Abstract
Purpose
The management of small (≤5 mm) rectal neuroendocrine neoplasms (r-NENs), incidentally removed during colonoscopy, still remains under debate.
Methods
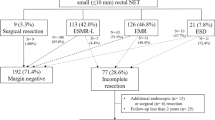
All consecutive patients affected by r-NENs from January 2013 to December 2017 were studied. The inclusion criteria were: (1) patients having an incidental pathological diagnosis of very small (≤5 mm) polypoid r-NENs; (2) patients treated with a standard polypectomy as first-line therapy and (3) patients treated by endoscopic submucosal dissection (ESD) as salvage therapy. The primary endpoint was to identify the factors related to residual disease after a standard polypectomy. The secondary endpoint was to calculate the accuracy of endoscopic ultrasound (EUS), grading and size in predicting residual disease.
Results
Starting from a prospective database of 123 consecutive patients affected by r-NENs, only 31 met the inclusion criteria. A final pathological examination of an ESD specimen showed residual disease in 7 out of 31 patients (22.6%). A multivariate analysis showed that the size of the polyps was the only independent factor related to residual disease with an odds ratio of 8.7 ± 7.5 (P = 0.013) for each millimetre. The accuracy of EUS, grading and tumour size (3.1 mm cut-off point) and area under the curves were 0.661 ± 0.111, 0.631 ± 0.109 and 0.821 ± 0.109, respectively.
Conclusions
When the r-NEN polyp was larger than 3 mm, ESD was indicated. Unlike the size of the tumour, grading and EUS features did not accurately predict residual disease.



Similar content being viewed by others
References
J.C. Yao, M. Hassan, A. Phan et al. One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumours in 35,825 cases in the United States. J. Clin. Oncol. 20, 3063–3072 (2008)
J.K. Ramage, W.W. De Herder, G. Delle Fave et al. Vienna Consensus Conference participants. ENETS Consensus Guidelines Update for Colorectal Neuroendocrine Neoplasms. Neuroendocrinology 103, 139–143 (2016)
K.O. Shebani, W.W. Souba, D.M. Finkelstein et al. Prognosis and survival in patients with gastrointestinal tract carcinoid tumours. Ann Surg 229, 815–821 (1999)
J. Wu, R. Srirajaskanthan, J. Ramage, Rectal neuroendocrine tumor. Dig. Endosc. 26, 532–533 (2014)
WHO, in Classification of Tumours of Endocrine Organs, 4th edn, ed. R.V. Lloyd, R.Y. Osamura, G. Kloppel, J. Rosai (IARC Press, Lyon, 2017), p 238.
L.H. Tang, M. Gonen, C. Hedvat et al. Objective quantification of the Ki67 proliferative index in neuroendocrine tumours of the gastroenteropancreatic system: a comparison of digital image analysis with manual methods. Am. J. Surg. Pathol. 36, 1761–1770 (2012)
C.Z. Mooney, R.D. Duval, Bootstrapping: A Non-Parametric Approach to Statistical Inference (Sage Publications, Newbury Park, CA, 1993).
M. Ferlitsch, A. Moss, C. Hassan et al. Colorectal polypectomy and endoscopic mucosal resection (EMR): European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 49, 270–297 (2017)
S. Chablaney, Z.A. Zator, N.A. Kumta, Diagnosis and management of rectal neuroendocrine tumours. Clin. Endosc. 50, 530–536 (2017)
J. Kim, J.H. Kim, J.Y. Lee et al. Clinical outcomes of endoscopic mucosal resection for rectal neuroendocrine tumor. BMC Gastroenterol. 18, 77 (2018)
H. So, S.H. Yoo, S. Han et al. Efficacy of precut endoscopic mucosal resection for treatment of rectal neuroendocrine tumors. Clin. Endosc. 50, 585–591 (2017)
H.W. Park, J.S. Byeon, Y.S. Park et al. Endoscopic submucosal dissection for treatment of rectal carcinoid tumours. Gastrointest. Endosc. 72, 143–149 (2010)
D.S. Lee, S.W. Jeon, S.Y. Park et al. The feasibility of endoscopic submucosal dissection for rectal carcinoid tumours: comparison with endoscopic mucosal resection. Endoscopy 42, 647–651 (2010)
X. Serra-Aracil, A. Pallisera-Lloveras, L. Mora-Lopez et al. Transanal endoscopic surgery is effective and safe after endoscopic polypectomy of potentially malignant rectal polyps with questionable margins. Colorectal Dis. 20, 789–796 (2018)
F. Nakamura, Y. Saito, S. Haruyama et al. Short-term prospective questionnaire study of early postoperative quality of life after colorectal endoscopic submucosal+ dissection. Dig. Dis. Sci. 62, 3325–3335 (2017)
A. Repici, N. Pagano, C. Hassan et al. Balanced propofol sedation administered by nonanesthesiologists: The first Italian experience. World J. Gastroenterol. 17, 3818–3823 (2011)
J. Carpenter, J. Bithell, M.B. Swift, Bootstrap confidence intervals (when, which, what? A practical guide for medical statisticians). Stat Med. 19, 1141–1164 (2000)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee, and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Pagano, N., Ricci, C., Brighi, N. et al. Incidental diagnosis of very small rectal neuroendocrine neoplasms: when should endoscopic submucosal dissection be performed? A single ENETS centre experience. Endocrine 65, 207–212 (2019). https://doi.org/10.1007/s12020-019-01907-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-019-01907-y