Abstract
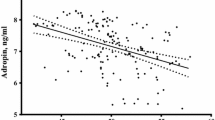
Betatrophin is a newly identified hormone determined to be a potent inducer of pancreatic beta cell proliferation in response to insulin resistance in mice. Polycystic ovary syndrome (PCOS) is an inflammatory-based metabolic disease associated with insulin resistance. However, no evidence is available indicating whether betatrophin is involved in women with PCOS. The objective of this study was to ascertain whether betatrophin levels are altered in women with PCOS. This study was conducted in secondary referral center. This cross-sectional study included 164 women with PCOS and 164 age- and BMI-matched female controls. Circulating betatrophin levels were measured using ELISA. Metabolic and hormonal parameters were also determined. Circulating betatrophin levels were significantly elevated in women with PCOS compared with controls (367.09 ± 55.78 vs. 295.65 ± 48.97 pg/ml, P < 0.001). Betatrophin levels were positively correlated with insulin resistance marker homeostasis model assessment of insulin resistance (HOMA-IR), free-testosterone, high-sensitivity C-reactive protein (hs-CRP), atherogenic lipid profiles, and BMI in PCOS. Multivariate logistic regression analyses revealed that the odds ratio for PCOS was 2.51 for patients in the highest quartile of betatrophin compared with those in the lowest quartile (95 % CI 1.31–4.81, P = 0.006). Multivariate regression analyses showed that HOMA-IR, hs-CRP, and free-testosterone were independent factors influencing serum betatrophin levels. Betatrophin levels were increased in women with PCOS and were associated with insulin resistance, hs-CRP, and free-testosterone in these patients. Elevated betatrophin levels were found to increase the odds of having PCOS. Further research is needed to elucidate the physiologic and pathologic significance of our findings.



Similar content being viewed by others
Abbreviations
- ANGPLT8:
-
Angiopoetin-like 8 protein
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- CV:
-
Coefficient of variability
- DHEA-S:
-
Dehydroepiandrosterone sulfate
- E2 :
-
Estradiol
- FBG:
-
Fasting blood glucose
- FG:
-
Ferriman–Gallwey
- GDM:
-
Gestational diabetes mellitus
- HDL-C:
-
High-density lipoprotein cholesterol
- HOMA-IR:
-
Homeostasis model assessment of insulin resistance
- hs-CRP:
-
High-sensitivity C-reactive protein
- LDL-C:
-
Low-density lipoprotein cholesterol
- OR:
-
Odds ratio
- PCOS:
-
Polycystic ovary syndrome
- RIFL:
-
Re-feeding induced fat and liver protein
- TD26:
-
Hepatocellular carcinoma-associated protein
- T2DM:
-
Type 2 diabetes mellitus
- VIF:
-
Variance inflation factor
References
D.A. Ehrmann, Polycystic ovary syndrome. N. Engl. J. Med. 352, 1223–1236 (2005)
R. Azziz, K.S. Woods, R. Reyna, T.J. Key, E.S. Knochenhauer, B.O. Yildiz, The prevalence and features of the polycystic ovary syndrome in an unselected population. J. Clin. Endocrinol. Metab. 89, 2745–2749 (2004)
R.S. Legro, S.A. Arslanian, D.A. Ehrmann, K.M. Hoeger, M.H. Murad, R. Pasquali, C.K. Welt, Diagnosis and treatment of polycystic ovary syndrome: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 98, 4565–4592 (2013)
C.N. Jayasena, S. Franks, The management of patients with polycystic ovary syndrome. Nat. Rev. Endocrinol. 10, 624–636 (2014)
R.A. Wild, E. Carmina, E. Diamanti-Kandarakis, A. Dokras, H.F. Escobar-Morreale, W. Futterweit, R. Lobo, R.J. Norman, E. Talbott, D.A. Dumesic, Assessment of cardiovascular risk and prevention of cardiovascular disease in women with the polycystic ovary syndrome: a consensus statement by the Androgen Excess and Polycystic Ovary Syndrome (AE-PCOS) Society. J. Clin. Endocrinol. Metab. 95, 2038–2049 (2010)
H. Mani, M.J. Levy, M.J. Davies, D.H. Morris, L.J. Gray, J. Bankart, H. Blackledge, K. Khunti, T.A. Howlett, Diabetes and cardiovascular events in women with polycystic ovary syndrome: a 20-year retrospective cohort study. Clin. Endocrinol. (Oxf) 78, 926–934 (2013)
C.G. Solomon, F.B. Hu, A. Dunaif, J.E. Rich-Edwards, M.J. Stampfer, W.C. Willett, F.E. Speizer, J.E. Manson, Menstrual cycle irregularity and risk for future cardiovascular disease. J. Clin. Endocrinol. Metab. 87, 2013–2017 (2002)
A. Dokras, Cardiovascular disease risk in women with PCOS. Steroids 78, 773–776 (2013)
L.K. Hoffman, D.A. Ehrmann, Cardiometabolic features of polycystic ovary syndrome. Nat. Clin. Pract. Endocrinol. Metab. 4, 215–222 (2008)
M.O. Goodarzi, D.A. Dumesic, G. Chazenbalk, R. Azziz, Polycystic ovary syndrome: etiology, pathogenesis and diagnosis. Nat. Rev. Endocrinol. 7, 219–231 (2011)
G. Ren, J.Y. Kim, C.M. Smas, Identification of RIFL, a novel adipocyte-enriched insulin target gene with a role in lipid metabolism. Am. J. Physiol. Endocrinol. Metab. 303, E334–E351 (2012)
R. Zhang, Lipasin, a novel nutritionally-regulated liver-enriched factor that regulates serum triglyceride levels. Biochem. Biophys. Res. Commun. 424, 786–792 (2012)
F. Quagliarini, Y. Wang, J. Kozlitina, N.V. Grishin, R. Hyde, E. Boerwinkle, D.M. Valenzuela, A.J. Murphy, J.C. Cohen, H.H. Hobbs, Atypical angiopoietin-like protein that regulates ANGPTL3. Proc. Natl. Acad. Sci. USA 109, 19751–19756 (2012)
P. Yi, J.-S. Park, D.A. Melton, Betatrophin: a hormone that controls pancreatic β cell proliferation. Cell 153, 747–758 (2013)
Y. Wang, F. Quagliarini, V. Gusarova, J. Gromada, D.M. Valenzuela, J.C. Cohen, H.H. Hobbs, Mice lacking ANGPTL8 (Betatrophin) manifest disrupted triglyceride metabolism without impaired glucose homeostasis. Proc. Natl. Acad. Sci. USA 110, 16109–16114 (2013)
D. Weissglas-Volkov, C.A. Aguilar-Salinas, E. Nikkola, K.A. Deere, I. Cruz-Bautista, O. Arellano-Campos, L.L. Muñoz-Hernandez, L. Gomez-Munguia, M.L. Ordoñez-Sánchez, P.M.V.L. Reddy, A.J. Lusis, N. Matikainen, M.-R. Taskinen, L. Riba, R.M. Cantor, J.S. Sinsheimer, T. Tusie-Luna, P. Pajukanta, Genomic study in Mexicans identifies a new locus for triglycerides and refines European lipid loci. J. Med. Genet. 50, 298–308 (2013)
G.M. Peloso, P.L. Auer, J.C. Bis, A. Voorman, A.C. Morrison, N.O. Stitziel, J.A. Brody, S.A. Khetarpal, J.R. Crosby, M. Fornage, A. Isaacs, J. Jakobsdottir, M.F. Feitosa, G. Davies, J.E. Huffman, A. Manichaikul, B. Davis, K. Lohman, A.Y. Joon, A.V. Smith, M.L. Grove, P. Zanoni, V. Redon, S. Demissie, K. Lawson, U. Peters, C. Carlson, R.D. Jackson, K.K. Ryckman, R.H. Mackey, J.G. Robinson, D.S. Siscovick, P.J. Schreiner, J.C. Mychaleckyj, J.S. Pankow, A. Hofman, A.G. Uitterlinden, T.B. Harris, K.D. Taylor, J.M. Stafford, L.M. Reynolds, R.E. Marioni, A. Dehghan, O.H. Franco, A.P. Patel, Y. Lu, G. Hindy, O. Gottesman, E.P. Bottinger, O. Melander, M. Orho-Melander, R.J.F. Loos, S. Duga, P.A. Merlini, M. Farrall, A. Goel, R. Asselta, D. Girelli, N. Martinelli, S.H. Shah, W.E. Kraus, M. Li, D.J. Rader, M.P. Reilly, R. McPherson, H. Watkins, D. Ardissino, NHLBI GO Exome Sequencing Project, Q. Zhang, J. Wang, M.Y. Tsai, H.A. Taylor, A. Correa, M.E. Griswold, L.A. Lange, J.M. Starr, I. Rudan, G. Eiriksdottir, L.J. Launer, J.M. Ordovas, D. Levy, Y.D.I. Chen, A.P. Reiner, C. Hayward, O. Polasek, I.J. Deary, I.B. Borecki, Y. Liu, V. Gudnason, J.G. Wilson, C.M. van Duijn, C. Kooperberg, S.S. Rich, B.M. Psaty, J.I. Rotter, C.J. O’Donnell, K. Rice, E. Boerwinkle, S. Kathiresan, L.A. Cupples, Association of low-frequency and rare coding-sequence variants with blood lipids and coronary heart disease in 56,000 whites and blacks. Am. J. Hum. Genet. 94, 223–232 (2014)
V. Gusarova, C.A. Alexa, E. Na, P.E. Stevis, Y. Xin, S. Bonner-Weir, J.C. Cohen, H.H. Hobbs, A.J. Murphy, G.D. Yancopoulos, J. Gromada, ANGPTL8/betatrophin does not control pancreatic beta cell expansion. Cell 159, 691–696 (2014)
D. Espes, M. Martinell, P.-O. Carlsson, Increased circulating betatrophin concentrations in patients with type 2 diabetes. Int. J. Endocrinol. 2014, 323407 (2014)
A. Fenzl, B.K. Itariu, L. Kosi, M. Fritzer-Szekeres, A. Kautzky-Willer, T.M. Stulnig, F.W. Kiefer, Circulating betatrophin correlates with atherogenic lipid profiles but not with glucose and insulin levels in insulin-resistant individuals. Diabetologia 57, 1204–1208 (2014)
J. Gomez-Ambrosi, E. Pascual, V. Catalan, A. Rodriguez, B. Ramirez, C. Silva, M.J. Gil, J. Salvador, G. Fruhbeck, Circulating betatrophin concentrations are decreased in human obesity and type 2 diabetes. J. Clin. Endocrinol. Metab. 99, E2004–E2009 (2014)
T. Gao, K. Jin, P. Chen, H. Jin, L. Yang, X. Xie, M. Yang, C. Hu, X. Yu, Circulating betatrophin correlates with triglycerides and postprandial glucose among different glucose tolerance statuses-a case-control study. PLoS One 10, e0133640 (2015)
R. Tarlatzis, B. Fauser, J. Chang, R. Azziz: Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). The Rotterdam ESHRE/ASRM-. Hum. Reprod. (2004)
D. Ferriman, J.D. Gallwey, Clinical assessment of body hair growth in women. J. Clin. Endocrinol. Metab. 21, 1440–1447 (1961)
D.R. Matthews, J.P. Hosker, A.S. Rudenski, B.A. Naylor, D.F. Treacher, R.C. Turner, Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28, 412–419 (1985)
M.H. Shanik, Y. Xu, J. Skrha, R. Dankner, Y. Zick, J. Roth, Insulin resistance and hyperinsulinemia: is hyperinsulinemia the cart or the horse? Diabetes Care 31, S262–S268 (2008)
E. Diamanti-Kandarakis, A. Dunaif, Insulin resistance and the polycystic ovary syndrome revisited: an update on mechanisms and implications. Endocr. Rev. 33, 981–1030 (2012)
P.M. Catalano, Trying to understand gestational diabetes. Diab. Med. 31, 273–281 (2014)
F. Ovalle, Insulin resistance, polycystic ovary syndrome, and type 2 diabetes mellitus. Fertil. Steril. 77, 1095–1105 (2002)
A. Dunaif, Insulin resistance and the polycystic ovary syndrome: mechanism and implications for pathogenesis 1. Endocr. Rev. 18, 774–800 (1997)
H. Hu, W. Sun, S. Yu, X. Hong, W. Qian, B. Tang, D. Wang, L. Yang, J. Wang, C. Mao, L. Zhou, G. Yuan, Increased circulating levels of betatrophin in newly diagnosed type 2 diabetic patients. Diab. Care 37, 2718–2722 (2014)
M. Abu-Farha, J. Abubaker, I. Al-Khairi, P. Cherian, F. Noronha, F.B. Hu, K. Behbehani, N. Elkum, Higher plasma betatrophin/ANGPTL8 level in Type 2 Diabetes subjects does not correlate with blood glucose or insulin resistance. Sci. Rep. 5, 10949 (2015)
N. Wawrusiewicz-Kurylonek, B. Telejko, M. Kuzmicki, A. Sobota, D. Lipinska, J. Pliszka, B. Raczkowska, P. Kuc, R. Urban, J. Szamatowicz, A. Kretowski, P. Laudanski, M. Gorska, Increased maternal and cord blood betatrophin in gestational diabetes. PLoS One 10, e0131171 (2015)
O. Erol, H.Y. Ellidağ, H. Ayık, M.K. Özel, A.U. Derbent, N. Yılmaz, Evaluation of circulating betatrophin levels in gestational diabetes mellitus. Gynecol. Endocrinol. 31, 1–5 (2015)
T. Ebert, S. Kralisch, U. Wurst, U. Lössner, J. Kratzsch, M. Blüher, M. Stumvoll, A. Tönjes, M. Fasshauer, Betatrophin levels are increased in women with gestational diabetes mellitus compared to healthy pregnant controls. Eur. J. Endocrinol. 173, 1–7 (2015)
X. Chen, P. Lu, W. He, J. Zhang, L. Liu, Y. Yang, Z. Liu, J. Xie, S. Shao, T. Du, X. Su, X. Zhou, S. Hu, G. Yuan, M. Zhang, H. Zhang, L. Liu, D. Wang, X. Yu, Circulating betatrophin levels are increased in patients with type 2 diabetes and associated with insulin resistance. J. Clin. Endocrinol. Metab. 100, E96–E100 (2015)
Acknowledgments
M.C., G.U.K., O.Y., and O.G.C. participated in study design and performed ELISA. M.C., P.Y., Y.M.S., and T.K. participated in study design, analyzed the data, wrote, reviewed, and edited the manuscript. O.Y. and M.T. provided serum samples and contributed to discussions of data interpretation. M.C. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
This study has not been funded by any organizations.
Disclosure
The authors have nothing to disclose.
Rights and permissions
About this article
Cite this article
Calan, M., Yilmaz, O., Kume, T. et al. Elevated circulating levels of betatrophin are associated with polycystic ovary syndrome. Endocrine 53, 271–279 (2016). https://doi.org/10.1007/s12020-016-0875-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-016-0875-z