. 96, 3550–3558 (2011)
N. Kyriakakis, J. Lynch, S.G. Gilbey, S.M. Webb, R.D. Murray, Impaired quality of life in patients with treated acromegaly despite long-term biochemically stable disease: Results from a 5-years prospective study. Clin. Endocrinol. 86, 806–815 (2017)
E. Solomon, D. Brănișteanu, A. Dumbravă, R.G. Solomon, L. Kiss, M. Glod, C. Preda, Executive functioning and quality of life in acromegaly. Psychol. Res. Behav. Manag. 12, 39–44 (2019)
X. Guo, L. Gao, X. Shi, H. Li, Q. Wang, Z. Wang, W. Chen, B. Xing, Pre- and postoperative body composition and metabolic characteristics in patients with acromegaly: a prospective study. Int. J. Endocrinol. 2018, 4125013 (2018)
E.M. Walchan, F.S. Guimarães, M.S. Soares, L. Kasuki, M.R. Gadelha, A.J. Lopes, Parameters of knee isokinetic dynamometry in individuals with acromegaly: association with growth hormone levels and general fatigue. Isokinet. Exerc. Sci. 24, 331–340 (2016)
L. Füchtbauer, D.S. Olsson, B.Å. Bengtsson, L.L. Norrman, K.S. Sunnerhagen, G. Johannsson, Muscle strength in patients with acromegaly at diagnosis and during long-term follow-up. Eur. J. Endocrinol. 177, 217–226 (2017)
J.B. Pickett, R.B. Layzer, S.R. Levin, V. Scheider, M.J. Campbell, A.J. Sumner, Neuromuscular complications of acromegaly. Neurology 1975 25, 638–645 (1975)
D.P. Guedes da Silva, F.S. Guimarães, C.M. Dias, A. Guimarães Sde, L. Kasuki, M.R. Gadelha, G.B. Camilo, A.J. Lopes, On the functional capacity and quality of life of patients with acromegaly: are they candidates for rehabilitation programs? J. Phys. Ther. Sci. 25, 1497–1501 (2013)
M.D. Smith, A.T. Chang, H.E. Seale, J.R. Walsh, P.W. Hodges, Balance is impaired in people with chronic obstructive pulmonary disease. Gait Posture 31, 456–460 (2010)
I. Crespo, S.M. Webb, Perception of health and cognitive dysfunction in acromegaly patients. Endocrine 46, 365–367 (2014)
A.J. Lopes, D.P. Guedes da Silva, S. Ferreira Ade, L. Kasuki, M.R. Gadelha, F.S. Guimarães, FS, What is the effect of peripheral muscle fatigue, pulmonary function, and body composition on functional exercise capacity in acromegalic patients? J. Phys. Ther. Sci. 27, 719–724 (2015)
A. Colao, D. Ferone, P. Marzullo, G. Lombardi, Systemic complications of acromegaly: epidemiology, pathogenesis, and management. Endocr. Rev. 25, 102–152 (2004)
S.G. Thomas, L.J. Woodhouse, S.M. Pagura, S. Ezzat, Ventilation threshold as a measure of impaired physical performance in adults with growth hormone excess. Clin. Endocrinol. 56, 351–358 (2002)
A.M. Pereira, J. Tiemensma, J.A. Romijn, N.R. Biermasz, Cognitive impairment and psychopathology in patients with pituitary diseases. Neth. J. Med. 70, 255–260 (2012)
C.L. Coulter, J.M. Scarvell, T.M. Neeman, P.N. Smith, Physiotherapist-directed rehabilitation exercises in the outpatient or home setting improve strength, gait speed and cadence after elective total hip replacement: a systematic review. J. Physiother. 59, 219–226 (2013)
J.J. Kraal, M.E. Van den Akker-Van Marle, A. Abu-Hanna, W. Stut, N. Peek, H.M. Kemps, Clinical and cost-effectiveness of home-based cardiac rehabilitation compared to conventional, centre-based cardiac rehabilitation: results of the FIT@Home study. Eur. J. Prev. Cardiol. 24, 1260–1273 (2017)
Acknowledgements
The authors thank the participants for their continuing participation in this research effort.
Funding
This study was funded by the Conselho Brasileiro de Desenvolvimento Científico e Tecnológico (grant number 304625/2016-7), the Fundação Carlos Chagas Filho de Amparo à Pesquisa do Estado do Rio de Janeiro (grant number E-26/202.679/2018), and the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (Finance Code 001).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in this study.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
About this article
Cite this article
Lima, T.R.L., Kasuki, L., Gadelha, M. et al. Physical exercise improves functional capacity and quality of life in patients with acromegaly: a 12-week follow-up study. Endocrine 66, 301–309 (2019). https://doi.org/10.1007/s12020-019-02011-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-019-02011-x