Abstract
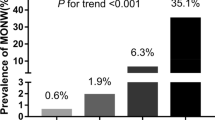
The secreted hepatokine fetuin-A emerges as an independent predictor of type 2 diabetes in adulthood. The overall aims of this study were: (1) to investigate the associations of fetuin-A with adiposity and insulin resistance, as well as its relationship with adipokines, in prepubertal children, and, (2) to evaluate whether, in prepubertal obesity, serum fetuin-A levels may either change or predict the responsiveness to an educational-based weight excess reduction program. We studied 200 prepubertal children (boys/girls: 89/111; Tanner stage 1; age: 5–13 years), included in a cohort of 44,231 adolescents who participated in an extensive Italian school-based survey. According to Cole’s criteria, 100 individuals were lean (boys/girls: 57/43) and 100 obese (boys/girls: 54/46). A subset of 53 obese individuals (boys/girls: 28/25; age: 6–12 years) were also evaluated after a weight excess reduction program. Serum fetuin-A, leptin, total and high molecular weight adiponectin levels, as well as homeostasis model assessment of insulin resistance were assessed. When compared with lean, obese children exhibited higher ( p < 0.0001) fetuin-A concentrations, without differences between sex. Fetuin-A was positively associated with adiposity, homeostasis model assessment of insulin resistance, and leptin levels. In multivariate analysis, the associations between fetuin-A and leptin or homeostasis model assessment of insulin resistance lost the significance after adjustment for BMI Z-score, which, in turn, represented an independent determinant of fetuin-A (R 2 adj 0.327; p < 0.0001). Notably, after weight excess reduction program, fetuin-A levels dropped ( p < 0.0001 vs. basal). Interestingly, no significant differences of fetuin-A concentrations between responders and no responders were found. In prepubertal children, fetuin-A represents an early marker of adiposity, and its reduction after lifestyle intervention may partly contribute to the beneficial effects of weight excess reduction program.


Similar content being viewed by others
References
J.L. Baker, L.W. Olsen, T.I. Sorensen, Childhood body-mass index and the risk of coronary heart disease in adulthood. N. Engl. J. Med. 357, 2329–2337 (2007)
J.C. Winer, T.L. Zern, S.E. Taksali, J. Dziura, A.M. Cali, M. Wollschlager, A.A. Seyal, R. Weiss, T.S. Burgert, S. Caprio, Adiponectin in childhood and adolescent obesity and its association with inflammatory markers and components of the metabolic syndrome. J. Clin. Endocrinol. Metab. 91(11), 4415–4423 (2006)
A. Sbarbati, F. Osculati, D. Silvagni, D. Benati, M. Galie, F.S. Camoglio, G. Rigotti, C. Maffeis, Obesity and inflammation: evidence for an elementary lesion. Pediatrics 117(1), 220–223 (2006)
M. Sabin, J. Holly, J. Shield, S. Turner, M. Grohmann, C. Stewart, E. Crowne, Mature subcutaneous and visceral adipocyte concentrations of adiponectin are highly correlated in prepubertal children and inversely related to body mass index standard deviation score. J. Clin. Endocrinol. Metab. 91, 332–335 (2006)
M. Valle, R. Martos, F. Gascon, R. Canete, M.A. Zafra, R. Morales, Low-grade systemic inflammation, hypoadiponectinemia and a high concentration of leptin are present in very young obese children, and correlate with metabolic syndrome. Diabetes Metab. 31(1), 55–62 (2005)
S.H. Ley, S.B. Harris, P.W. Connelly, M. Mamakeesick, J. Gittelsohn, R.A. Hegele, R. Retnakaran, B. Zinman, A.J. Hanley, Adipokines and incident type 2 diabetes in an Aboriginal Canadian population: the Sandy Lake Health and Diabetes Project. Diabetes Care 31(7), 1410–1415 (2008)
Y. Wang, K.S. Lam, M.H. Yau, A. Xu, Post-translational modifications of adiponectin: mechanisms and functional implications. Biochem. J. 409(3), 623–633 (2008)
N. Stefan, H. HU, The metabolically benign and malignant fatty liver. Diabetes 60, 2011–2017 (2011)
N. Stefan, H.U. Haring, The role of hepatokines in metabolism. Nat. Rev. Endocrinol. 9(3), 144–152 (2013)
C. Weikert, N. Stefan, M.B. Schulze, T. Pischon, K. Berger, H.G. Joost, H.U. Haring, H. Boeing, A. Fritsche, Plasma fetuin-a levels and the risk of myocardial infarction and ischemic stroke. Circulation 118(24), 2555–2562 (2008)
A. Iroz, J.-P. Couty, C. Postic, Hepatokines: unlocking the multi-organ network in metabolic diseases. Diabetologia 58, 1699–1703 (2015)
L. Kalabay, K. Chavin, J. Lebreton, K. Robinson, M. Buse, P. Arnaud, Human recombinant alpha 2-HS glycoprotein is produced in insect cells as a full length inhibitor of the insulin receptor tyrosine kinase. Horm. Metab. Res. 30, 1–6 (1998)
T. Reinehr, C.L. Roth, Fetuin-A and its relation to metabolic syndrome and fatty liver disease in obese children before and after weight loss. J. Clin. Endocrinol. Metab. 93(11), 4479–4485 (2008)
N. Stefan, Q. Sun, A. Fritsche, J. Machann, F. Schick, F. Gerst, C. Jeppesen, H.G. Joost, F.B. Hu, H. Boeing, S. Ullrich, H.U. Haring, M.B. Schulze, Impact of the adipokine adiponectin and the hepatokine fetuin-A on the development of type 2 diabetes: prospective cohort- and cross-sectional phenotyping studies. PLoS One 9(3), e92238 (2014)
A.M. Hennige, H. Staiger, C. Wicke, F. Machicao, A. Fritsche, H.U. Haring, N. Stefan, Fetuin-A induces cytokine expression and suppresses adiponectin production. PLoS One 3(3), e1765 (2008)
J.H. Ix, C.L. Wassel, A.M. Kanaya, E. Vittinghoff, K.C. Johnson, A. Koster, J.A. Cauley, T.B. Harris, S.R. Cummings, M.G. Shlipak, Fetuin-A and incident diabetes mellitus in older persons. J. Am. Med. Assoc. 300(2), 182–188 (2008)
T. Reinehr, B. Karges, T. Meissner, S. Wiegand, M. Fritsch, H. RWeinhard, J. Woelfle, Fibroblast growth factor 21 and fetuin-A in obese adolescents with and without type 2 diabetes. J. Clin. Endocrinol. Metab. 100, 3004–3010 (2015)
T. Reinehr, B. Stoffel-Wagner, C.L. Roth, Adipocyte fatty acid-binding protein in obese children before and after weight loss. Metabolism 56(12), 1735–1741 (2007)
J.M. Brix, H. Stingl, F. Hollerl, G.H. Schernthaner, H.P. Kopp, G. Schernthaner, Elevated fetuin-A concentrations in morbid obesity decrease after dramatic weight loss. J. Clin. Endocrinol. Metab. 95(11), 4877–4881 (2010)
T. Reinehr, J. Kratzsch, W. Kiess, W. Andler, Circulating soluble leptin receptor, leptin, and insulin resistance before and after weight loss in obese children. Int. J. Obes. (Lond.) 29(10), 1230–1235 (2005)
G. Di Stefano, V. Bini, F. Papi, F. Celi, G. Contessa, M.G. Berioli, M.L. Bacosi, A. Falorni, Leptin serum concentrations predict the responsiveness of obese children and adolescents to weight excess reduction program. Int. J. Obes. Relat. Metab. Disord. 24(12), 1586–1591 (2000)
G. Murdolo, B. Nowotny, F. Celi, M. Donati, V. Bini, F. Papi, G. Gornitzka, S. Castellani, M. Roden, A. Falorni, C. Herder, A. Falorni, Inflammatory adipokines, high molecular weight adiponectin, and insulin resistance: a population-based survey in prepubertal schoolchildren. PLoS One 6(2), e17264 (2011)
F. Celi, V. Bini, G. De Giorgi, D. Molinari, F. Faraoni, G. Di Stefano, M.L. Bacosi, M.G. Berioli, G. Contessa, A. Falorni, Epidemiology of overweight and obesity among school children and adolescents in three provinces of central Italy, 1993–2001: study of potential influencing variables. Eur. J. Clin. Nutr. 57, 1045–1051 (2003)
A. Falorni, G. Galmacci, V. Bini, F. Papi, D. Molinari, G. De Giorgi, F. Faraoni, F. Celi, G. Di Stefano, M.G. Berioli, G. Contessa, M.L. Bacosi, Fasting serum leptin levels in the analysis of body mass index cut-off values: are they useful for overweight screening in children and adolescents? A school population-based survey in three provinces of central Italy. Int. J. Obes. Relat. Metab. Disord. 22(12), 1197–1208 (1998)
A. Falorni, V. Bini, D. Molinari, F. Papi, F. Celi, G. Di Stefano, M.G. Berioli, M.L. Bacosi, G. Contessa, Leptin serum levels in normal weight and obese children and adolescents: relationship with age, sex, pubertal development, body mass index and insulin. Int. J. Obes. Relat. Metab. Disord. 21(10), 881–890 (1997)
T.J. Cole, M.C. Bellizzi, K.M. Flegal, W.H. Dietz, Establishing a standard definition for child overweight and obesity worldwide: international survey. Br. Med. J. 320(7244), 1240–1243 (2000)
F. Abbasi, J. Chu, C. Lamendola, T. McLaughlin, J. Hayden, G. Reaven, P. Reaven, Discrimination between obesity and insulin-resistance in the relationship with adiponectin. Diabetes 53, 585–590 (2004)
S. Araki, K. Dobashi, K. Kubo, K. Asayama, A. Shirahata, High molecular weight, rather than total, adiponectin levels better reflect metabolic abnormalities associated with childhood obesity. J. Clin. Endocrinol. Metab. 91(12), 5113–5116 (2006)
H. Mangge, G. Almer, S. Haj-Yahya, S. Pilz, R. Gasser, R. Moller, R. Horejsi, Preatherosclerosis and adiponectin subfractions in obese adolescents. Obesity (Silver Spring) 16(12), 2578–2584 (2008)
P.L. Tsou, Y.D. Jiang, C.C. Chang, J.N. Wei, F.C. Sung, C.C. Lin, C.C. Chiang, T.Y. Tai, L.M. Chuang, Sex-related differences between adiponectin and insulin resistance in schoolchildren. Diabetes Care 27(2), 308–313 (2004)
K.K. Andersen, J. Frystyk, O.D. Wolthers, C. Heuck, A. Flyvbjerg, Gender differences of oligomers and total adiponectin during puberty: a cross-sectional study of 859 Danish school children. J. Clin. Endocrinol. Metab. 92(5), 1857–1862 (2007)
A. Bottner, J. Kratzsch, G. Muller, T.M. Kapellen, S. Bluher, E. Keller, M. Bluher, W. Kiess, Gender differences of adiponectin levels develop during the progression of puberty and are related to serum androgen levels. J. Clin. Endocrinol. Metab. 89(8), 4053–4061 (2004)
A.M. Wallace, A.D. McMahon, C.J. Packard, A. Kelly, J. Shepherd, A. Gaw, N. Sattar, Plasma leptin and the risk of cardiovascular disease in the west of Scotland coronary prevention study (WOSCOPS). Circulation 104(25), 3052–3056 (2001)
N. Satoh, M. Naruse, T. Usui, T. Tagami, T. Suganami, K. Yamada, H. Kuzuya, A. Shimatsu, Y. Ogawa, Leptin-to-adiponectin ratio as a potential atherogenic index in obese type 2 diabetic patients. Diabetes Care 27(10), 2488–2490 (2004)
N. Stefan, A.M. Hennige, H. Staiger, J. Machann, F. Schick, S.M. Krober, F. Machicao, A. Fritsche, H.U. Haring, Alpha2-Heremans-Schmid glycoprotein/fetuin-A is associated with insulin resistance and fat accumulation in the liver in humans. Diabetes Care 29(4), 853–857 (2006)
I. Dahlman, P. Eriksson, M. Kaaman, H. Jiao, C.M. Lindgren, J. Kere, P. Arner, Alpha2-Heremans-Schmid glycoprotein gene polymorphisms are associated with adipocyte insulin action. Diabetologia 47(11), 1974–1979 (2004)
A. Siddiq, F. Lepretre, S. Hercberg, P. Froguel, F. Gibson, A synonymous coding polymorphism in the alpha2-Heremans-Schmid glycoprotein gene is associated with type 2 diabetes in French Caucasians. Diabetes 54(8), 2477–2481 (2005)
L. Groop, C. Forsblom, M. Lehtovirta, T. Tuomi, S. Karanko, M. Nissen, B.O. Ehrnstrom, B. Forsen, B. Isomaa, B. Snickars, M.R. Taskinen, Metabolic consequences of a family history of NIDDM (the Botnia study): evidence for sex-specific parental effects. Diabetes 45(11), 1585–1593 (1996)
J. Hwang, B. Thakkar, J. Chamberland, C. Mantzoros, Circulating fetuin-A levels are not affected by short and long-term energy deprivation and/or by leptin administration. Metabolism 63, 754–759 (2014)
B. Gustafson, A. Hammarstedt, C. Andersson, U. Smith, Inflamed adipose tissue: a culprit underlying the metabolic syndrome and atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 27, 2276–2283 (2007)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Murdolo, G., Tortoioli, C., Celi, F. et al. Fetuin-A, adiposity-linked insulin resistance and responsiveness to an educational-based weight excess reduction program: a population-based survey in prepubertal schoolchildren. Endocrine 56, 357–365 (2017). https://doi.org/10.1007/s12020-016-1009-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-016-1009-3