Abstract
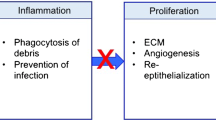
Mast cells (MCs), apart from their classic role in allergy, contribute to a number of biologic processes including wound healing. In particular, two aspects of their histologic distribution within the skin have attracted the attention of researchers to study their wound healing role; they represent up to 8% of the total number of cells within the dermis and their cutaneous versions are localized adjacent to the epidermis and the subdermal vasculature and nerves. At the onset of a cutaneous injury, the accumulation of MCs and release of proinflammatory and immunomodulatory mediators have been well documented. The role of MC-derived mediators has been investigated through the stages of wound healing including inflammation, proliferation, and remodeling. They contribute to hemostasis and clot formation by enhancing the expression of factor XIIIa in dermal dendrocytes through release of TNF-α, and contribute to clot stabilization. Keratinocytes, by secreting stem cell factor (SCF), recruit MCs to the site. MCs in return release inflammatory mediators, including predominantly histamine, VEGF, interleukin (IL)-6, and IL-8, that contribute to increase of endothelial permeability and vasodilation, and facilitate migration of inflammatory cells, mainly monocytes and neutrophils to the site of injury. MCs are capable of activating the fibroblasts and keratinocytes, the predominant cells involved in wound healing. MCs stimulate fibroblast proliferation during the proliferative phase via IL-4, vascular endothelial growth factor (VEGF), and basic fibroblast growth factor (bFGF) to produce a new extracellular matrix (ECM). MC-derived mediators including fibroblast growth factor-2, VEGF, platelet-derived growth factor (PDGF), TGF-β, nerve growth factor (NGF), IL-4, and IL-8 contribute to neoangiogenesis, fibrinogenesis, or reepithelialization during the repair process. MC activation inhibition and targeting the MC-derived mediators are potential therapeutic strategies to improve wound healing through reduced inflammatory responses and scar formation.






Similar content being viewed by others
Abbreviations
- bFGF:
-
Basic fibroblast growth factor
- ECM:
-
Extracellular matrix
- FGF:
-
Fibroblast growth factor
- IGF:
-
Insulin-like growth factor
- KGF:
-
Keratinocyte growth factor
- MC:
-
Mast cell
- MCP-1:
-
Monocyte chemoattractant protein-1
- MIP-2:
-
Macrophage inflammatory protein-2
- MMP:
-
Matrix metalloproteinases
- PAI-1:
-
Plasminogen activator inhibitor 1
- PDGF:
-
Platelet-derived growth factor
- SCF:
-
Stem cell factor
- TGF-β:
-
Transforming growth factor β
- t-PA:
-
Tissue-type plasminogen activator
- VEGF:
-
Vascular endothelial growth factor
References
Schultz GS, Davidson JM, Kirsner RS, Bornstein P, Herman IM (2011) Dynamic reciprocity in the wound microenvironment. Wound Repair Regen 19(2):134–148. https://doi.org/10.1111/j.1524-475X.2011.00673.x
Brugues A, Anon E, Conte V, Veldhuis JH, Gupta M, Colombelli J, Munoz JJ, Brodland GW, Ladoux B, Trepat X (2014) Forces driving epithelial wound healing. Nat Phys 10(9):683–690. https://doi.org/10.1038/nphys3040
Wulff BC, Wilgus TA (2013) Mast cell activity in the healing wound: more than meets the eye? Exp Dermatol 22(8):507–510. https://doi.org/10.1111/exd.12169
Noli C, Miolo A (2001) The mast cell in wound healing. Vet Dermatol 12(6):303–313
Chen L, DiPietro LA (2017) Toll-like receptor function in acute wounds. Adv Wound Care 6(10):344–355. https://doi.org/10.1089/wound.2017.0734
Das A, Dickerson R, Ghatak PD, Gordillo GM, Chaffee S, Saha A, Khanna S, Roy S (2018) May dietary supplementation augment respiratory burst in wound-site inflammatory cells? Antioxid Redox Signal 28(5):401–405. https://doi.org/10.1089/ars.2017.7304
Berksoy Hayta S, Durmus K, Altuntas EE, Yildiz E, Hisarciklio M, Akyol M (2018) The reduction in inflammation and impairment in wound healing by using strontium chloride hexahydrate. Cutan Ocul Toxicol 37(1):24–28. https://doi.org/10.1080/15569527.2017.1326497
Sun L, Gao W, Fu X, Shi M, Xie W, Zhang W, Zhao F, Chen X (2017) Enhanced wound healing in diabetic rats by nanofibrous scaffolds mimicking the basketweave pattern of collagen fibrils in native skin. Biomater Sci 6:340–349. https://doi.org/10.1039/c7bm00545h
Tracy LE, Minasian RA, Caterson EJ (2016) Extracellular matrix and dermal fibroblast function in the healing wound. Adv Wound Care 5(3):119–136. https://doi.org/10.1089/wound.2014.0561
Yeh CJ, Chen CC, Leu YL, Lin MW, Chiu MM, Wang SH (2017) The effects of artocarpin on wound healing: in vitro and in vivo studies. Sci Rep 7(1):15599. https://doi.org/10.1038/s41598-017-15876-7
Adamson R (2009) Role of macrophages in normal wound healing: an overview. J Wound Care 18(8):349–351. https://doi.org/10.12968/jowc.2009.18.8.43636
Martin P, D'Souza D, Martin J, Grose R, Cooper L, Maki R, McKercher SR (2003) Wound healing in the PU.1 null mouse--tissue repair is not dependent on inflammatory cells. Curr Biol: CB 13(13):1122–1128
Yan J, Tie G, Wang S, Tutto A, DeMarco N, Khair L, Fazzio TG, Messina LM (2018) Diabetes impairs wound healing by Dnmt1-dependent dysregulation of hematopoietic stem cells differentiation towards macrophages. Nat Commun 9(1):33. https://doi.org/10.1038/s41467-017-02425-z
Artuc M, Hermes B, Steckelings UM, Grutzkau A, Henz BM (1999) Mast cells and their mediators in cutaneous wound healing--active participants or innocent bystanders? Exp Dermatol 8(1):1–16
Au SR, Au K, Saggers GC, Karne N, Ehrlich HP (2007) Rat mast cells communicate with fibroblasts via gap junction intercellular communications. J Cell Biochem 100(5):1170–1177. https://doi.org/10.1002/jcb.21107
Komi DEA, Rambasek T, Wohrl S (2017) Mastocytosis: from a molecular point of view. https://doi.org/10.1007/s12016-017-8619-2
Elieh Ali Komi D, Grauwet K (2017) Role of mast cells in regulation of T cell responses in experimental and clinical settings. Clin Rev Allergy Immunol 54:432–445. https://doi.org/10.1007/s12016-017-8646-z
Elieh-Ali-Komi D, Cao Y (2017) Role of mast cells in the pathogenesis of multiple sclerosis and experimental autoimmune encephalomyelitis. Clin Rev Allergy Immunol 52(3):436–445. https://doi.org/10.1007/s12016-016-8595-y
Elieh Ali Komi D, Bjermer L (2018) Mast cell-mediated orchestration of the immune responses in human allergic asthma: current insights. Clin Rev Allergy Immunol. https://doi.org/10.1007/s12016-018-8720-1
Elieh Ali Komi D, Rambasek T, Bielory L (2017) Clinical implications of mast cell involvement in allergic conjunctivitis. Allergy 73:528–539. https://doi.org/10.1111/all.13334
Wilgus TA, Wulff BC (2014) The importance of mast cells in dermal scarring. Adv Wound Care 3(4):356–365. https://doi.org/10.1089/wound.2013.0457
Huttunen M, Aalto ML, Harvima RJ, Horsmanheimo M, Harvima IT (2000) Alterations in mast cells showing tryptase and chymase activity in epithelializating and chronic wounds. Exp Dermatol 9(4):258–265
Fukuoka Y, Hite MR, Dellinger AL, Schwartz LB (2013) Human skin mast cells express complement factors C3 and C5. J Immunol (Baltimore, Md: 1950) 191(4):1827–1834. https://doi.org/10.4049/jimmunol.1202889
Bowser C, Erstein DP, Silverberg JI, Nowakowski M, Joks R (2010) Correlation of plasma complement split product levels with allergic respiratory disease activity and relation to allergen immunotherapy. Ann Allergy Asthma Immunol 104(1):42–49. https://doi.org/10.1016/j.anai.2009.11.021
Oskeritzian CA, Zhao W, Min HK, Xia HZ, Pozez A, Kiev J, Schwartz LB (2005) Surface CD88 functionally distinguishes the MCTC from the MCT type of human lung mast cell. J Allergy Clin Immunol 115(6):1162–1168. https://doi.org/10.1016/j.jaci.2005.02.022
Weisel JW (2005) Fibrinogen and fibrin. Adv Protein Chem 70:247–299. https://doi.org/10.1016/s0065-3233(05)70008-5
Hartmann K, Henz BM, Kruger-Krasagakes S, Kohl J, Burger R, Guhl S, Haase I, Lippert U, Zuberbier T (1997) C3a and C5a stimulate chemotaxis of human mast cells. Blood 89(8):2863–2870
Wojta J, Kaun C, Zorn G, Ghannadan M, Hauswirth AW, Sperr WR, Fritsch G, Printz D, Binder BR, Schatzl G, Zwirner J, Maurer G, Huber K, Valent P (2002) C5a stimulates production of plasminogen activator inhibitor-1 in human mast cells and basophils. Blood 100(2):517–523
Oschatz C, Maas C, Lecher B, Jansen T, Bjorkqvist J, Tradler T, Sedlmeier R, Burfeind P, Cichon S, Hammerschmidt S, Muller-Esterl W, Wuillemin WA, Nilsson G, Renne T (2011) Mast cells increase vascular permeability by heparin-initiated bradykinin formation in vivo. Immunity 34(2):258–268. https://doi.org/10.1016/j.immuni.2011.02.008
Yanase Y, Takahagi S, Hide M (2017) Chronic spontaneous urticaria and the extrinsic coagulation system. Allergol Int 67:191–194. https://doi.org/10.1016/j.alit.2017.09.003
Zhu H, Liang B, Li R, Li J, Lin L, Ma S, Wang J (2013) Activation of coagulation, anti-coagulation, fibrinolysis and the complement system in patients with urticaria. Asian Pac J Allergy Immunol 31(1):43–50
Kettelhut BV, Metcalfe DD (1991) Pediatric mastocytosis. J Investig Dermatol 96(3 Suppl):15S–18S; discussion 18S, 60S–65S. https://doi.org/10.1111/1523-1747.ep12468942
Gonzalo-Garijo MA, Perez-Rangel I, Alvarado-Izquierdo MI, Perez-Calderon R, Sanchez-Vega S, Zambonino MA (2010) Metrorrhagia as an uncommon symptom of anaphylaxis. J Investig Allergol Clin Immunol 20(6):540–541
Prieto-Garcia A, Castells MC, Hansbro PM, Stevens RL (2014) Mast cell-restricted tetramer-forming tryptases and their beneficial roles in hemostasis and blood coagulation. Immunol Allergy Clin N Am 34(2):263–281. https://doi.org/10.1016/j.iac.2014.01.001
Trautmann A, Toksoy A, Engelhardt E, Brocker EB, Gillitzer R (2000) Mast cell involvement in normal human skin wound healing: expression of monocyte chemoattractant protein-1 is correlated with recruitment of mast cells which synthesize interleukin-4 in vivo. J Pathol 190(1):100–106. https://doi.org/10.1002/(sici)1096-9896(200001)190:1<100::aid-path496>3.0.co;2-q
Gillitzer R, Goebeler M (2001) Chemokines in cutaneous wound healing. J Leukoc Biol 69(4):513–521
Ogle ME, Segar CE, Sridhar S, Botchwey EA (2016) Monocytes and macrophages in tissue repair: implications for immunoregenerative biomaterial design. Exp Biol Med (Maywood, NJ) 241(10):1084–1097. https://doi.org/10.1177/1535370216650293
Gordon JR (2000) Monocyte chemoattractant peptide-1 expression during cutaneous allergic reactions in mice is mast cell dependent and largely mediates the monocyte recruitment response. J Allergy Clin Immunol 106(1 Pt 1):110–116. https://doi.org/10.1067/mai.2000.107036
Li J, Chen J, Kirsner R (2007) Pathophysiology of acute wound healing. Clin Dermatol 25(1):9–18. https://doi.org/10.1016/j.clindermatol.2006.09.007
Egozi EI, Ferreira AM, Burns AL, Gamelli RL, Dipietro LA (2003) Mast cells modulate the inflammatory but not the proliferative response in healing wounds. Wound Repair Regen 11(1):46–54
Leoni G, Neumann PA, Sumagin R, Denning TL, Nusrat A (2015) Wound repair: role of immune-epithelial interactions. Mucosal Immunol 8(5):959–968. https://doi.org/10.1038/mi.2015.63
van der Veer WM, Bloemen MC, Ulrich MM, Molema G, van Zuijlen PP, Middelkoop E, Niessen FB (2009) Potential cellular and molecular causes of hypertrophic scar formation. Burns 35(1):15–29. https://doi.org/10.1016/j.burns.2008.06.020
Iba Y, Shibata A, Kato M, Masukawa T (2004) Possible involvement of mast cells in collagen remodeling in the late phase of cutaneous wound healing in mice. Int Immunopharmacol 4(14):1873–1880. https://doi.org/10.1016/j.intimp.2004.08.009
Theoharides TC, Alysandratos KD, Angelidou A, Delivanis DA, Sismanopoulos N, Zhang B, Asadi S, Vasiadi M, Weng Z, Miniati A, Kalogeromitros D (2012) Mast cells and inflammation. Biochim Biophys Acta 1822(1):21–33. https://doi.org/10.1016/j.bbadis.2010.12.014
Kennelly R, Conneely JB, Bouchier-Hayes D, Winter DC (2011) Mast cells in tissue healing: from skin to the gastrointestinal tract. Curr Pharm Des 17(34):3772–3775
Ng MF (2010) The role of mast cells in wound healing. Int Wound J 7(1):55–61. https://doi.org/10.1111/j.1742-481X.2009.00651.x
Ishikawa T, Kanda N, Hau CS, Tada Y, Watanabe S (2009) Histamine induces human beta-defensin-3 production in human keratinocytes. J Dermatol Sci 56(2):121–127. https://doi.org/10.1016/j.jdermsci.2009.07.012
Soliman M, Kim DS, Park JG, Kim JY, Alfajaro MM, Baek YB, Cho EH, Park CH, Kang MI, Park SI, Cho KO (2018) PI3K/Akt and MEK/ERK signaling pathways facilitate sapovirus trafficking and late endosomal acidification for viral uncoating in LLC-PK cells. J Virol 92. https://doi.org/10.1128/jvi.01674-18
Zhu C, Bao NR, Chen S, Zhao JN (2016) HBD-3 regulation of the immune response and the LPS/TLR4-mediated signaling pathway. Exp Ther Med 12(4):2150–2154. https://doi.org/10.3892/etm.2016.3579
Rohrl J, Yang D, Oppenheim JJ, Hehlgans T (2008) Identification and biological characterization of mouse beta-defensin 14, the orthologue of human beta-defensin 3. J Biol Chem 283(9):5414–5419. https://doi.org/10.1074/jbc.M709103200
Kasuya A, Tokura Y (2014) Attempts to accelerate wound healing. J Dermatol Sci 76(3):169–172. https://doi.org/10.1016/j.jdermsci.2014.11.001
Huttunen M, Hyttinen M, Nilsson G, Butterfield JH, Horsmanheimo M, Harvima IT (2001) Inhibition of keratinocyte growth in cell culture and whole skin culture by mast cell mediators. Exp Dermatol 10(3):184–192
Gruber BL (2003) Mast cells in the pathogenesis of fibrosis. Curr Rheumatol Rep 5(2):147–153
Yamamoto T, Hartmann K, Eckes B, Krieg T (2000) Mast cells enhance contraction of three-dimensional collagen lattices by fibroblasts by cell-cell interaction: role of stem cell factor/c-kit. Immunology 99(3):435–439
Yamamoto T, Hartmann K, Eckes B, Krieg T (2001) Role of stem cell factor and monocyte chemoattractant protein-1 in the interaction between fibroblasts and mast cells in fibrosis. J Dermatol Sci 26(2):106–111
Shiota N, Nishikori Y, Kakizoe E, Shimoura K, Niibayashi T, Shimbori C, Tanaka T, Okunishi H (2010) Pathophysiological role of skin mast cells in wound healing after scald injury: study with mast cell-deficient W/W(V) mice. Int Arch Allergy Immunol 151(1):80–88. https://doi.org/10.1159/000232573
Nauta AC, Grova M, Montoro DT, Zimmermann A, Tsai M, Gurtner GC, Galli SJ, Longaker MT (2013) Evidence that mast cells are not required for healing of splinted cutaneous excisional wounds in mice. PLoS One 8(3):e59167. https://doi.org/10.1371/journal.pone.0059167
Tellechea A, Leal EC, Kafanas A, Auster ME, Kuchibhotla S, Ostrovsky Y, Tecilazich F, Baltzis D, Zheng Y, Carvalho E, Zabolotny JM, Weng Z, Petra A, Patel A, Panagiotidou S, Pradhan-Nabzdyk L, Theoharides TC, Veves A (2016) Mast cells regulate wound healing in diabetes. Diabetes 65(7):2006–2019. https://doi.org/10.2337/db15-0340
Oskeritzian CA (2012) Mast cells and wound healing. Adv Wound Care 1(1):23–28. https://doi.org/10.1089/wound.2011.0357
Wilgus TA (2008) Immune cells in the healing skin wound: influential players at each stage of repair. Pharmacol Res 58(2):112–116. https://doi.org/10.1016/j.phrs.2008.07.009
Hiromatsu Y, Toda S (2003) Mast cells and angiogenesis. Microsc Res Tech 60(1):64–69. https://doi.org/10.1002/jemt.10244
Rao KN, Brown MA (2008) Mast cells: multifaceted immune cells with diverse roles in health and disease. Ann N Y Acad Sci 1143:83–104. https://doi.org/10.1196/annals.1443.023
Maltby S, Khazaie K, McNagny KM (2009) Mast cells in tumor growth: angiogenesis, tissue remodelling and immune-modulation. Biochim Biophys Acta 1796(1):19–26. https://doi.org/10.1016/j.bbcan.2009.02.001
Hinz B (2016) The role of myofibroblasts in wound healing. Curr Res Transl Med 64(4):171–177. https://doi.org/10.1016/j.retram.2016.09.003
Nishikori Y, Shiota N, Okunishi H (2014) The role of mast cells in cutaneous wound healing in streptozotocin-induced diabetic mice. Arch Dermatol Res 306(9):823–835. https://doi.org/10.1007/s00403-014-1496-0
Bagher M, Larsson-Callerfelt AK, Rosmark O, Hallgren O, Bjermer L, Westergren-Thorsson G (2018) Mast cells and mast cell tryptase enhance migration of human lung fibroblasts through protease-activated receptor 2. Cell Commun Signal 16(1):59. https://doi.org/10.1186/s12964-018-0269-3
Landolina N, Gangwar RS, Levi-Schaffer F (2015) Mast cells’ integrated actions with eosinophils and fibroblasts in allergic inflammation: implications for therapy. Adv Immunol 125:41–85. https://doi.org/10.1016/bs.ai.2014.09.002
Takeo M, Lee W, Ito M (2015) Wound healing and skin regeneration. Cold Spring Harbor Perspect Med 5(1):a023267. https://doi.org/10.1101/cshperspect.a023267
Glim JE, van Egmond M, Niessen FB, Everts V, Beelen RH (2013) Detrimental dermal wound healing: what can we learn from the oral mucosa? Wound Repair Regen 21(5):648–660. https://doi.org/10.1111/wrr.12072
Moyer KE, Saggers GC, Ehrlich HP (2004) Mast cells promote fibroblast populated collagen lattice contraction through gap junction intercellular communication. Wound Repair Regen 12(3):269–275. https://doi.org/10.1111/j.1067-1927.2004.012310.x
Ehrlich HP (2013) A snapshot of direct cell-cell communications in wound healing and scarring. Adv Wound Care 2(4):113–121. https://doi.org/10.1089/wound.2012.0414
Darby IA, Hewitson TD (2007) Fibroblast differentiation in wound healing and fibrosis. Int Rev Cytol 257:143–179. https://doi.org/10.1016/s0074-7696(07)57004-x
Wulff BC, Parent AE, Meleski MA, DiPietro LA, Schrementi ME, Wilgus TA (2012) Mast cells contribute to scar formation during fetal wound healing. J Investig Dermatol 132(2):458–465. https://doi.org/10.1038/jid.2011.324
Whitby DJ, Ferguson MW (1991) The extracellular matrix of lip wounds in fetal, neonatal and adult mice. Development 112(2):651–668
Glim JE, Beelen RH, Niessen FB, Everts V, Ulrich MM (2015) The number of immune cells is lower in healthy oral mucosa compared to skin and does not increase after scarring. Arch Oral Biol 60(2):272–281. https://doi.org/10.1016/j.archoralbio.2014.10.008
Natah SS, Hayrinen-Immonen R, Hietanen J, Malmstrom M, Konttinen YT (1998) Quantitative assessment of mast cells in recurrent aphthous ulcers (RAU). J Oral Pathol Med 27(3):124–129
Dong X, Xu T, Ma S, Wen H (2015) Expression and activity levels of chymase in mast cells of burn wound tissues increase during the healing process in a hamster model. Exp Ther Med 9(6):2190–2194. https://doi.org/10.3892/etm.2015.2424
Salmon-Ehr V, Ramont L, Godeau G, Birembaut P, Guenounou M, Bernard P, Maquart FX (2000) Implication of interleukin-4 in wound healing. Lab Investig 80(8):1337–1343
Succar J, Douaiher J, Lancerotto L, Li Q, Yamaguchi R, Younan G, Pejler G, Orgill DP (2014) The role of mouse mast cell proteases in the proliferative phase of wound healing in microdeformational wound therapy. Plast Reconstr Surg 134(3):459–467. https://doi.org/10.1097/prs.0000000000000432
Weller K, Foitzik K, Paus R, Syska W, Maurer M (2006) Mast cells are required for normal healing of skin wounds in mice. FASEB J 20(13):2366–2368. https://doi.org/10.1096/fj.06-5837fje
Lin L, Bankaitis E, Heimbach L, Li N, Abrink M, Pejler G, An L, Diaz LA, Werb Z, Liu Z (2011) Dual targets for mouse mast cell protease-4 in mediating tissue damage in experimental bullous pemphigoid. J Biol Chem 286(43):37358–37367. https://doi.org/10.1074/jbc.M111.272401
Honnegowda TM, Kumar P, Padmanabha Udupa EG, Kumar S, Kumar U, Rao P (2015) Role of angiogenesis and angiogenic factors in acute and chronic wound healing. Plast Aesthet Res 2:243–249. https://doi.org/10.4103/2347-9264.165438
Caughey GH (2007) Mast cell tryptases and chymases in inflammation and host defense. Immunol Rev 217:141–154. https://doi.org/10.1111/j.1600-065X.2007.00509.x
Gailit J, Marchese MJ, Kew RR, Gruber BL (2001) The differentiation and function of myofibroblasts is regulated by mast cell mediators. J Investig Dermatol 117(5):1113–1119. https://doi.org/10.1046/j.1523-1747.2001.15211.x
Kondo S, Kagami S, Kido H, Strutz F, Muller GA, Kuroda Y (2001) Role of mast cell tryptase in renal interstitial fibrosis. J Am Soc Nephrol 12(8):1668–1676
Li CY, Baek JY (2002) Mastocytosis and fibrosis: role of cytokines. Int Arch Allergy Immunol 127(2):123–126
Wygrecka M, Dahal BK, Kosanovic D, Petersen F, Taborski B, von Gerlach S, Didiasova M, Zakrzewicz D, Preissner KT, Schermuly RT, Markart P (2013) Mast cells and fibroblasts work in concert to aggravate pulmonary fibrosis: role of transmembrane SCF and the PAR-2/PKC-alpha/Raf-1/p44/42 signaling pathway. Am J Pathol 182(6):2094–2108. https://doi.org/10.1016/j.ajpath.2013.02.013
Jarbrink K, Ni G, Sonnergren H, Schmidtchen A, Pang C, Bajpai R, Car J (2016) Prevalence and incidence of chronic wounds and related complications: a protocol for a systematic review. 5(1):152. https://doi.org/10.1186/s13643-016-0329-y
Janssens AS, Heide R, den Hollander JC, Mulder PG, Tank B, Oranje AP (2005) Mast cell distribution in normal adult skin. J Clin Pathol 58(3):285–289. https://doi.org/10.1136/jcp.2004.017210
Huttunen M, Naukkarinen A, Horsmanheimo M, Harvima IT (2002) Transient production of stem cell factor in dermal cells but increasing expression of Kit receptor in mast cells during normal wound healing. Arch Dermatol Res 294(7):324–330. https://doi.org/10.1007/s00403-002-0331-1
Iemura A, Tsai M, Ando A, Wershil BK, Galli SJ (1994) The c-kit ligand, stem cell factor, promotes mast cell survival by suppressing apoptosis. Am J Pathol 144(2):321–328
Alm PE, Bloom GD, Hellstrom S, Stenfors LE, Widemar L (1983) Mast cells in the pars flaccida of the tympanic membrane. A quantitative morphological and biochemical study in the rat. Experientia 39(3):287–289
Widemar L, Hellstrom S, Stenfors LE, Bloom GD (1986) An overlooked site of tissue mast cells—the human tympanic membrane. Implications for middle ear affections. Acta Otolaryngol 102(5–6):391–395
Ichimiya I, Kawauchi H, Mogi G (1990) Analysis of immunocompetent cells in the middle ear mucosa. Arch Otolaryngol Head Neck Surg 116(3):324–330
Sankovic S, Dergenc R, Bojic P (2005) Mast cells in chronic inflammation of the middle ear mucosa. Rev Laryngol Otol Rhinol 126(1):15–18
Hurst DS, Amin K, Seveus L, Venge P (1999) Evidence of mast cell activity in the middle ears of children with otitis media with effusion. Laryngoscope 109(3):471–477
Griffin G, Flynn CA (2011) Antihistamines and/or decongestants for otitis media with effusion (OME) in children. Cochrane Database Syst Rev 9:Cd003423. https://doi.org/10.1002/14651858.CD003423.pub3
Schulz JN, Zeltz C, Sorensen IW, Barczyk M, Carracedo S, Hallinger R, Niehoff A, Eckes B, Gullberg D (2015) Reduced granulation tissue and wound strength in the absence of alpha11beta1 integrin. J Investig Dermatol 135(5):1435–1444. https://doi.org/10.1038/jid.2015.24
Olaso E, Lin HC, Wang LH, Friedman SL (2011) Impaired dermal wound healing in discoidin domain receptor 2-deficient mice associated with defective extracellular matrix remodeling. Fibrogenesis Tissue Repair 4(1):5. https://doi.org/10.1186/1755-1536-4-5
Jun JI, Lau LF (2010) The matricellular protein CCN1 induces fibroblast senescence and restricts fibrosis in cutaneous wound healing. Nat Cell Biol 12(7):676–685. https://doi.org/10.1038/ncb2070
Denton CP, Khan K, Hoyles RK, Shiwen X, Leoni P, Chen Y, Eastwood M, Abraham DJ (2009) Inducible lineage-specific deletion of TbetaRII in fibroblasts defines a pivotal regulatory role during adult skin wound healing. J Investig Dermatol 129(1):194–204. https://doi.org/10.1038/jid.2008.171
Kopecki Z, Luchetti MM, Adams DH, Strudwick X, Mantamadiotis T, Stoppacciaro A, Gabrielli A, Ramsay RG, Cowin AJ (2007) Collagen loss and impaired wound healing is associated with c-Myb deficiency. J Pathol 211(3):351–361. https://doi.org/10.1002/path.2113
Peters T, Sindrilaru A, Hinz B, Hinrichs R, Menke A, Al-Azzeh EA, Holzwarth K, Oreshkova T, Wang H, Kess D, Walzog B, Sulyok S, Sunderkotter C, Friedrich W, Wlaschek M, Krieg T, Scharffetter-Kochanek K (2005) Wound-healing defect of CD18(−/−) mice due to a decrease in TGF-beta1 and myofibroblast differentiation. EMBO J 24(19):3400–3410. https://doi.org/10.1038/sj.emboj.7600809
Al-Otaiby M, Tassi E, Schmidt MO, Chien CD, Baker T, Salas AG, Xu J, Furlong M, Schlegel R, Riegel AT, Wellstein A (2012) Role of the nuclear receptor coactivator AIB1/SRC-3 in angiogenesis and wound healing. Am J Pathol 180(4):1474–1484. https://doi.org/10.1016/j.ajpath.2011.12.032
Xu Z, Xu H, Ploplis VA, Castellino FJ (2010) Factor VII deficiency impairs cutaneous wound healing in mice. Mol Med 16(5–6):167–176. https://doi.org/10.2119/molmed.2009.00171
Geary SM, Cowin AJ, Copeland B, Baleato RM, Miyazaki K, Ashman LK (2008) The role of the tetraspanin CD151 in primary keratinocyte and fibroblast functions: implications for wound healing. Exp Cell Res 314(11–12):2165–2175. https://doi.org/10.1016/j.yexcr.2008.04.011
Bairy KL, Rao CM, Ramesh KV, Kulkarni DR (1991) Effects of antihistamines on wound healing. Indian J Exp Biol 29(4):398–399
Gallant-Behm CL, Hildebrand KA, Hart DA (2008) The mast cell stabilizer ketotifen prevents development of excessive skin wound contraction and fibrosis in red Duroc pigs. Wound Repair Regen 16(2):226–233. https://doi.org/10.1111/j.1524-475X.2008.00363.x
Chen L, Schrementi ME, Ranzer MJ, Wilgus TA, DiPietro LA (2014) Blockade of mast cell activation reduces cutaneous scar formation. PLoS One 9(1):e85226. https://doi.org/10.1371/journal.pone.0085226
Orenstein SB, Saberski ER, Klueh U, Kreutzer DL, Novitsky YW (2010) Effects of mast cell modulation on early host response to implanted synthetic meshes. Hernia 14(5):511–516. https://doi.org/10.1007/s10029-010-0680-1
Shah DR, Dholakia S, Shah RR (2014) Effect of tyrosine kinase inhibitors on wound healing and tissue repair: implications for surgery in cancer patients. Drug Saf 37(3):135–149. https://doi.org/10.1007/s40264-014-0139-x
Cheng C, Nayernama A, Christopher Jones S, Casey D, Waldron PE (2018) Wound healing complications with lenvatinib identified in a pharmacovigilance database. J Oncol Pharm Pract. https://doi.org/10.1177/1078155218817109
Younan G, Suber F, Xing W, Shi T, Kunori Y, Abrink M, Pejler G, Schlenner SM, Rodewald HR, Moore FD Jr, Stevens RL, Adachi R, Austen KF, Gurish MF (2010) The inflammatory response after an epidermal burn depends on the activities of mouse mast cell proteases 4 and 5. J Immunol 185(12):7681–7690. https://doi.org/10.4049/jimmunol.1002803
el Sayed SO, Dyson M (1993) Responses of dermal mast cells to injury. J Anat 182(Pt 3):369–376
Dorsett-Martin WA (2004) Rat models of skin wound healing: a review. Wound Repair Regen 12(6):591–599. https://doi.org/10.1111/j.1067-1927.2004.12601.x
Garner WL, Ehrlich HP (2011) Discussion: mast cells are required in the proliferation and remodeling phases of microdeformational wound therapy. Plast Reconstr Surg 128(6):659e–660e. https://doi.org/10.1097/PRS.0b013e318230bec1
Dong X, Geng Z, Zhao Y, Chen J, Cen Y (2013) Involvement of mast cell chymase in burn wound healing in hamsters. Exp Ther Medicine 5(2):643–647. https://doi.org/10.3892/etm.2012.836
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
No informed consent was required to prepare the manuscript.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Komi, D.E.A., Khomtchouk, K. & Santa Maria, P.L. A Review of the Contribution of Mast Cells in Wound Healing: Involved Molecular and Cellular Mechanisms. Clinic Rev Allerg Immunol 58, 298–312 (2020). https://doi.org/10.1007/s12016-019-08729-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12016-019-08729-w