Abstract
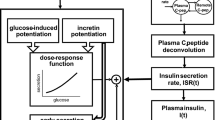
This study investigated the impact of incretin on early-phase insulin secretion and glucose excursion. The normal glucose tolerance (NGT), impaired glucose tolerance (IGT), and type 2 diabetes mellitus (T2DM) groups included 16, 8, and 19 subjects, respectively. Subjects underwent continuous glucose monitoring for 3 days, followed by an oral glucose tolerance test. Plasma glucose, insulin, glucagon, total glucose-dependent insulinotropic polypeptide (GIP), and glucagon-like peptide-l (GLP-1) levels were measured at 30-min increments for 2 h after glucose intake. Differences with P < 0.05 were considered statistically significant. The area under the curve (AUC) of total GIP (120-min GIP-AUC) of the T2DM group was significantly lower than those of the NGT and IGT groups. The 120-min GLP-1-AUC of the NGT group was significantly larger than those of the T2DM and IGT groups. The early-phase insulin secretion index (ΔI30/ΔG30) of the T2DM group was significantly lower than those of the NGT and IGT groups. Mean amplitudes of glycemic excursions (MAGEs) went in the order of NGT < IGT < T2DM (P < 0.01, IGT vs. NGT; P < 0.001, T2DM vs. IGT). The 120-min GIP-AUC was negatively correlated with MAGE (r = −0.464), but uncorrelated with ΔI30/ΔG30. The 120-min GLP-1-AUC was positively correlated with ΔI30/ΔG30 (r = 0.580), but negatively correlated with MAGE (r = −0.606). Incretin may ameliorate glucose excursions, and GLP-1 may exert them by promoting early-phase insulin secretion. No correlation was observed between GIP secretion and early-phase insulin secretion.


Similar content being viewed by others
References
R.A. DeFronzo, Current issues in the treatment of type 2 diabetes. Overview of newer agents: where treatment is going. Am. J. Med. 123, S38–S48 (2010)
L. Monnier, E. Mas, C. Ginet, F. Michel, L. Villon, J.P. Cristol, C. Colette, Activation of oxidative stress by acute glucose fluctuations compared with sustained chronic hyperglycemia in patients with type 2 diabetes. JAMA 295, 1681–1687 (2006)
L. Nalysnyk, M. Hernandez-Medina, G. Krishnarajah, Glycaemic variability and complications in patients with diabetes mellitus: evidence from a systematic review of the literature. Diabetes Obes. Metab. 12, 288–298 (2010)
D. Tsujino, R. Nishimura, K. Taki, Y. Miyashita, A. Morimoto, N. Tajima, Daily glucose profiles in Japanese people with normal glucose tolerance as assessed by continuous glucose monitoring. Diabetes Technol. Ther. 11, 457–460 (2009)
T.S. Temelkova-Kurktschiev, C. Koehler, E. Henkel, W. Leonhardt, K. Fuecker, M. Hanefeld, Postchallenge plasma glucose and glycemic spikes are more strongly associated with atherosclerosis than fasting glucose or HbA1c level. Diabetes Care 23, 1830–1834 (2000)
D. Koya, G.L. King, Protein kinase C activation and the development of diabetic complications. Diabetes 47, 859–866 (1998)
C. Wang, L. Lv, Y. Yang, D. Chen, G. Liu, L. Chen, Y. Song, L. He, X. Li, H. Tian, W. Jia, X. Ran, Glucose fluctuations in subjects with normal glucose tolerance, impaired glucose regulation and newly-diagnosed type 2 diabetes mellitus. Clin. Endocrinol. (Oxf.) 76, 810–815 (2012)
J. Liu, Y.B. Li, H. Shao, Y.X. Li, Y.H. Yuan, Y.B. Xiao, J.P. Weng, Evaluation of islet beta cell function in subjects with normal glucose tolerance, impaired glucose regulation, and type 2 diabetes mellitus. Zhonghua Yi Xue Za Zhi 87, 1252–1255 (2007)
T.N. Kim, M.S. Park, S.K. Lee, S.J. Yang, K.W. Lee, M.S. Nam, Y.S. Park, J.T. Woo, Y.S. Kim, S.H. Baik, Elevated A1C is associated with impaired early-phase insulin secretion rather than insulin resistance in Koreans at high risk for developing diabetes. Endocrine 42, 548–591 (2012)
K. Matsumoto, H. Sakamaki, K. Izumino, M. Yano, Y. Ueki, S. Miyake, Y. Tominega, Increased insulin sensitivity and decreased insulin secretion in offspring of insulin-sensitive type 2 diabetic patients. Metabolism 49, 1219–1223 (2000)
Y. Seino, M. Fukushima, D. Yabe, GIP and GLP-1, the two incretin hormones: similarities and differences. J. Diabetes Invest. 1(1–2), 8–23 (2010)
T. Vilsbøll, T. Krarup, C.F. Deacon, S. Madesbad, J.J. Holst, Reduced postprandial concentrations of intact biologically active glucagon-like peptide 1 in type 2 diabetic patients. Diabetes 50, 609–613 (2001)
M.B. Toft-Nielsen, M.B. Damholt, S. Madsbad, L.M. Hilsted, T.E. Hughes, B.K. Michelsen, J.J. Holst, Determinants of the impaired secretion of glucagon-like peptide-1 in type 2 diabetic patients. J. Clin. Endocrinol. Metab. 86, 3717–3723 (2001)
J. Skrha, J. Hilgertová, M. Jarolímková, M. Kunesová, M. Hill, Meal test for glucose-dependent insulinotropic peptide (GIP) in obese and type 2 diabetic patients. Physiol. Res. 59, 749–755 (2010)
S.J. Han, H.J. Kim, S.E. Choi, Y. Kang, K.W. Lee, D.J. Kim, Incretin secretion and serum DPP-IV activity in Korean patients with type 2 diabetes. Diabetes Res. Clin. Pract. 89(3), e49–e52 (2010)
J. Kozawa, K. Okita, A. Imagawa, J.J. Holst, K. Yamagata, I. Shimomura, Similar incretin secretion in obese and non-obese Japanese subjects with type 2 diabetes. Biochem. Biophys. Res. Commun. 393(3), 410–413 (2010)
M.A. Narck, I. Vardarli, C.F. Deacon, J.J. Holst, J.J. Meier, Secretion of glucagon-like peptide-1 (GLP-1) in type 2 diabetes:what is up, what is down? Diabetologia 54, 10–18 (2011)
S. Lee, D. Yabe, K. Nohtomi, M. Takada, R. Morita, Y. Seino, T. Hirano, Intact glucagon-like peptide-1 levels are not decreased in Japanese patients with type 2 diabetes. Endocr. J. 57, 119–126 (2010)
S.J. Han, H.J. Kim, S.E. Choi, Y. Kang, K.W. Lee, D.J. Kim, Incretin secretion and serum DPP-IV activity in Korean patients with type 2 diabetes. Diabetes Res. Clin. Pract. 89, e49–e52 (2010)
N. Harada, A. Hamasaki, S. Yamane, A. Muraoka, E. Joo, K. Fujita, N. Inagaki, Plasma gastric inhibitory polypeptide and glucagon-like peptide-1 levels after glucose loading are associated with different factors in Japanese subjects. J. Diabetes Invest. 2(3), 193–199 (2011)
B. Laferrere, Do we really know why diabetes remits after gastric bypass surgery? Endocrine 40, 162–167 (2011)
E. Mannucci, L. Pala, M. Monami, L. Da Vico, G. Bardini, I. Dicembrini, S. Ciani, C. Lamanna, N. Marchionni, C.M. Rotella, Glucagon-like peptide-1 response to meals and post-prandial hyperglycemia in type 2 diabetic patients. J. Endocrinol. Invest. 33(3), 147–150 (2010)
F. Fehse, M. Trautmann, J.J. Holst, A.E. Halseth, N. Nanayakkara, L.L. Nielsen, M.S. Fineman, D.D. Kim, M.A. Nauck, Exenatide augments first- and second-phase insulin secretion in response to intravenous glucose in subjects with type 2 diabetes. J. Clin. Endocrinol. Metab. 90(11), 5991–5997 (2005)
K.M. Johnson, T. Farmer, K. Schurr, E. Patrick Donahue, B. Farmer, D. Neal, A.D. Cherrington, Endogenously released GLP-1 is not sufficient to alter postprandial glucose regulation in the dog. Endocrine 39(3), 229–234 (2011)
D. Yabe, K. Watanabe, K. Sugawara, H. Kuwata, Y. Kitamoto, K. Sugizaki, S. Fujiwara, M. Hishizawa, T. Hyo, K. Kuwabara, K. Yokota, M. Iwasaki, N. Kitatani, T. Kurose, N. Inagaki, Y. Seino, Comparison of incretin immunoassays with or without plasma extraction: incretin secretion in Japanese patients with type 2 diabetes. J. Diabetes Invest. 3(1), 70–79 (2012)
J.T. Lewis, B. Dayanandan, J.F. Habener, T.J. Kieffer, Glucose-dependent insulinotropic polypeptide confers early phase insulin release to oral glucose in rats: demonstration by a receptor antagonist. Endocrinology 141(10), 3710–3716 (2000)
Acknowledgments
This study was supported by the Science and Technology Projects of Guangdong Province (2009B011400036) in China.
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical standards
This study complied with the current laws of the People’s Republic of China.
Author information
Authors and Affiliations
Corresponding author
Additional information
Jie Shen and Zhi Chen contributed equally to this study.
Rights and permissions
About this article
Cite this article
Shen, J., Chen, Z., Chen, C. et al. Impact of incretin on early-phase insulin secretion and glucose excursion. Endocrine 44, 403–410 (2013). https://doi.org/10.1007/s12020-012-9867-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-012-9867-9