Abstract
Purpose
Serum thyroid-stimulating hormone level was influenced by several factors, including age, gender, thyroid auto-antibodies, race, and intake of dietary iodine. We evaluated age-specific reference interval of serum thyroid-stimulating hormone levels in Korea, an iodine excess area.
Methods
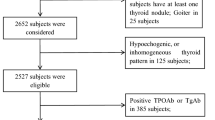
This nationwide population-based cross-sectional study included representative civilian, non-institutional population (n = 6564) who underwent thyroid function tests from Korea National Health and Nutrition Examination Survey VI (2013–2015). The reference interval of serum thyroid-stimulating hormone levels was defined between the 2.5th and 97.5th percentiles in the reference population.
Results
The geometric mean of serum thyroid-stimulating hormone levels in the reference population was 2.17 mIU/L with a reference interval of 0.62–6.84 mIU/L. In the reference population, the geometric mean of serum TSH levels in each age group of 10–18, 19–29, 30–39, 40–49, 50–59, 60–69, and equal or older than 70 years was 2.47, 2.20, 2.07, 2.04, 2.23, 2.12, and 2.27 mIU/L, with a reference interval of 0.74–7.35, 0.67–6.42, 0.63–6.04, 0.62–6.20, 0.56–7.37, 0.57–6.90, and 0.42–6.58 mIU/L, respectively. In the reference population, the urinary iodine concentrations were consistently high in all age groups (median 298.5 μg/L). Subjects aged 10–18 years had the highest urinary iodine concentrations.
Conclusions
There was no shift toward higher levels with age in the distribution of serum thyroid-stimulating hormone levels. The reference interval of serum thyroid-stimulating hormone levels was consistently high in all age group, especially from adolescence 10–18 years in a Korean population who had excessive intake of dietary iodine.



Similar content being viewed by others
References
D.S. Cooper, Subclinical hypothyroidism. JAMA 258, 246–247 (1987)
M. Kim, T.Y. Kim, S.H. Kim, Y. Lee, S.Y. Park, H.D. Kim, H. Kwon, Y.M. Choi, E.K. Jang, M.J. Jeon, W.G. Kim, Y.K. Shong, W.B. Kim, Reference interval for thyrotropin in a ultrasonography screened Korean population. Korean J. Intern. Med. 30, 335–344 (2015)
J.G. Hollowell, N.W. Staehling, W.D. Flanders, W.H. Hannon, E.W. Gunter, C.A. Spencer, L.E. Braverman, Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): national health and nutrition examination survey (NHANES III). J. Clin. Endocrinol. Metab. 87, 489–499 (2002)
M.I. Surks, J.G. Hollowell, Age-specific distribution of serum thyrotropin and antithyroid antibodies in the US population: implications for the prevalence of subclinical hypothyroidism. J. Clin. Endocrinol. Metab. 92, 4575–4582 (2007)
C. Sriphrapradang, S. Pavarangkoon, W. Jongjaroenprasert, L.O. Chailurkit, B. Ongphiphadhanakul, W. Aekplakorn, Reference ranges of serum TSH, FT4 and thyroid autoantibodies in the Thai population: the national health examination survey. Clin. Endocrinol. 80, 751–756 (2014)
T. Vadiveloo, P.T. Donnan, M.J. Murphy, G.P. Leese, Age- and gender-specific TSH reference intervals in people with no obvious thyroid disease in Tayside, Scotland: the thyroid epidemiology, audit, and research study (TEARS). J. Clin. Endocrinol. Metab. 98, 1147–1153 (2013)
T.E. Hamilton, S. Davis, L. Onstad, K.J. Kopecky, Thyrotropin levels in a population with no clinical, autoantibody, or ultrasonographic evidence of thyroid disease: implications for the diagnosis of subclinical hypothyroidism. J. Clin. Endocrinol. Metab. 93, 1224–1230 (2008)
K.M. Kahapola-Arachchige, N. Hadlow, R. Wardrop, E.M. Lim, J.P. Walsh, Age-specific TSH reference ranges have minimal impact on the diagnosis of thyroid dysfunction. Clin. Endocrinol. 77, 773–779 (2012)
K. Takeda, M. Mishiba, H. Sugiura, A. Nakajima, M. Kohama, S. Hiramatsu, Evaluated reference intervals for serum free thyroxine and thyrotropin using the conventional outliner rejection test without regard to presence of thyroid antibodies and prevalence of thyroid dysfunction in Japanese subjects. Endocr. J. 56, 1059–1066 (2009)
C.A. Spencer, J.G. Hollowell, M. Kazarosyan, L.E. Braverman, National Health and Nutrition Examination Survey III thyroid-stimulating hormone (TSH)-thyroperoxidase antibody relationships demonstrate that TSH upper reference limits may be skewed by occult thyroid dysfunction. J. Clin. Endocrinol. Metab. 92, 4236–4240 (2007)
A.P. Bremner, P. Feddema, P.J. Leedman, S.J. Brown, J.P. Beilby, E.M. Lim, S.G. Wilson, P.C. O’Leary, J.P. Walsh, Age-related changes in thyroid function: a longitudinal study of a community-based cohort. J. Clin. Endocrinol. Metab. 97, 1554–1562 (2012)
L. Mehran, A. Amouzgar, H. Delshad, F. Azizi, The association of cigarette smoking with serum TSH concentration and thyroperoxidase antibody. Exp. Clin. Endocrinol. Diabetes 120, 80–83 (2012)
R.M. Belin, B.C. Astor, N.R. Powe, P.W. Ladenson, Smoke exposure is associated with a lower prevalence of serum thyroid autoantibodies and thyrotropin concentration elevation and a higher prevalence of mild thyrotropin concentration suppression in the third National health and nutrition examination survey (NHANES III). J. Clin. Endocrinol. Metab. 89, 6077–6086 (2004)
X. Sun, Z. Shan, W. Teng, Effects of increased iodine intake on thyroid disorders. Endocrinol. Metab. 29, 240–247 (2014)
L. Bjergved, T. Jorgensen, H. Perrild, A. Carle, C. Cerqueira, A. Krejbjerg, P. Laurberg, L. Ovesen, I. Bulow Pedersen, R.L. Banke, N. Knudsen, Predictors of change in serum TSH after iodine fortification: an 11-year follow-up to the DanThyr study. J. Clin. Endocrinol. Metab. 97, 4022–4029 (2012)
L.E. Braverman, Iodine and the thyroid: 33 years of study. Thyroid 4, 351–356 (1994)
D.J. Topliss, Clinical update in aspects of the management of autoimmune thyroid diseases. Endocrinol. Metab. 31, 493–499 (2016)
M.I. Surks, L. Boucai, Age- and race-based serum thyrotropin reference limits. J. Clin. Endocrinol. Metab. 95, 496–502 (2010)
W. Teng, Z. Shan, X. Teng, H. Guan, Y. Li, D. Teng, Y. Jin, X. Yu, C. Fan, W. Chong, F. Yang, H. Dai, Y. Yu, J. Li, Y. Chen, D. Zhao, X. Shi, F. Hu, J. Mao, X. Gu, R. Yang, Y. Tong, W. Wang, T. Gao, C. Li, Effect of iodine intake on thyroid diseases in China. N. Engl. J. Med. 354, 2783–2793 (2006)
P. Laurberg, K.M. Pedersen, A. Hreidarsson, N. Sigfusson, E. Iversen, P.R. Knudsen, Iodine intake and the pattern of thyroid disorders: a comparative epidemiological study of thyroid abnormalities in the elderly in Iceland and in Jutland, Denmark. J. Clin. Endocrinol. Metab. 83, 765–769 (1998)
B. Biondi, D.S. Cooper, The clinical significance of subclinical thyroid dysfunction. Endocr. Rev. 29, 76–131 (2008)
H. Volzke, D. Alte, T. Kohlmann, J. Ludemann, M. Nauck, U. John, W. Meng, Reference intervals of serum thyroid function tests in a previously iodine-deficient area. Thyroid 15, 279–285 (2005)
World Health Organization. Urinary iodine concentrations for determining iodine status in populations, http://www.who.int/vmnis/indicators/urinaryiodine/en/. Accessed 20 Jan 2017
H.J. Kim, N.K. Kim, H.K. Park, D.W. Byun, K. Suh, M.H. Yoo, Y.K. Min, S.W. Kim, J.H. Chung, Strong association of relatively low and extremely excessive iodine intakes with thyroid cancer in an iodine-replete area. Eur. J. Nutr. 56, 965–971 (2017)
J.Y. Joung, Y.Y. Cho, S.M. Park, T.H. Kim, N.K. Kim, S.Y. Sohn, S.W. Kim, J.H. Chung, Effect of iodine restriction on thyroid function in subclinical hypothyroid patients in an iodine-replete area: a long period observation in a large-scale cohort. Thyroid 24, 1361–1368 (2014)
J. Lee, J.H. Kim, S.Y. Lee, J.H. Lee, Iodine status in Korean preschool children as determined by urinary iodine excretion. Eur. J. Nutr. 53, 683–688 (2014)
W.G. Kim, W.B. Kim, G. Woo, H. Kim, Y. Cho, T.Y. Kim, S.W. Kim, M.H. Shin, J.W. Park, H.L. Park, K. Oh, J.H. Chung, Thyroid stimulating hormone reference range and prevalence of thyroid dysfunction in the Korean population: Korea National Health and Nutrition Examination Survey 2013–2015. Endocrinol. Metab. 32, 106–114 (2017)
Z. Baloch, P. Carayon, B. Conte-Devolx, L.M. Demers, U. Feldt-Rasmussen, J.F. Henry, V.A. LiVosli, P. Niccoli-Sire, R. John, J. Ruf, P.P. Smyth, C.A. Spencer, J.R. Stockigt, N.A.o.C.B. guidelines committee, laboratory medicine practice guidelines. Laboratory support for the diagnosis and monitoring of thyroid disease. Thyroid 13, 3–126 (2003)
L. Boucai, M.I. Surks, Reference limits of serum TSH and free T4 are significantly influenced by race and age in an urban outpatient medical practice. Clin. Endocrinol. 70, 788–793 (2009)
G. Atzmon, N. Barzilai, M.I. Surks, I. Gabriely, Genetic predisposition to elevated serum thyrotropin is associated with exceptional longevity. J. Clin. Endocrinol. Metab. 94, 4768–4775 (2009)
G. Atzmon, N. Barzilai, J.G. Hollowell, M.I. Surks, I. Gabriely, Extreme longevity is associated with increased serum thyrotropin. J. Clin. Endocrinol. Metab. 94, 1251–1254 (2009)
H. Guan, Z. Shan, X. Teng, Y. Li, D. Teng, Y. Jin, X. Yu, C. Fan, W. Chong, F. Yang, H. Dai, Y. Yu, J. Li, Y. Chen, D. Zhao, X. Shi, F. Hu, J. Mao, X. Gu, R. Yang, W. Chen, Y. Tong, W. Wang, T. Gao, C. Li, W. Teng, Influence of iodine on the reference interval of TSH and the optimal interval of TSH: results of a follow-up study in areas with different iodine intakes. Clin. Endocrinol. 69, 136–141 (2008)
T. Kang, D. Leem, J. Seo, Y. Lee, T. Yoon, J. Lee, Y. Lee, Y. Kim, S. Kim, Monitoring of iodine in foods for estimation of dietary intake. R&D Annu. Rep. Korean Minist. Food Drug Saf. 16, 152 (2012)
J.Y. Kim, S.J. Moon, K.R. Kim, C.Y. Sohn, J.J. Oh, Dietary iodine intake and urinary iodine excretion in normal Korean adults. Yonsei Med. J. 39, 355–362 (1998)
M.J. Jeon, W.G. Kim, H. Kwon, M. Kim, S. Park, H.S. Oh, M. Han, T.Y. Kim, Y.K. Shong, W.B. Kim, Excessive iodine intake and thyrotropin reference interval: data from the Korean national health and nutrition examination survey. Thyroid 27, 967–972 (2017)
K.H. Choi, H.S. PY, S.H. Choi, S. Lim, D.J. Park, H.C. Jang, N.H. Cho, Cho BY, Prevalence of subclinical hypothyroidism in two population based-cohort: Ansung and KLoSHA cohort in Korea. J. Korean Thyroid Assoc. 3, 32–40 (2010)
F. Veltri, F.O. Rocha, D. Willems, J.P. Praet, L. Grabczan, P. Kleynen, T. Pepersack, K. Poppe, Prevalence of thyroid dysfunction and autoimmunity in the older population and implications of age-specific reference ranges. Clin. Chim. Acta 465, 34–39 (2017)
D. Unuane, B. Velkeniers, E. Anckaert, J. Schiettecatte, H. Tournaye, P. Haentjens, K. Poppe, Thyroglobulin autoantibodies: is there any added value in the detection of thyroid autoimmunity in women consulting for fertility treatment? Thyroid 23, 1022–1028 (2013)
Funding
This study was supported by a grant of the Korean Health Technology R&D project, Ministry of Health & Welfare, Republic of Korea (HC15C3372).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Kwon, H., Kim, W.G., Jeon, M.J. et al. Age-specific reference interval of serum TSH levels is high in adolescence in an iodine excess area: Korea national health and nutrition examination survey data. Endocrine 57, 445–454 (2017). https://doi.org/10.1007/s12020-017-1375-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-017-1375-5