Abstract
Osteoarthritis is a highly prevalent disease particularly in subjects over 65 years of age worldwide. While in the past it was considered a mere consequence of cartilage degradation leading to anatomical and functional joint impairment, in recent decades, there has been a more dynamic view with the synovium, the cartilage, and the subchondral bone producing inflammatory mediators which ultimately lead to cartilage damage. Inflammaging is defined as a chronic, sterile, low-grade inflammation state driven by endogenous signals in the absence of infections, occurring with aging. This chronic status is linked to the production of reactive oxygen species and molecules involved in the development of age-related disease such as cancer, diabetes, and cardiovascular and neurodegenerative diseases. Inflammaging contributes to osteoarthritis development where both the innate and the adaptive immune response are involved. Elevated systemic and local inflammatory cytokines and senescent molecules promote cartilage degradation, and antigens derived from damaged joints further trigger inflammation through inflammasome activation. B and T lymphocyte populations also change with inflammaging and OA, with reduced regulatory functions, thus implicating self-reactivity as an additional mechanism of joint damage. The discovery of the underlying pathogenic pathways may help to identify potential therapeutic targets for the management or the prevention of osteoarthritis. We will provide a comprehensive evaluation of the current literature on the role of inflammaging in osteoarthritis and discuss the emerging therapeutic strategies.

Similar content being viewed by others
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Bland JH, Cooper SM (1984) Osteoarthritis: a review of the cell biology involved and evidence for reversibility. Management rationally related to known genesis and pathophysiology. Semin Arthritis Rheum 14:106–133
Hutton CW (1989) Osteoarthritis: the cause not result of joint failure? Ann Rheum Dis 48:958–961. https://doi.org/10.1136/ard.48.11.958
Litwic A, Edwards MH, Dennison EM, Cooper C (2013) Epidemiology and burden of osteoarthritis. Br Med Bull 105:185–199. https://doi.org/10.1093/bmb/lds038
Altman R, Alarcón G, Appelrouth D et al (1991) The American college of rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum 34:505–514. https://doi.org/10.1002/art.1780340502
Altman R, Asch E, Bloch D et al (1986) Development of criteria for the classification and reporting of osteoarthritis: classification of osteoarthritis of the knee. Arthritis Rheum 29:1039–1049. https://doi.org/10.1002/art.1780290816
Altman R, Alarcon G, Appelrouth D et al (1990) The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hand. Arthritis Rheum 33:1601–1610. https://doi.org/10.1002/art.1780331101
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteoarthrosis. Ann Rheum Dis 16:494–502. https://doi.org/10.1136/ard.16.4.494
Loeser RF, Goldring SR, Scanzello CR, Goldring MB (2012) Osteoarthritis: a disease of the joint as an organ. Arthritis Rheum 64:1697–1707
Sharma L, Chmiel JS, Almagor O et al (2014) Significance of preradiographic magnetic resonance imaging lesions in persons at increased risk of knee osteoarthritis. Arthritis Rheumatol 66:1811–1819. https://doi.org/10.1002/art.38611
Hunter DJ, March L, Chew M (2020) Osteoarthritis in 2020 and beyond: a Lancet Commission. Lancet 396:1711–1712
Zhang Y, Jordan JM (2010) Epidemiology of osteoarthritis. Clin Geriatr Med 26:355–369
Lawrence RC, Felson DT, Helmick CG et al (2008) Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II Arthritis Rheum 58:26–35. https://doi.org/10.1002/art.23176
Zhang Y, Niu J, Kelly-Hayes M et al (2002) Prevalence of symptomatic hand osteoarthritis and its impact on functional status among the elderly: the Framingham study. Am J Epidemiol 156:1021–1027. https://doi.org/10.1093/aje/kwf141
Xie F, Kovic B, Jin X et al (2016) Economic and humanistic burden of osteoarthritis: A systematic review of large sample studies. Pharmacoeconomics 34:1087–1100
Hubertsson J, Turkiewicz A, Petersson IF, Englund M (2017) Understanding occupation, sick leave, and disability pension due to knee and hip osteoarthritis from a sex perspective. Arthritis Care Res 69:226–233. https://doi.org/10.1002/acr.22909
Cross M, Smith E, Hoy D et al (2014) The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis 73:1323–1330. https://doi.org/10.1136/annrheumdis-2013-204763
Haan MN, Lee A, Odden MC et al (2016) Gender differences in the combined effects of cardiovascular disease and osteoarthritis on progression to functional impairment in older Mexican Americans. J Gerontol - Ser A Biol Sci Med Sci 71:1089–1095. https://doi.org/10.1093/gerona/glw014
Park JI, Jung HH (2017) Estimation of years lived with disability due to noncommunicable diseases and injuries using a population-representative survey. PLoS ONE 12. https://doi.org/10.1371/journal.pone.0172001
Veronese N, Stubbs B, Solmi M et al (2017) Association between lower limb osteoarthritis and incidence of depressive symptoms: data from the osteoarthritis initiative. Age Ageing 46:470–476. https://doi.org/10.1093/ageing/afw216
Kye SY, Park K (2017) Suicidal ideation and suicidal attempts among adults with chronic diseases: a cross-sectional study. Compr Psychiatry 73:160–167. https://doi.org/10.1016/j.comppsych.2016.12.001
Innes KE, Sambamoorthi U (2018) The association of perceived memory loss with osteoarthritis and related joint pain in a large Appalachian population. Pain Med (United States) 19:1340–1356. https://doi.org/10.1093/pm/pnx107
Schieir O, Tosevski C, Glazier RH et al (2017) Incident myocardial infarction associated with major types of arthritis in the general population: a systematic review and meta-analysis. Ann Rheum Dis 76:1396–1404. https://doi.org/10.1136/annrheumdis-2016-210275
Chung WS, Lin HH, Ho FM et al (2016) Risks of acute coronary syndrome in patients with osteoarthritis: a nationwide population-based cohort study. Clin Rheumatol 35:2807–2813. https://doi.org/10.1007/s10067-016-3391-x
Courties A, Sellam J, Maheu E et al (2017) Coronary heart disease is associated with a worse clinical outcome of hand osteoarthritis: a cross-sectional and longitudinal study. RMD Open 3. https://doi.org/10.1136/rmdopen-2016-000344
Gao SG, Zeng C, Xiong YL et al (2016) Is painful knee an independent predictor of mortality in middle-aged women? Ann Rheum Dis 75:e22
Piva SR, Susko AM, Khoja SS et al (2015) Links between osteoarthritis and diabetes: implications for management from a physical activity perspective. Clin Geriatr Med 31:67–87
Hawker GA, Croxford R, Bierman AS et al (2017) Osteoarthritis-related difficulty walking and risk for diabetes complications. Osteoarthr Cartil 25:67–75. https://doi.org/10.1016/j.joca.2016.08.003
Jeon CY, Lokken RP, Hu FB, Van Dam RM (2007) Physical activity of moderate intensity and risk of type 2 diabetes: a systematic review. Diabetes Care 30:744–752
Messier SP, Mihalko SL, Legault C et al (2013) Effects of intensive diet and exercise on knee joint loads, inflammation, and clinical outcomes among overweight and obese adults with knee osteoarthritis: The IDEA randomized clinical trial. JAMA - J Am Med Assoc 310:1263–1273. https://doi.org/10.1001/jama.2013.277669
Duncan BB, Schmidt MI, Pankow JS et al (2003) Low-grade systemic inflammation and the development of type 2 diabetes: the atherosclerosis risk in communities study. Diabetes 52:1799–1805. https://doi.org/10.2337/diabetes.52.7.1799
Rahman MM, Cibere J, Anis AH et al (2014) Risk of type 2 diabetes among osteoarthritis patients in a prospective longitudinal study. Int J Rheumatol 2014. https://doi.org/10.1155/2014/620920
Neogi T, Zhang Y (2013) Epidemiology of osteoarthritis. Rheum Dis Clin North Am 39:1–19
Agricola R, Heijboer MP, Roze RH et al (2013) Pincer deformity does not lead to osteoarthritis of the hip whereas acetabular dysplasia does: acetabular coverage and development of osteoarthritis in a nationwide prospective cohort study (CHECK). Osteoarthr Cartil 21:1514–1521. https://doi.org/10.1016/j.joca.2013.07.004
Valdes AM, Spector TD (2011) Genetic epidemiology of hip and knee osteoarthritis. Nat Rev Rheumatol 7:23–32. https://doi.org/10.1038/NRRHEUM.2010.191
Loughlin J (2005) The genetic epidemiology of human primary osteoarthritis: current status. Expert Rev Mol Med 7. https://doi.org/10.1017/S1462399405009257
Zeggini E, Panoutsopoulou K, Southam L et al (2012) Identification of new susceptibility loci for osteoarthritis (arcOGEN): a genome-wide association study. Lancet 380:815–823. https://doi.org/10.1016/S0140-6736(12)60681-3
Warnera SC, Valdesa AM (2017) Genetic association studies in osteoarthritis: is it fairytale? Curr Opin Rheumatol 29:103–109
Hochberg MC, Yerges-Armstrong L, Yau M, Mitchell BD (2013) Genetic epidemiology of osteoarthritis: recent developments and future directions. Curr Opin Rheumatol 25:192–197
Rogers EL, Reynard LN, Loughlin J (2015) The role of inflammation-related genes in osteoarthritis. Osteoarthr Cartil 23:1933–1938. https://doi.org/10.1016/J.JOCA.2015.01.003
Reynard LN, Loughlin J (2013) Insights from human genetic studies into the pathways involved in osteoarthritis. Nat Rev Rheumatol 9:573–583. https://doi.org/10.1038/NRRHEUM.2013.121
Goldring MB, Marcu KB (2012) Epigenomic and microRNA-mediated regulation in cartilage development, homeostasis, and osteoarthritis. Trends Mol Med 18:109–118. https://doi.org/10.1016/J.MOLMED.2011.11.005
Barter MJ, Bui C, Young DA (2012) Epigenetic mechanisms in cartilage and osteoarthritis: DNA methylation, histone modifications and microRNAs. Osteoarthr Cartil 20:339–349. https://doi.org/10.1016/J.JOCA.2011.12.012
Loughlin J, Reynard LN (2015) Osteoarthritis: epigenetics of articular cartilage in knee and hip OA. Nat Rev Rheumatol 11:6–7. https://doi.org/10.1038/NRRHEUM.2014.189
Shen J, Abu-Amer Y, O’Keefe RJ, McAlinden A (2017) Inflammation and epigenetic regulation in osteoarthritis. Connect Tissue Res 58:49–63. https://doi.org/10.1080/03008207.2016.1208655
Unnikrishnan A, Freeman WM, Jackson J et al (2019) The role of DNA methylation in epigenetics of aging. Pharmacol Ther 195:172–185. https://doi.org/10.1016/J.PHARMTHERA.2018.11.001
Allen KD, Golightly YM (2015) State of the evidence. Curr Opin Rheumatol 27:276–283
Glyn-Jones S, Palmer AJR, Agricola R et al (2015) Osteoarthritis. In: The Lancet. Lancet Publishing Group, pp 376–387
Agricola R, Waarsing JH, Arden NK et al (2013) Cam impingement of the hip-a risk factor for hip osteoarthritis. Nat Rev Rheumatol 9:630–634
Neogi T, Bowes MA, Niu J et al (2013) Magnetic resonance imaging-based three-dimensional bone shape of the knee predicts onset of knee osteoarthritis: data from the osteoarthritis initiative. Arthritis Rheum 65:2048–2058. https://doi.org/10.1002/art.37987
Sharma L, Chmiel JS, Almagor O et al (2013) The role of varus and valgus alignment in the initial development of knee cartilage damage by MRI: the MOST study. Ann Rheum Dis 72:235–240. https://doi.org/10.1136/annrheumdis-2011-201070
Felson DT, Niu J, Gross KD et al (2013) Valgus malalignment is a risk factor for lateral knee osteoarthritis incidence and progression: findings from the multicenter osteoarthritis study and the osteoarthritis initiative. Arthritis Rheum 65:355–362. https://doi.org/10.1002/art.37726
Harvey WF, Yang M, Cooke TDV et al (2010) Association of leg-length inequality with knee osteoarthritis a cohort study. Ann Intern Med 152:287–295. https://doi.org/10.7326/0003-4819-152-5-201003020-00006
Wang Y, Wluka AE, Berry PA et al (2012) Increase in vastus medialis cross-sectional area is associated with reduced pain, cartilage loss, and joint replacement risk in knee osteoarthritis. Arthritis Rheum 64:3917–3925. https://doi.org/10.1002/art.34681
Lievense AM, Bierma-Zeinstra SMA, Verhagen AP et al (2003) Influence of sporting activities on the development of osteoarthritis of the hip: a systematic review. Arthritis Care Res 49:228–236
Siebenrock KA, Kaschka I, Frauchiger L et al (2013) Prevalence of cam-type deformity and hip pain in elite ice hockey players before and after the end of growth. Am J Sports Med 41:2308–2313. https://doi.org/10.1177/0363546513497564
Nevitt MC, Zhang Y, Javaid MK et al (2010) High systemic bone mineral density increases the risk of incident knee OA and joint space narrowing, but not radiographic progression of existing knee OA: The MOST study. Ann Rheum Dis 69:163–168. https://doi.org/10.1136/ard.2008.099531
Muthuri SG, McWilliams DF, Doherty M, Zhang W (2011) History of knee injuries and knee osteoarthritis: a meta-analysis of observational studies. Osteoarthr Cartil 19:1286–1293. https://doi.org/10.1016/j.joca.2011.07.015
Blagojevic M, Jinks C, Jeffery A, Jordan KP (2010) Risk factors for onset of osteoarthritis of the knee in older adults: a systematic review and meta-analysis. Osteoarthr Cartil 18:24–33. https://doi.org/10.1016/j.joca.2009.08.010
Conde J, Scotece M, Gómez R et al (2011) Adipokines and osteoarthritis: novel molecules involved in the pathogenesis and progression of disease. Arthritis 2011:1–8. https://doi.org/10.1155/2011/203901
Reyes C, Leyland KM, Peat G et al (2016) Association between overweight and obesity and risk of clinically diagnosed knee, hip, and hand osteoarthritis: a population-based cohort study. Arthritis Rheumatol 68:1869–1875. https://doi.org/10.1002/art.39707
Gersing AS, Schwaiger BJ, Nevitt MC et al (2017) Is weight loss associated with less progression of changes in knee articular cartilage among obese and overweight patients as assessed with MR imaging over 48 months? Data from the osteoarthritis initiative. Radiology 284:508–520. https://doi.org/10.1148/radiol.2017161005
Atukorala I, Makovey J, Lawler L et al (2016) Is there a dose-response relationship between weight loss and symptom improvement in persons with knee osteoarthritis? Arthritis Care Res 68:1106–1114. https://doi.org/10.1002/acr.22805
Frey N, Hügle T, Jick SS et al (2017) Hyperlipidaemia and incident osteoarthritis of the hand: a population-based case-control study. Osteoarthr Cartil 25:1040–1045. https://doi.org/10.1016/j.joca.2017.01.014
Garcia-Gil M, Reyes C, Ramos R et al (2017) Serum lipid levels and risk of hand osteoarthritis: the Chingford prospective cohort study. Sci Rep 7. https://doi.org/10.1038/s41598-017-03317-4
Driban JB, Lo GH, Eaton CB et al (2016) Exploratory analysis of osteoarthritis progression among medication users: data from the Osteoarthritis Initiative. Ther Adv Musculoskelet Dis 8:207–219. https://doi.org/10.1177/1759720X16664323
Lo GH, McAlindon TE, Katz JN et al (2017) Systolic and pulse pressure associate with incident knee osteoarthritis: data from the Osteoarthritis Initiative. Clin Rheumatol 36:2121–2128. https://doi.org/10.1007/s10067-017-3656-z
Magnusson K, Bech Holte K, Juel NG et al (2017) Long term type 1 diabetes is associated with hand pain, disability and stiffness but not with structural hand osteoarthritis features - The Dialong hand study. PLoS ONE 12. https://doi.org/10.1371/journal.pone.0177118
Frey N, Hügle T, Jick SS et al (2016) Type II diabetes mellitus and incident osteoarthritis of the hand: a population-based case–control analysis. Osteoarthr Cartil 24:1535–1540. https://doi.org/10.1016/j.joca.2016.04.005
Garessus EDG, de Mutsert R, Visser AW et al (2016) No association between impaired glucose metabolism and osteoarthritis. Osteoarthr Cartil 24:1541–1547. https://doi.org/10.1016/j.joca.2016.04.007
Wang X, Cicuttini F, Jin X et al (2017) Knee effusion-synovitis volume measurement and effects of vitamin D supplementation in patients with knee osteoarthritis. Osteoarthr Cartil 25:1304–1312. https://doi.org/10.1016/j.joca.2017.02.804
Berenbaum F (2013) Osteoarthritis as an inflammatory disease (osteoarthritis is not osteoarthrosis!). Osteoarthr Cartil 21:16–21
Hwang HS, Kim HA (2015) Chondrocyte apoptosis in the pathogenesis of osteoarthritis. Int J Mol Sci 16:26035–26054
Guilak F, Nims RJ, Dicks A et al (2018) Osteoarthritis as a disease of the cartilage pericellular matrix. Matrix Biol 71–72:40–50
Funck-Brentano T, Cohen-Solal M (2015) Subchondral bone and osteoarthritis. Curr Opin Rheumatol 27:420–426
Kovács B, Vajda E, Nagy EE (2019) Regulatory effects and interactions of the Wnt and OPG-RANKL-RANK signaling at the bone-cartilage interface in osteoarthritis. Int J Mol Sci 20
Zhou X, Cao H, Yuan Y, Wu W (2020) Biochemical signals mediate the crosstalk between cartilage and bone in osteoarthritis. Biomed Res Int 2020
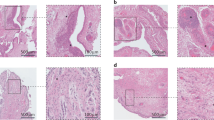
Mathiessen A, Conaghan PG (2017) Synovitis in osteoarthritis: current understanding with therapeutic implications. Arthritis Res Ther 19
Sarmanova A, Hall M, Moses J et al (2016) Synovial changes detected by ultrasound in people with knee osteoarthritis – a meta-analysis of observational studies. Osteoarthr Cartil 24:1376–1383. https://doi.org/10.1016/j.joca.2016.03.004
Guermazi A, Hayashi D, Roemer FW et al (2014) Synovitis in knee osteoarthritis assessed by contrast-enhanced magnetic resonance imaging (MRI) is associated with radiographic tibiofemoral osteoarthritis and MRI-detected widespread cartilage damage: The MOST study. J Rheumatol 41:501–508. https://doi.org/10.3899/jrheum.130541
Felson DT, Niu J, Neogi T et al (2016) Synovitis and the risk of knee osteoarthritis: the MOST study. Osteoarthr Cartil 24:458–464. https://doi.org/10.1016/j.joca.2015.09.013
Prieto-Potin I, Largo R, Roman-Blas JA et al (2015) Characterization of multinucleated giant cells in synovium and subchondral bone in knee osteoarthritis and rheumatoid arthritis. BMC Musculoskelet Disord 16. https://doi.org/10.1186/s12891-015-0664-5
Wojdasiewicz P, Poniatowski ŁA, Szukiewicz D (2014) The role of inflammatory and anti-inflammatory cytokines in the pathogenesis of osteoarthritis. Mediators Inflamm 2014
Klein-Wieringa IR, De Lange-Brokaar BJE, Yusuf E et al (2016) Inflammatory cells in patients with endstage knee osteoarthritis: a comparison between the synovium and the infrapatellar fat pad. J Rheumatol 43:771–778. https://doi.org/10.3899/jrheum.151068
Kapoor M, Martel-Pelletier J, Lajeunesse D et al (2011) Role of proinflammatory cytokines in the pathophysiology of osteoarthritis. Nat Rev Rheumatol 7:33–42
Cai S, Ming B, Ye C et al (2021) Similar transition processes in synovial fibroblasts from rheumatoid arthritis and osteoarthritis: a single-cell study. Clin Dev Immunol 2019. https://doi.org/10.1155/2019/4080735
Jin X, Beguerie JR, Zhang W et al (2015) Circulating C reactive protein in osteoarthritis: a systematic review and meta-analysis. Ann Rheum Dis 74:703–710. https://doi.org/10.1136/annrheumdis-2013-204494
Stannus O, Jones G, Cicuttini F et al (2010) Circulating levels of IL-6 and TNF-α are associated with knee radiographic osteoarthritis and knee cartilage loss in older adults. Osteoarthr Cartil 18:1441–1447. https://doi.org/10.1016/j.joca.2010.08.016
Livshits G, Zhai G, Hart DJ et al (2009) Interleukin-6 is a significant predictor of radiographic knee osteoarthritis: the Chingford study. Arthritis Rheum 60:2037–2045. https://doi.org/10.1002/art.24598
Spector TD, Hart DJ, Nandra D et al (1997) Low-level increases in serum C-reactive protein are present in early osteoarthritis of the knee and predict progressive disease. Arthritis Rheum 40:723–727. https://doi.org/10.1002/art.1780400419
Bulló M, Casas-Agustench P, Amigó-Correig P et al (2007) Inflammation, obesity and comorbidities: the role of diet. Public Health Nutr 10:1164–1172
Presle N, Pottie P, Dumond H et al (2006) Differential distribution of adipokines between serum and synovial fluid in patients with osteoarthritis. Contribution of joint tissues to their articular production. Osteoarthr Cartil 14:690–695. https://doi.org/10.1016/j.joca.2006.01.009
de Boer TN, van Spil WE, Huisman AM et al (2012) Serum adipokines in osteoarthritis; comparison with controls and relationship with local parameters of synovial inflammation and cartilage damage. Osteoarthr Cartil 20:846–853. https://doi.org/10.1016/j.joca.2012.05.002
Liu B, Gao YH, Dong N et al (2019) Differential expression of adipokines in the synovium and infrapatellar fat pad of osteoarthritis patients with and without metabolic syndrome. Connect Tissue Res 60:611–618. https://doi.org/10.1080/03008207.2019.1620221
Tu C, He J, Wu B et al (2019) An extensive review regarding the adipokines in the pathogenesis and progression of osteoarthritis. Cytokine 113:1–12
Neumann E, Junker S, Schett G et al (2016) Adipokines in bone disease. Nat Rev Rheumatol 12:296–302
Zhao CW, Gao YH, Song WX et al (2019) An update on the emerging role of resistin on the pathogenesis of osteoarthritis. Mediators Inflamm 2019
Garten A, Schuster S, Penke M et al (2015) Physiological and pathophysiological roles of NAMPT and NAD metabolism. Nat Rev Endocrinol 11:535–546. https://doi.org/10.1038/NRENDO.2015.117
Travelli C, Consonni FM, Sangaletti S et al (2019) Nicotinamide phosphoribosyltransferase acts as a metabolic gate for mobilization of myeloid-derived suppressor cells. Cancer Res 79:1938–1951. https://doi.org/10.1158/0008-5472.CAN-18-1544
Yu Q, Dong L, Li Y, Liu G (2018) SIRT1 and HIF1α signaling in metabolism and immune responses. Cancer Lett 418:20–26. https://doi.org/10.1016/J.CANLET.2017.12.035
Dvir-Ginzberg M, Steinmeyer J (2013) Towards elucidating the role of SirT1 in osteoarthritis. Front Biosci (Landmark Ed) 18:343–355. https://doi.org/10.2741/4105
Chen C, Zhou M, Ge Y, Wang X (2020) SIRT1 and aging related signaling pathways. Mech Ageing Dev 187. https://doi.org/10.1016/J.MAD.2020.111215
Tsai CH, Liu SC, Chung WH et al (2020) Visfatin increases VEGF-dependent angiogenesis of endothelial progenitor cells during osteoarthritis progression. Cells 9. https://doi.org/10.3390/CELLS9051315
Suzuki A, Yabu A, Nakamura H (2020) Advanced glycation end products in musculoskeletal system and disorders. Methods 203:179–186. https://doi.org/10.1016/j.ymeth.2020.09.012
Xie J, Méndez JD, Méndez-Valenzuela V, Aguilar-Hernández MM (2013) Cellular signalling of the receptor for advanced glycation end products (RAGE). Cell Signal 25:2185–2197
Lambert C, Zappia J, Sanchez C et al (2021) The damage-associated molecular patterns (DAMPs) as potential targets to treat osteoarthritis: perspectives from a review of the literature. Front Med 7
Motta F, Sica A, Selmi C (2020) Frailty in rheumatic diseases. Front Immunol 11
Fulop T, Larbi A, Pawelec G et al (2021) Immunology of aging: the birth of inflammaging. Clin Rev Allergy Immunol. https://doi.org/10.1007/S12016-021-08899-6
Franceschi C, Campisi J (2014) Chronic inflammation (Inflammaging) and its potential contribution to age-associated diseases. J Gerontol - Ser A Biol Sci Med Sci 69:S4–S9
Torre LA, Bray F, Siegel RL et al (2015) Global cancer statistics, 2012. CA Cancer J Clin 65:87–108. https://doi.org/10.3322/caac.21262
Kennedy BK, Berger SL, Brunet A et al (2014) Geroscience: linking aging to chronic disease. Cell 159:709–713
López-Otín C, Blasco MA, Partridge L et al (2013) The hallmarks of aging. Cell 153:1194
Finkel T, Holbrook NJ (2000) Oxidants, oxidative stress and the biology of ageing. Nature 408:239–247
Reuter S, Gupta SC, Chaturvedi MM, Aggarwal BB (2010) Oxidative stress, inflammation, and cancer: how are they linked? Free Radic. Biol Med 49:1603–1616
Sosa V, Moliné T, Somoza R et al (2013) Oxidative stress and cancer: an overview. Ageing Res Rev 12:376–390
Karunakaran U, Park KG (2013) A systematic review of oxidative stress and safety of antioxidants in diabetes: focus on islets and their defense. Diabetes Metab J 37:106–112
Pirillo A, Norata GD, Catapano AL (2013) LOX-1, OxLDL, and atherosclerosis. Mediators Inflamm. 2013
Yu W, Zhang H, Shin MR, Sesti F (2019) Oxidation of KCNB1 potassium channels in the murine brain during aging is associated with cognitive impairment. Biochem Biophys Res Commun 512:665–669. https://doi.org/10.1016/j.bbrc.2019.03.130
Liu Z, Zhou T, Ziegler AC et al (2017) Oxidative stress in neurodegenerative diseases: from molecular mechanisms to clinical applications. Oxid Med Cell Longev 2017
John-Schuster G, Günter S, Hager K et al (2016) Inflammaging increases susceptibility to cigarette smoke-induced COPD. Oncotarget 7:30068–30083. https://doi.org/10.18632/oncotarget.4027
Mateen S, Moin S, Khan AQ et al (2016) Increased reactive oxygen species formation and oxidative stress in rheumatoid arthritis. PLoS ONE 11. https://doi.org/10.1371/journal.pone.0152925
Li Y, Goronzy JJ, Weyand CM (2018) DNA damage, metabolism and aging in pro-inflammatory T cells: Rheumatoid arthritis as a model system. Exp Gerontol 105:118–127
Franceschi C, Bonafè M, Valensin S et al (2000) Inflammaging. An evolutionary perspective on immunosenescence. In: Annals of the New York Academy of Sciences. New York Academy of Sciences, pp 244–254
Vitale G, Salvioli S, Franceschi C (2013) Oxidative stress and the ageing endocrine system. Nat Rev Endocrinol 9:228–240
Fulop T, Witkowski JM, Olivieri F, Larbi A (2018) The integration of inflammaging in age-related diseases. Semin Immunol 40:17–35
Callender LA, Carroll EC, Beal RWJ et al (2018) Human CD8 + EMRA T cells display a senescence-associated secretory phenotype regulated by p38 MAPK. Aging Cell 17. https://doi.org/10.1111/acel.12675
Coppé JP, Patil CK, Rodier F et al (2008) Senescence-associated secretory phenotypes reveal cell-nonautonomous functions of oncogenic RAS and the p53 tumor suppressor. PLoS Biol 6. https://doi.org/10.1371/journal.pbio.0060301
Coppé JP, Desprez PY, Krtolica A, Campisi J (2010) The senescence-associated secretory phenotype: the dark side of tumor suppression. Annu Rev Pathol Mech Dis 5:99–118
Bleve A, Motta F, Durante B et al (2022) Immunosenescence, inflammaging, and frailty: role of myeloid cells in age-related diseases. Clin Rev Allergy Immunol. https://doi.org/10.1007/S12016-021-08909-7
Coder BD, Wang H, Ruan L, Su D-M (2015) Thymic involution perturbs negative selection leading to autoreactive t cells that induce chronic inflammation. J Immunol 194:5825–5837. https://doi.org/10.4049/jimmunol.1500082
Coder B, Su DM (2015) Thymic involution beyond T-cell insufficiency. Oncotarget 6:21777–21778
Brunner S, Herndler-Brandstetter D, Weinberger B, Grubeck-Loebenstein B (2011) Persistent viral infections and immune aging. Ageing Res Rev 10:362–369
Ebersole JL, Graves CL, Gonzalez OA et al (2000) (2016) Aging, inflammation, immunity and periodontal disease. Periodontol 72:54–75
Franceschi C, Garagnani P, Vitale G et al (2017) Inflammaging and ‘Garb-aging.’ Trends Endocrinol Metab 28:199–212
Lee B-J, Min C-K, Hancock M et al (2021) Human cytomegalovirus host interactions: EGFR and host cell signaling is a point of convergence between viral infection and functional changes in infected cells. Front Microbiol 12:660901. https://doi.org/10.3389/fmicb.2021.660901
Lohr JM, Oldstone MBA (1990) Detection of cytomegalovirus nucleic acid sequences in pancreas in type 2 diabetes. Lancet 336:644–648. https://doi.org/10.1016/0140-6736(90)92145-8
Donath MY, Shoelson SE (2011) Type 2 diabetes as an inflammatory disease. Nat Rev Immunol 11:98–107
Low H, Mukhamedova N, Cui HL et al (2016) Cytomegalovirus restructures lipid rafts via a US28/CDC42-mediated pathway, enhancing cholesterol efflux from host cells. Cell Rep 16:186–200. https://doi.org/10.1016/j.celrep.2016.05.070
Yu Y, Clippinger AJ, Alwine JC (2011) Viral effects on metabolism: changes in glucose and glutamine utilization during human cytomegalovirus infection. Trends Microbiol 19:360–367
Hotamisligil GS (2006) Inflammation and metabolic disorders. Nature 444:860–867
Ye J, Keller JN (2010) Regulation of energy metabolism by inflammation: a feedback response in obesity and calorie restriction. Aging (Albany NY) 2:361–368. https://doi.org/10.18632/aging.100155
Collino S, Montoliu I, Martin F-PJ et al (2013) Correction: metabolic signatures of extreme longevity in Northern Italian centenarians reveal a complex remodeling of lipids, amino acids, and gut microbiota metabolism. PLoS ONE 8. https://doi.org/10.1371/annotation/5fb9fa6f-4889-4407-8430-6dfc7ecdfbdd
Biagi E, Nylund L, Candela M et al (2010) Through ageing, and beyond: gut microbiota and inflammatory status in seniors and centenarians. PLoS ONE 5. https://doi.org/10.1371/journal.pone.0010667
Biagi E, Candela M, Franceschi C, Brigidi P (2011) The aging gut microbiota: new perspectives. Ageing Res Rev 10:428–429
Cevenini E, Monti D, Franceschi C (2013) Inflamm-ageing. Curr Opin Clin Nutr Metab Care 16:14–20
Biagi E, Franceschi C, Rampelli S et al (2016) Gut microbiota and extreme longevity. Curr Biol 26:1480–1485. https://doi.org/10.1016/j.cub.2016.04.016
Franceschi C, Salvioli S, Garagnani P et al (2017) Immunobiography and the heterogeneity of immune responses in the elderly: a focus on inflammaging and trained immunity. Front Immunol 8
Santoro A, Ostan R, Candela M et al (2018) Gut microbiota changes in the extreme decades of human life: a focus on centenarians. Cell Mol Life Sci 75:129–148
Kundu P, Blacher E, Elinav E, Pettersson S (2017) Our gut microbiome: the evolving inner self. Cell 171:1481–1493
Lee C, Longo V (2016) Dietary restriction with and without caloric restriction for healthy aging. F1000Research 5
Barzilai N, Huffman DM, Muzumdar RH, Bartke A (2012) The critical role of metabolic pathways in aging. Diabetes 61:1315–1322
Ristow M, Schmeisser K (2014) Mitohormesis: promoting health and lifespan by increased levels of reactive oxygen species (ROS). Dose-Response 12:288–341. https://doi.org/10.2203/dose-response.13-035.Ristow
Das SK, Balasubramanian P, Weerasekara YK (2017) Nutrition modulation of human aging: the calorie restriction paradigm. Mol Cell Endocrinol 455:148–157. https://doi.org/10.1016/j.mce.2017.04.011
Mirzaei H, Suarez JA, Longo VD (2014) Protein and amino acid restriction, aging and disease: from yeast to humans. Trends Endocrinol Metab 25:558–566
Loeser RF, Olex AL, McNulty MA et al (2012) Microarray analysis reveals age-related differences in gene expression during the development of osteoarthritis in mice. Arthritis Rheum 64:705–717. https://doi.org/10.1002/ART.33388
Long D, Blake S, Song XY et al (2008) Human articular chondrocytes produce IL-7 and respond to IL-7 with increased production of matrix metalloproteinase-13. Arthritis Res Ther 10. https://doi.org/10.1186/AR2376
Rezuș E, Cardoneanu A, Burlui A et al (2019) The link between inflammaging and degenerative joint diseases. Int J Mol Sci 20. https://doi.org/10.3390/IJMS20030614
Millerand M, Berenbaum F, Jacques C (2019) Danger signals and inflammaging in osteoarthritis. Clin Exp Rheumatol 37:48–56
Goekoop RJ, Kloppenburg M, Kroon HM et al (2010) Low innate production of interleukin-1β and interleukin-6 is associated with the absence of osteoarthritis in old age. Osteoarthr Cartil 18:942–947. https://doi.org/10.1016/j.joca.2010.03.016
Ni Z, Kuang L, Chen H et al (2019) The exosome-like vesicles from osteoarthritic chondrocyte enhanced mature IL-1β production of macrophages and aggravated synovitis in osteoarthritis. Cell Death Dis 10. https://doi.org/10.1038/s41419-019-1739-2
Kato T, Miyaki S, Ishitobi H et al (2014) Exosomes from IL-1β stimulated synovial fibroblasts induce osteoarthritic changes in articular chondrocytes. Arthritis Res Ther 16. https://doi.org/10.1186/ar4679
Chien SY, Tsai CH, Liu SC et al (2020) Noggin inhibits IL-1β and BMP-2 expression, and attenuates cartilage degeneration and subchondral bone destruction in experimental osteoarthritis. Cells 9. https://doi.org/10.3390/cells9040927
Nasi S, So A, Combes C et al (2016) Interleukin-6 and chondrocyte mineralisation act in tandem to promote experimental osteoarthritis. Ann Rheum Dis 75:1372–1379. https://doi.org/10.1136/annrheumdis-2015-207487
Loeser RF, Collins JA, Diekman BO (2016) Ageing and the pathogenesis of osteoarthritis. Nat Rev Rheumatol 12:412–420
Jeon H, Il IG (2017) Autophagy in osteoarthritis. Connect Tissue Res 58:497–508. https://doi.org/10.1080/03008207.2016.1240790
Gao T, Guo W, Chen M et al (2016) Extracellular vesicles and autophagy in osteoarthritis. Biomed Res Int 2016. https://doi.org/10.1155/2016/2428915
Ponchel F, Burska AN, Hensor EMA et al (2015) Changes in peripheral blood immune cell composition in osteoarthritis. Osteoarthr Cartil 23:1870–1878. https://doi.org/10.1016/j.joca.2015.06.018
Zhu W, Zhang X, Jiang Y et al (2020) Alterations in peripheral T cell and B cell subsets in patients with osteoarthritis. Clin Rheumatol 39:523–532. https://doi.org/10.1007/s10067-019-04768-y
Shan Y, Qi C, Liu Y et al (2017) Increased frequency of peripheral blood follicular helper T cells and elevated serum IL-21 levels in patients with knee osteoarthritis. Mol Med Rep 15:1095–1102. https://doi.org/10.3892/mmr.2017.6132
de Lange-Brokaar BJE, Ioan-Facsinay A, van Osch GJVM et al (2012) Synovial inflammation, immune cells and their cytokines in osteoarthritis: a review. Osteoarthr Cartil 20:1484–1499. https://doi.org/10.1016/J.JOCA.2012.08.027
Pessler F, Chen LX, Dai L et al (2008) A histomorphometric analysis of synovial biopsies from individuals with Gulf War Veterans’ illness and joint pain compared to normal and osteoarthritis synovium. Clin Rheumatol 27:1127–1134. https://doi.org/10.1007/S10067-008-0878-0
Mikolajczyk TP, Nosalski R, Szczepaniak P et al (2016) Role of chemokine RANTES in the regulation of perivascular inflammation, T-cell accumulation, and vascular dysfunction in hypertension. FASEB J 30:1987–1999. https://doi.org/10.1096/fj.201500088R
Lopes EBP, Filiberti A, Husain SA, Humphrey MB (2017) Immune contributions to osteoarthritis. Curr Osteoporos Rep 15:593–600. https://doi.org/10.1007/S11914-017-0411-Y
Siebuhr AS, Bay-Jensen AC, Jordan JM et al (2016) Inflammation (or synovitis)-driven osteoarthritis: an opportunity for personalizing prognosis and treatment? Scand J Rheumatol 45:87–98
Fried LP, Tangen CM, Walston J et al (2001) Frailty in older adults: evidence for a phenotype. J Gerontol - Ser A Biol Sci Med Sci 56. https://doi.org/10.1093/gerona/56.3.m146
Kojima G, Liljas AEM, Iliffe S (2019) Frailty syndrome: implications and challenges for health care policy. Risk Manag Healthc Policy 12:23–30
Ferrucci L, Fabbri E (2018) Inflammageing: chronic inflammation in ageing, cardiovascular disease, and frailty. Nat Rev Cardiol 15:505–522
Motta F, Sica A, Selmi C (2020) Frailty in rheumatic diseases. Front Immunol 11. https://doi.org/10.3389/FIMMU.2020.576134
Cacciatore F, Della-morte D, Basile C et al (2014) Long-term mortality in frail elderly subjects with osteoarthritis. Rheumatology (Oxford) 53:293–299. https://doi.org/10.1093/RHEUMATOLOGY/KET348
Chen P, Huang L, Ma Y et al (2019) Intra-articular platelet-rich plasma injection for knee osteoarthritis: a summary of meta-analyses. J Orthop Surg Res 14. https://doi.org/10.1186/s13018-019-1363-y
Le ADK, Enweze L, DeBaun MR, Dragoo JL (2019) Platelet-rich plasma. Clin Sports Med 38:17–44. https://doi.org/10.1016/J.CSM.2018.08.001
Spreafico A, Chellini F, Frediani B et al (2009) Biochemical investigation of the effects of human platelet releasates on human articular chondrocytes. J Cell Biochem 108:1153–1165. https://doi.org/10.1002/JCB.22344
Smyth NA, Murawski CD, Fortier LA et al (2013) Platelet-rich plasma in the pathologic processes of cartilage: review of basic science evidence. Arthroscopy 29:1399–1409. https://doi.org/10.1016/J.ARTHRO.2013.03.004
Battaglia M, Guaraldi F, Vannini F et al (2013) Efficacy of ultrasound-guided intra-articular injections of platelet-rich plasma versus hyaluronic acid for hip osteoarthritis. Orthopedics 36. https://doi.org/10.3928/01477447-20131120-13
Dallari D, Stagni C, Rani N et al (2016) Ultrasound-guided injection of platelet-rich plasma and hyaluronic acid, separately and in combination, for hip osteoarthritis: a randomized controlled study. Am J Sports Med 44:664–671. https://doi.org/10.1177/0363546515620383
Doria C, Mosele GR, Caggiari G et al (2017) Treatment of early hip osteoarthritis: ultrasound-guided platelet rich plasma versus hyaluronic acid injections in a randomized clinical trial. Joints 5:152–155. https://doi.org/10.1055/S-0037-1605584
Di Sante L, Villani C, Santilli V et al (2016) Intra-articular hyaluronic acid vs platelet-rich plasma in the treatment of hip osteoarthritis. Med Ultrason 18:463–468. https://doi.org/10.11152/MU-874
Hamilton JA, Cook AD, Tak PP (2016) Anti-colony-stimulating factor therapies for inflammatory and autoimmune diseases. Nat Rev Drug Discov 16:53–70. https://doi.org/10.1038/NRD.2016.231
Lee KMC, Prasad V, Achuthan A et al (2020) Targeting GM-CSF for collagenase-induced osteoarthritis pain and disease in mice. Osteoarthr Cartil 28:486–491. https://doi.org/10.1016/j.joca.2020.01.012
Cook AD, Pobjoy J, Steidl S et al (2012) Granulocyte-macrophage colony-stimulating factor is a key mediator in experimental osteoarthritis pain and disease development. Arthritis Res Ther 14. https://doi.org/10.1186/AR4037
Steen-Louws C, Popov-Celeketic J, Mastbergen SC et al (2018) IL4-10 fusion protein has chondroprotective, anti-inflammatory and potentially analgesic effects in the treatment of osteoarthritis. Osteoarthr Cartil 26:1127–1135. https://doi.org/10.1016/j.joca.2018.05.005
van Helvoort EM, de Visser HM, Lafeber FPJG et al (2021) IL4-10 fusion protein shows DMOAD activity in a rat osteoarthritis model. Cartilage 13:1155S-1164S. https://doi.org/10.1177/19476035211026736
Hwang HS, Park IY, Choi SY, Kim HA (2017) PEP-1-GRX-1 modulates matrix metalloproteinase-13 and nitric oxide expression of human articular chondrocytes. Cell Physiol Biochem 41:252–264. https://doi.org/10.1159/000456090
Bin ZH, Zhang Y, Chen C et al (2016) Pioglitazone inhibits advanced glycation end product-induced matrix metalloproteinases and apoptosis by suppressing the activation of MAPK and NF-κB. Apoptosis 21:1082–1093. https://doi.org/10.1007/s10495-016-1280-z
Campo GM, Avenoso A, D’Ascola A et al (2012) Hyaluronan differently modulates TLR-4 and the inflammatory response in mouse chondrocytes. BioFactors 38:69–76. https://doi.org/10.1002/biof.202
Li Y, Zhang Y, Chen C et al (2016) Establishment of a rabbit model to study the influence of advanced glycation end products accumulation on osteoarthritis and the protective effect of pioglitazone. Osteoarthr Cartil 24:307–314. https://doi.org/10.1016/J.JOCA.2015.08.001
Boileau C, Martel-Pelletier J, Fahmi H et al (2007) The peroxisome proliferator-activated receptor gamma agonist pioglitazone reduces the development of cartilage lesions in an experimental dog model of osteoarthritis: in vivo protective effects mediated through the inhibition of key signaling and catabolic pathways. Arthritis Rheum 56:2288–2298. https://doi.org/10.1002/ART.22726
Kobayashi T, Notoya K, Naito T et al (2005) Pioglitazone, a peroxisome proliferator-activated receptor gamma agonist, reduces the progression of experimental osteoarthritis in guinea pigs. Arthritis Rheum 52:479–487. https://doi.org/10.1002/ART.20792
Chayanupatkul M, Honsawek S (2010) Soluble receptor for advanced glycation end products (sRAGE) in plasma and synovial fluid is inversely associated with disease severity of knee osteoarthritis. Clin Biochem 43:1133–1137. https://doi.org/10.1016/j.clinbiochem.2010.07.007
Peng Y, Park HS, Tang LA et al (2019) Generation of sRAGE high transgenic mice to study inflammaging. Front Biosci - Landmark 24:555–563. https://doi.org/10.2741/4735
Luo Y, Li J, Wang B et al (2021) Protective effect of glycyrrhizin on osteoarthritis cartilage degeneration and inflammation response in a rat model. J Bioenerg Biomembr 53:285–293. https://doi.org/10.1007/S10863-021-09889-1
Olcum M, Tufekci KU, Durur DY et al (2021) Ethyl Ethyl pyruvate attenuates microglial NLRP3 inflammasome activation via inhibition of HMGB1/NF-κB/miR-223 signaling. Antioxidants (Basel, Switzerland) 10. https://doi.org/10.3390/ANTIOX10050745
Luo Y, Li J, Wang B et al (2021) Protective effect of glycyrrhizin on osteoarthritis cartilage degeneration and inflammation response in a rat model. J Bioenerg Biomembr 53. https://doi.org/10.1007/s10863-021-09889-1
Li S, Liang F, Kwan K et al (2018) Identification of ethyl pyruvate as a NLRP3 inflammasome inhibitor that preserves mitochondrial integrity. Mol Med 24. https://doi.org/10.1186/s10020-018-0006-9
Xue J, Suarez JS, Minaai M et al (2021) HMGB1 as a therapeutic target in disease. J Cell Physiol 236:3406–3419
Aulin C, Lassacher T, Palmblad K, Erlandsson Harris H (2020) Early stage blockade of the alarmin HMGB1 reduces cartilage destruction in experimental OA. Osteoarthr Cartil 28:698–707. https://doi.org/10.1016/j.joca.2020.01.003
Schelbergen RF, Geven EJ, Van Den Bosch MHJ et al (2015) Prophylactic treatment with S100A9 inhibitor paquinimod reduces pathology in experimental collagenase-induced osteoarthritis. Ann Rheum Dis 74:2254–2258. https://doi.org/10.1136/annrheumdis-2014-206517
Van Den Bosch MH, Blom AB, Schelbergen RF et al (2016) Alarmin S100A9 induces proinflammatory and catabolic effects predominantly in the M1 macrophages of human osteoarthritic synovium. J Rheumatol 43:1874–1884. https://doi.org/10.3899/jrheum.160270
van den Bosch MHJ (2019) Inflammation in osteoarthritis: is it time to dampen the alarm(in) in this debilitating disease? Clin Exp Immunol 195:153–166
Cremers NAJ, van den Bosch MHJ, van Dalen S et al (2017) S100A8/A9 increases the mobilization of pro-inflammatory Ly6Chigh monocytes to the synovium during experimental osteoarthritis. Arthritis Res Ther 19. https://doi.org/10.1186/s13075-017-1426-6
Jeon OH, Kim C, Laberge RM et al (2017) Local clearance of senescent cells attenuates the development of post-traumatic osteoarthritis and creates a pro-regenerative environment. Nat Med 23:775–781. https://doi.org/10.1038/nm.4324
Bay-Jensen AC, Mobasheri A, Thudium CS et al (2022) Blood and urine biomarkers in osteoarthritis - an update on cartilage associated type II collagen and aggrecan markers. Curr Opin Rheumatol 34:54–60. https://doi.org/10.1097/BOR.0000000000000845
Kraus VB, Collins JE, Hargrove D et al (2017) Predictive validity of biochemical biomarkers in knee osteoarthritis: data from the FNIH OA Biomarkers Consortium. Ann Rheum Dis 76:186–195. https://doi.org/10.1136/ANNRHEUMDIS-2016-209252
Luo Y, He Y, Reker D et al (2018) A novel high sensitivity type II collagen blood-based biomarker, PRO-C2, for assessment of cartilage formation. Int J Mol Sci 19. https://doi.org/10.3390/IJMS19113485
Siebuhr AS, Bay-Jensen AC, Leeming DJ et al (2013) Serological identification of fast progressors of structural damage with rheumatoid arthritis. Arthritis Res Ther 15. https://doi.org/10.1186/AR4266
Goldring MB, Goldring SR (2010) Articular cartilage and subchondral bone in the pathogenesis of osteoarthritis. Ann N Y Acad Sci 1192:230–237. https://doi.org/10.1111/J.1749-6632.2009.05240.X
Huebner JL, Bay-Jensen AC, Huffman KM et al (2014) Alpha C-telopeptide of type I collagen is associated with subchondral bone turnover and predicts progression of joint space narrowing and osteophytes in osteoarthritis. Arthritis Rheumatol (Hoboken, NJ) 66:2440–2449. https://doi.org/10.1002/ART.38739
Engbersen M, Huang ZKV (2016) Bone biomarkers related to osteoarthritis. In: Preedy V (ed) Biomarkers in disease: methods, discoveries and applications. Dordrecht
Haraden CA, Huebner JL, Hsueh MF et al (2019) Synovial fluid biomarkers associated with osteoarthritis severity reflect macrophage and neutrophil related inflammation. Arthritis Res Ther 21. https://doi.org/10.1186/S13075-019-1923-X
Hsueh MF, Zhang X, Wellman SS et al (2021) Synergistic roles of macrophages and neutrophils in osteoarthritis progression. Arthritis Rheumatol (Hoboken, NJ) 73:89–99. https://doi.org/10.1002/ART.41486
Sunahori K, Yamamura M, Yamana J et al (2006) The S100A8/A9 heterodimer amplifies proinflammatory cytokine production by macrophages via activation of nuclear factor kappa B and p38 mitogen-activated protein kinase in rheumatoid arthritis. Arthritis Res Ther 8. https://doi.org/10.1186/AR1939
Van Lent PLEM, Blom AB, Schelbergen RFP et al (2012) Active involvement of alarmins S100A8 and S100A9 in the regulation of synovial activation and joint destruction during mouse and human osteoarthritis. Arthritis Rheum 64:1466–1476. https://doi.org/10.1002/ART.34315
Swindell WR, Johnston A, Xing X et al (2013) Robust shifts in S100a9 expression with aging: a novel mechanism for chronic inflammation. Sci Rep 3. https://doi.org/10.1038/SREP01215
Gerss J, Roth J, Holzinger D et al (2012) Phagocyte-specific S100 proteins and high-sensitivity C reactive protein as biomarkers for a risk-adapted treatment to maintain remission in juvenile idiopathic arthritis: a comparative study. Ann Rheum Dis 71:1991–1997. https://doi.org/10.1136/ANNRHEUMDIS-2012-201329
Choi IY, Gerlag DM, Herenius MJ et al (2015) MRP8/14 serum levels as a strong predictor of response to biological treatments in patients with rheumatoid arthritis. Ann Rheum Dis 74:499–505. https://doi.org/10.1136/ANNRHEUMDIS-2013-203923
Holzinger D, Nippe N, Vogl T et al (2014) Myeloid-related proteins 8 and 14 contribute to monosodium urate monohydrate crystal-induced inflammation in gout. Arthritis Rheumatol (Hoboken, NJ) 66:1327–1339. https://doi.org/10.1002/ART.38369
Funding
FM, AS, and CS were funded by the Italian Ministry of Health (Ricerca Corrente and grant RF-2016–02364842).
Author information
Authors and Affiliations
Contributions
Both FM and CS conceived the idea for the paper. FM and EB performed the literature search and drafted the manuscript. CS and AS provided helpful suggestions in the preparation of this manuscript, and all the authors reviewed and approved the final version of the paper.
Corresponding author
Ethics declarations
Ethics Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Motta, F., Barone, E., Sica, A. et al. Inflammaging and Osteoarthritis. Clinic Rev Allerg Immunol 64, 222–238 (2023). https://doi.org/10.1007/s12016-022-08941-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12016-022-08941-1