Abstract
Intravenous immunoglobulin (IVIG) provides replacement therapy in immunodeficiency and immunomodulatory therapy in inflammatory and autoimmune diseases. This paper describes the immune mechanisms underlying six major non-primary immunodeficiency pediatric diseases and the diverse immunomodulatory functions of IVIG therapy. In Kawasaki disease, IVIG plays a major, proven, and effective role in decreasing aneurysm formation, which represents an aberrant inflammatory response to an infectious trigger in a genetically predisposed individual. In immune thrombocytopenia, IVIG targets the underlying increased platelet destruction and decreased platelet production. Although theoretically promising, IVIG shows no clear clinical benefit in the prophylaxis and treatment of neonatal sepsis. Limitations in research design combined with the unique neonatal immunologic environment offer explanations for this finding. Inflammation from aberrant immune activation underlies the myelinotoxic effects of Guillain-Barré syndrome. HIV-1 exerts a broad range of immunologic effects and was found to decrease serious bacterial infections in the pre-highly active anti-retroviral therapy (HAART) era, although its practical relevance in the post-HAART era has waned. Clinical and experimental data support the role of immune mechanisms in the pathogenesis of childhood epilepsy. IVIG exerts anti-epileptic effects through targeting upregulated cytokine pathways and antibodies thought to contribute to epilepsy. Applications in six additional pediatric diseases including pediatric asthma, atopic dermatitis, cystic fibrosis, pediatric autoimmune neuropsychiatric disorders associated with streptococcal infection (PANDAS), autism, and transplantation will also be briefly reviewed. From autoimmunity to immunodeficiency, a dynamic immunologic basis underlies major pediatric diseases and highlights the broad potential of IVIG therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Immunoglobulin replacement (Ig) therapy consists of pooled polyclonal IgG from thousands of healthy donors with broad applications. Commercial preparations of intravenous immunoglobulin (IVIG) contain >95 % IgG monomers with a small percentage of dimers, IgM, IgA, and other small proteins. Classically, IVIG provides replacement therapy in immunodeficiency and immunomodulatory therapy in many non-immunodeficiency diseases. Historically, the use of immunoglobulin replacement dates back to Colonel (Dr.) Ogden Bruton’s characterization of an inherited form of severe agammaglobulinemia that responded well to treatment with subcutaneous human serum globulin [1]. Yet, its history dates back to its applications in treating infectious disease, as reflected in the observation by von Behring and Kitasato in 1890 that immune sera can treat diphtheria and tetanus [2]. Currently, the FDA-approved indications for IVIG remain limited, although at least 75 % of IVIG in the USA is administered off-label for autoimmune or inflammatory conditions, most commonly neurologic diseases [3].
While the immunoglobulin replacement provided by IVIG is well defined, the anti-inflammatory and immunoregulatory functions of IVIG remain incompletely elucidated. Numerous studies have reported that IVIG has effects on B cells, antibodies, the complement system, T cell mechanisms, cell trafficking, and cytokine-based mechanisms [3, 4]. For inflammatory and autoimmune diseases, IVIG is often administered at doses four to five times those used in replacement therapy for immunodeficiency [3]. Speculation remains regarding whether the benefit of IVIG therapy in these contexts is direct or simply an observed “bystander” effect [5]. IVIG is effective in select autoimmune and inflammatory diseases, and different underlying disease mechanisms likely underly why some but not all autoimmune processes respond to IVIG. In some cases, the specific mechanisms of these autoimmune processes are still being elucidated. In other diseases, attention has shifted to the application of more targeted monoclonal antibody-based therapies.
Still, IVIG is often administered when conventional therapy fails or no alternative therapy exists, and mixed outcomes have been demonstrated across a wide range of diseases in which the etiology remains elusive. The applications of IVIG have expanded in both adult and pediatric diseases. Here, we seek to review the non-primary immune deficiency applications of IVIG in six major pediatric diseases, chosen due to their relevance to pediatrics. Specifically, we will explore the applications of IVIG in Kawasaki disease (KD), immune thrombocytopenia (ITP), Guillain-Barré syndrome (GBS), preterm and neonatal sepsis, pediatric HIV-1, and intractable childhood epilepsy (ICE). Other established indications for IVIG including chronic lymphocytic leukemia (CLL), autoimmune blistering diseases, inflammatory myopathies (dermatomyositis), and chronic inflammatory demyelinating polyradiculoneuropathy (CIPD) are predominantly adult diseases that are relatively rare in pediatric populations and omitted from specific discussion in this review. Here, we will briefly introduce each of the six diseases, the underlying immunologic dysfunction, and the mechanism of action underlying IVIG as a therapeutic. Applications of IVIG in six additional pediatric diseases including pediatric asthma, atopic dermatitis, cystic fibrosis, pediatric autoimmune neuropsychiatric disorders associated with streptococcal infection (PANDAS), autism, and transplantation are also briefly reviewed.
Kawasaki Disease
KD is an acute systemic vasculitis of childhood and the most common cause of acquired heart disease of children in developed countries [5]. The vasculitis involves the small- and medium-sized arteries, and symptoms include high fever, rash, cervical lymphadenopathy, conjunctivitis, and mucocutaneous changes. The most concerning life-long morbidity involves formation of ectasia or aneurysm of the coronary arteries [6]. The majority of children with KD are under 5 years old, with peak incidence between 18 and 24 months.
Immunologic Theories Behind KD
KD is believed to represent an aberrant inflammatory response to an infectious trigger in a genetically predisposed individual [6]. Activation of monocytes, macrophages, and inflammatory cytokines such as tumor necrosis alpha (TNF-α), interleukin (IL)-1, and IL-6 contributes largely to the inflammatory state characteristic of KD [6]. The influx of neutrophils characterizes the early stage, and resultant reactive oxygen species and other mediators also contribute to endothelial inflammation and resultant dysfunction [6, 7]. Specific Toll-like receptor agonists (such a TLR-2) contribute to the upregulation of co-stimulatory and inflammatory cytokines inducing coronary pathology in KD [7]. KD is also characterized by the presence of autoreactive anti-endothelial IgG and IgM antibodies that cause endothelial lysis when stimulated by TNF-α or IL-1 [8]. Monocytes, CD8+ T cells, and plasma cells infiltrate the coronary arterial wall leading to aneurysm formation [8]. While no single microbial entity has been identified, bacterial superantigens are suspected to play an etiologic role given the similar clinical mucocutaneous features shared between KD and staphylococcal and streptococcal-mediated disorders [5]. The overexpression of particular T lymphocyte receptor Vβ families is associated with a massive immune response in animal models suggesting differential predisposition toward inflammation [9]. Additionally, T regulatory cells (Treg) and FOXP3 mRNA gene expression appear significantly reduced in acute KD [10].
IVIG Treatment for KD
The American Heart Association recommends a single administration of 2 g/kg of IVIG within 5–10 days after onset of fever. A meta-analysis of large, randomized studies showed that IVIG and aspirin unequivocally shorten fever duration and reduce coronary artery aneurysm formation from 15 to 25 % in those untreated down to less than 5 % after treatment [8]. Still, approximately 10–20 % of patients experience the persistence or recurrence of fever. Moreover, 5 % of children experience transient coronary artery dilation and 1 % still go on to develop giant aneurysms [8]. Genetic polymorphisms encoding cytokines, chemokines, and enzymes involved in signal transduction are thought to explain differences in susceptibility to KD itself, as well as the response to IVIG treatment [11].
IVIG appears to reduce immune activation and inflammation through several proposed mechanisms (Table 1). IVIG inhibits the activation of monocytes, macrophages, and coronary arterial endothelial cells more than T lymphocytes in vitro. Interestingly, Kawasaki himself was the first to describe peripheral blood eosinophilia in his initial cohort of 50 patients with KD [12].
Finally, Treg and FOXP3 mRNA gene expression both increased after IVIG treatment [10]. These changes were not associated with clinical endpoints such as coronary artery aneurysm involvement, but they suggest that an inflammatory environment contributes to the Treg dysregulation which IVIG therapy targets, although no direct linkage has been established to date [10]. IVIG also suppresses an array of immune activation genes in monocytes, including those activating FcɣRs and genes involved in TGF-β signaling [5]. Genomic studies have identified several genes encoding FcɣRI and FcɣRIII on monocytes were reduced after IVIG [11]. Conversely, a reduced therapeutic response to IVIG is a known risk factor for coronary aneurysm development [11].
Immune Thrombocytopenia
Primary ITP is characterized by thrombocytopenia typically occurring several weeks after a viral illness. Acute pediatric ITP is considered one of the most common acquired bleeding disorders in children and is generally self-limited, with spontaneous resolution occurring within 6–12 months in over 80 % of cases irrespective of intervention [13]. While most cases in children are accompanied by mild mucosal bleeding, the risk of severe intracranial hemorrhage (ICH) or gastrointestinal hemorrhage fuels the impetus for treatment given its high mortality rate [14]. The 2011 American Society of Hematology Clinical Treatment Guideline lists IVIG as a first-line treatment option favored over corticosteroids in settings when a rapid increase in platelet count is desired. Dosing for this and other indications reviewed are listed (Table 2).
Immune Mechanisms of ITP
Acute ITP represents the majority of pediatric ITP, while most adult cases are chronic. The mechanisms underlying childhood ITP appear distinct from adult ITP, and some authors theorize that childhood ITP results from transient immune complex formation, whereas adult ITP is a manifestation of an underlying autoimmune disorder often requiring corticosteroids [15]. Two main mechanisms underlie the pathogenesis of ITP: (1) increased platelet destruction and (2) decreased platelet production [16].
Increased destruction occurs predominantly via autoantibodies against platelet antigens such as glycoprotein IIb/IIIa and glycoprotein Ib/IX that opsonize the platelets leading to phagocytosis via the reticuloendothelial system [16, 17]. Molecular mimicry contributes to epitope spreading leading to chronic ITP. T cell mechanisms underlying defective immune tolerance have been proposed, given that platelet-associated autoantibodies are undetectable in 40–50 % of ITP cases [16]. Decreased platelet production is also attributable to antiplatelet antibodies that suppress megakaryocytopoiesis through the direct inhibition of the thrombopoietin (TPO) receptor [18]. This observation is supported by studies showing that lower than expected TPO levels were found in ITP patients [19].
Effects of IVIG Treatment on ITP
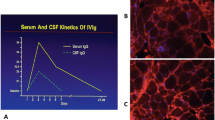
The application of IVIG in ITP dates back to 1981 when an increase in platelets was observed after IVIG in a patient with Wiskott-Aldrich syndrome [20]. Yet, suspicion of an immune mechanism underlying ITP dates back earlier, raising interest in ITP as a model for studying the effects of IVIG on other autoimmune-mediated disorders. Today, ITP is the most common non-primary immunodeficiency-based indication for IVIG in children. The primary mechanism of IVIG occurs through the neutralization and clearance of pathogenic antibodies, modulating or blocking the Fc receptors on platelets and macrophages, and preventing the formation of immune complexes, opsonization, and phagocytosis [21]. IVIG also competitively saturates the neonatal Fc receptor (FcRn) and increases the catabolism and clearance of antibodies, including pathogenic ITP autoantibodies [21]. Finally, IVIG provides pathogen-blocking activity (passive immunity) given that infection is a proposed trigger. These and other immune modulatory effects are reviewed (Table 1 and Fig. 1).
Adverse Effects of IVIG on ITP
While IVIG is generally considered safe, common and serious adverse effects include aseptic meningitis, anaphylaxis, and thromboembolism (Table 3). Generally, thromboembolic complications are rare in pediatric populations, but several mechanisms specific to ITP have been identified to include platelet activation, arterial vasospasm, increased fibrinogen levels, increased plasma viscosity, increased factor XI concentration, activation of serum complement, and increase in arterial vascular tone (Table 3) [22]. A case of cerebral sinus thrombosis in a child with ITP with a post-IVIG headache highlights that thromboembolism remains a serious risk [23]. Another less severe adverse effect of IVIG is neutropenia, which tends to be transient [24].
Pediatric Guillain-Barré Syndrome
GBS is an acute acquired inflammatory demyelinating polyneuropathy that occurs in both adults and children and is the most common cause of acquired neuropathy in the post-poliomyelitis era. It is characterized by symmetric, ascending flaccid paralysis, weakness, or diminished deep tendon reflexes. Although generally self-limited, severe rapidly progressive weakness may require ventilator support. It has been associated with infectious triggers including Campylobacter jejuni. In general, the pediatric form is thought to be clinically milder with greater likelihood of recovery, although persisting muscle weaknesses was seen in 20–25 % of cases in both the pre-IVIG and post-IVIG eras but with milder deficits in the post-IVIG era [25, 26]. Moreover, age younger than 9 years and rapid progression of symptoms within 10 days were predictors of long-term sequelae [26].
Pathogenesis of GBS
Studies on the immunologic pathogenesis of GBS are predominantly based on animal model or in vitro studies, as GBS resembles an animal-based disease entity called experimental autoimmune neuritis (EAN). Macrophages play a key role in phagocytosis and release of pro-inflammatory cytokines which propagate axonal damage [27]. Both humoral and cell-mediated immunity contribute to the pathogenesis of GBS. Antibodies to antigens found on the myelin sheath or peripheral nerve correlate with disease severity [28, 29]. However, a major limitation in this finding was that elevated titers of such antibodies were also observed in healthy controls [29, 30]. It was subsequently discovered that immunoglobulins and particularly IgG bind nonspecifically to myelin proteins found in the central and peripheral nervous systems [28]. Other antibodies target gangliosides and neural glycolipids. The role of cell-mediated immunity also contributes to the pathogenesis of GBS, and a predominance of CD4+ T helper cells compared to CD8+ T cells and T regulatory cells is observed [28]. CD4+ T cells play a pivotal role in the activation of macrophages, B cell proliferation, production of plasma cells, and the activation of cytokines with myelinotoxic effects via the Th1 inflammatory pathway [28]. Inflammation from immune activation is thought to disturb nerve impulse propagation through myelinotoxic effects [30].
The Therapeutic Role of IVIG
Along with plasmapheresis, corticosteroids, and supportive therapy, IVIG is one of the major treatments for GBS. In adults, IVIG and plasmapheresis have similar efficacy in hastening recovery from GBS [25]. Pediatric studies of IVIG (2 g/kg divided over 2 or 5 days) are limited but suggest benefit [25]. One multicenter randomized study from Western Europe found that early treatment with IVIG was associated with earlier motor recovery [31]. Other studies show that IVIG was no better than supportive care, although the time from symptom onset to maximum symptom severity was shorter in patients who received IVIG within 10 days than patients who did not receive IVIG [32]. Both efficacy and non-efficacy have been documented in children with GBS, and most of these studies are limited by small study design.
The most recent Cochrane Review published in 2012 describes the beneficial effect of IVIG in children over supportive care only, although the studies reviewed contained limitations in study design [25]. Moreover, the pediatric studies also showed a trend toward more clinical improvement with high-dose compared with low-dose IVIG given over 2 days [25].
IVIG inhibits both humoral and cell-mediated mechanisms activated in GBS (Table 1). IVIG also appears to target bacterial triggers and counter superantigen-induced T cell activation via anti-toxin antibodies. In addition to its immunomodulatory effects, IVIG has been described to promote remyelination in animal models. In an EAN study, pooled immunoglobulin from donor mice promoted remyelination in studies in multiple sclerosis and in EAN [33, 34]. The mechanism is unknown but proposed to occur through improving the opsonization of myelin and axons, limiting the secondary inflammatory cell infiltration and injury, and removing myelin-associated debris [35].
Neonatal and Preterm Infant Sepsis
For nearly two decades, attention has focused on the use of IVIG as a potential strategy to both prevent and reduce the morbidity and mortality associated with neonatal sepsis, particularly in vulnerable preterm infants [36]. Neonatal bacterial infections can be particularly devastating in this vulnerable population, and antibodies play a particularly central role in combating infections caused by encapsulated bacteria and promoting FcɣR-mediated phagocytosis and the deposition of the opsonin complement C3b. In healthy newborns, IgG originates via placental transfer predominantly in the third trimester, with the highest IgG delivered typically at 38–40 weeks gestation [36]. Preterm delivery alters this, as such infants have profoundly low levels of IgG and do not begin generating their own immunoglobulin until 6 months of age. Hence, the application of IVIG to prevent neonatal sepsis would appear particularly attractive given it could directly supply the antibodies and additional immunomodulatory benefits [36, 37].
Use of IVIG Prophylaxis in Preterm Infants
Theoretically, replacement IgG in preterm infants appeared promising. Yet, despite extensive studies, no published guidelines clearly recommend its use [38]. Data on the use of prophylactic IVIG appear mixed, with the majority of studies showing minimal benefit and questionable clinical utility. A 2013 Cochrane Review of 19 studies performed across 10 countries included preterm and/or low-birth weight infants and found IVIG was associated with a 3–4 % reduction in serious nosocomial infection and shorter duration of hospitalization (mean 2.1 days) but no benefit in infant mortality from infection [39]. Authors argue that this small but statistically significant reduction in infection should be weighed against the costs of broad recommendation across the large preterm infant population [39]. In contrast, animal studies have suggested potential detriment, showing that excessive IgG may impair microbial clearance [40, 41].
IVIG for Treatment of Neonatal Sepsis
IVIG as a therapeutic adjuvant in neonatal sepsis has been explored with immunologic mechanisms reviewed (Table 1). Providing passive immunity to sick neonates underlies the application of IVIG as a treatment modality for culture-proven or suspected neonatal sepsis in addition to enhancing opsonization, phagocytosis, and complement, promoting antibody-dependent cytotoxicity (ADCC), modulating T cell and macrophage activity via cytokines, stimulating B cell effector functions, and improving neutrophil-mediated killing [36, 37]. Studies are limited by data derived from small and heterogeneous studies. One multicenter trial of term neonates with symptoms of bacterial sepsis showed that a single dose of IVIG in combination with antibiotics significantly delayed death and suggested a role for IVIG in enhancing survival [42]. Still, a recent randomized trial of 3,493 infants with suspected sepsis evaluated the role of IVIG (500 mg/kg/dose) as adjuvant therapy in infants already receiving IV antibiotics and found no significant difference in death or neurodevelopmental outcomes [43].
Unique Nature of Neonatal Immunity
Multiple explanations address the limited efficacy of IVIG for the prevention or treatment of neonatal sepsis [44]. Some are based in limitations in study design such as varied inclusion criteria, heterogeneity in dosing, variation in pathogens, the low levels of antibodies to neonate-specific pathogens in IVIG, and use of non-enriched IgM products. The limited application of IVIG in sepsis may be attributable to the unique nature of the neonatal immune system. In particular, one of the theoretical benefits of IVIG is improving opsonization and phagocytosis. However, preterm infants exhibit decreased PMN opsonic capacity, phagocytosis, and respiratory burst compared to term neonates and adults [45]. Hence, immunoglobulin supplementation in a complement-reduced neonatal environment derived from adult serum may be poorly matched for vulnerable neonates [46].
Pediatric Human Immunodeficiency Virus (HIV-1)
Pediatric HIV-1/AIDS was recognized in the 1980s as a clinical syndrome resembling agammaglobulinemia characterized by recurrent bacterial infections and sepsis. HIV-1 is now estimated to affect 3.3 million children worldwide, with primary transmission occurring vertically from infected mothers [47]. Infants with perinatally acquired infection demonstrate a shorter incubation period and a more rapid clinical course compared to adults. The normal physiologic lymphocytosis of infancy offsets the CD4+ T cell lymphopenia more typically observed in adult HIV-1 [48].
Immunology of Pediatric HIV
Although the main target of HIV is the CD4 T cell, HIV-1 exerts a broad range of immunologic effects. HIV itself has envelope glycoproteins that have been shown to inhibit lymphoproliferative responses. For example, the envelope protein gp120 serves to inhibit phytohemagluttin responses [49]. B cell dysfunction is reflected in the hypergammaglobulinemia and diminished functional antibody response. Residues on the carboxyl end of the HIV-1 envelope glycoprotein gp41 have been implicated in this dysfunctional B cell stimulatory activity which may deplete the remaining antigen-responsive precursor B cell pool and suppress clonal expansion [50]. Moreover, uncontrolled HIV-1 viremia inhibits adequate IL-2 in response to CD4 T cell stimulation [51]. Even after restoration of immune function with highly active anti-retroviral therapy (HAART), B cell memory was not restored after vaccination or to naturally occurring viruses [52], signaling that the fundamental ability of B cells to produce antibodies to previously exposed antigens remained impaired. The relative poor response was attributable to the deficiency of IgM memory B cells, which also explains the increased risk to encapsulated organisms [52]. Other aspects of compromised B cell function are marked by the presence of increased circulating immune complexes (associated with the hypergammaglobulinemia) as well as occasional observation of hypogammaglobulinemia [53]. Moreover, in pediatric HIV-1, infants who are infected prior to delivery or perinatally receive incomplete passive transplacental transfer of maternal IgG, a further disadvantage [54].
Rationale for IVIG
IVIG exerts a broad range of immunologic effects (Table 1) and has been studied as both prophylaxis and treatment for pediatric HIV-1 in the pre- and post-HAART eras. Prior to the era of routine use of HAART, the rationale for use of IVIG was based on the clinical similarity of infections in children with HIV and those with congenital hypogammaglobulinemia, and IVIG was found to decrease serious bacterial infections. HAART has since substantially reduced morbidity and increased the life expectancy of children with HIV-1 [55]. Prior to the routine use of HAART, the National Institute of Child Health and Human Development study was the most rigorous randomized, placebo-controlled study of IVIG in a multicenter population of 372 children receiving monthly IVIG and demonstrated decreased serious and minor bacterial infections and days of hospitalization; however, IVIG had no effect on mortality [56]. Subsequently, Spector et al. conducted another randomized trial in children receiving the anti-retroviral zidovudine and found that IVIG decreased risk of serious bacterial infections only in those subjects not receiving TMP-SMX prophylaxis [57]. IVIG did not slow the decline in CD4+ T cell counts or effect survival [57]. While pediatric HIV-1 maintains its historic place as one of the few pediatric-specific FDA-approved indications for IVIG, its practical relevance in the post-HAART era has waned.
Intractable Childhood Epilepsy (ICE)
Despite advances in treating epileptic disorders in childhood, approximately 30 % of children with epilepsy do not respond to conventional therapies, and alternative treatments are needed. An immunologic mechanism was hypothesized to play a role in epilepsy studies in animal models dating back to the 1970s, contradicting the notion that the brain is an immunologically privileged organ. In the 1980s, autoimmune mechanisms were suspected after observing that IVIG effectively treated some forms of ICE [58]. Since then, clinical and experimental data support the role of immune mechanisms in the pathogenesis of childhood epilepsy, and IVIG has been used to treat West syndrome, Lennox Gastaut syndrome, early myoclonic encephalopathy, and Rasmussen syndrome with promising results [59]. Immunologic abnormalities appear disproportionately in epileptic patients and include decreased IgA, IgG2, increased total IgG and IgM, anti-idiotype antibodies, increased prevalence of certain human leukocyte antigen (HLA) types, alterations in cytokine profiles, and autoantibodies to neuronal signaling pathways [60, 61]. The favorable response to immunomodulating treatments like corticosteroids and corticotrophin (ACTH) to treat seizure disorders (West syndrome) also supports an immunologic role and the potential value of IVIG as an adjunctive treatment option for ICE [61].
Trials of IVIG for ICE
A multicenter review of 373 children suffering from ICE across 29 studies published in the 1970s–1990s reports similar responsiveness for refractory cases ranging from 30 to 50 %, although studies were heterogeneous with controls lacking [62]. A more recent, retrospective, multicenter study of 64 patients treated with IVIG for epileptic encephalopathy or refractory epilepsy showed an overall 30 % response, and improvement was seen in 75 % of idiopathic West syndrome [61]. Although retrospective, the authors claim their study was the largest consecutive study of IVIG therapy to children with epilepsy and conclude that it may be beneficial for some forms of ICE, although no common dominator among responders was identified [61]. These data are consistent with other studies, although response rates remain variable [63].
IVIG Therapeutic Mechanisms
IVIG is thought to exert anti-epileptic effects through targeting upregulated cytokine pathways and antibodies thought to contribute to epilepsy (Table 1) [64]. Although the mechanism is not fully elucidated, studies suggest IVIG acts centrally to limit the progression of electrical seizure activity into clinical seizures [63]. In Rasmussen syndrome, characterized by focal seizures, progressive neurologic and intellectual deterioration, chronic encephalitis, and hemispheric atrophy, the identification of serum antibodies to the glutamate receptor GluR3, anti-nuclear antibodies, increased total IgG, and the presence of intrathecal oligoclonal Ig synthesis suggests an autoimmune mechanism justifying the application for IVIG in difficult-to-treat cases [59, 63].
Applications in Miscellaneous Pediatric Diseases
IVIG has been applied to other pediatric diseases of interest with varying degrees of efficacy observed in light of other available therapeutic modalities. These disease entities particularly relevant in pediatrics but of varying clinical utility are reviewed here and include pediatric asthma, atopic dermatitis, cystic fibrosis, PANDAS, autism, and transplantation.
In pediatric asthma, IVIG has been utilized to target the chronic airway inflammation and as a potential steroid-sparing therapeutic in small numbers of steroid-dependent asthmatic children in the 1990s. While initial open label and uncontrolled studies in populations of children receiving high-dose IVIG appeared promising [65, 66], subsequent randomized, double-blind, placebo-controlled studies did not show sufficient steroid-sparing effects [67, 68]. No significant subsequent studies have been performed since. Overall, asthma remains a heterogeneous disease driven and perpetuated by multiple triggers. While some of these small studies suggest IVIG may be helpful in very select populations, the overall consensus is that insufficient data on efficacy in addition to concerns about side effects do not warrant routine or broad usage in the treatment of pediatric asthma.
IVIG has also been used in the treatment of atopic dermatitis (AD), initially noted anecdotally in patients with KD or ITP with dermatitis that improved after IVIG [69]. Other studies in patients with elevated IgE did not demonstrate benefit to AD symptoms [70]. Other studies describe increased Th2 cytokines including IL-4, IL-5, IL-10, and IL-13 in the acute phase and Th1 cytokines (IFN-γ) in the chronic phase of severe AD [71]. In a controlled study of 30 children treated with IVIG (2 g/kg/month) and 10 treated with placebo [72], patients demonstrated baseline increased levels of ICAM-1 and endothelial leukocyte adhesion molecule (ELAM-1). After 3 months of IVIG, levels of ICAM-1, ELAM-1, and IL-5 were reduced and remained reduced 3 months after high-dose IVIG therapy. Efficacy was also demonstrated at 3 months based on SCORAD and immunologic markers but not at 6 months. Data from smaller studies [70, 73] suggests that in select patients with severe, steroid-resistant AD, IVIG may be efficacious. No randomized, controlled trials have been performed, and caution with respect to the infusion frequency, side effects, and cost are additional considerations in the application of IVIG in pediatric atopic dermatitis.
IVIG has also been applied to select cases of children with cystic fibrosis (CF) with secondary hypogammaglobulinemia, but there remains no clear additional benefit or reduction in morbidity based on studies performed several decades ago [74]. One study retrospectively measured the serum immunoglobulins of 419 patients with CF and demonstrated that in contrast to older CF children and adolescents, nearly one quarter of CF patients less than 10 years old had hypogammaglobulinemia [75]. This differential observation remained unexplained in studies of T and B lymphocyte function in vitro or in studies of IgG metabolism in vivo. The authors did find that patients with hypogammaglobulinemia demonstrated less severe lung disease than CF children with normal or elevated IgG, a finding that was replicated in a population of 70 children [76]. The authors speculated that the progression of lung disease may be due in part to immune hyperactivation in CF [75]. No significant further study has been performed on CF and IVIG, so its applications remain limited.
PANDAS is a controversial disease entity that has historically been treated with steroids, IVIG, or plasma exchange [77]. The disease is believed to be mediated by antibodies to neuronal tissue after group A β-hemolytic streptococcal infection and associated with the presentation or exacerbation of neuropsychiatric symptoms including tics and obsessive-compulsive disorder. Recent retrospective analysis of a small case series demonstrated that despite heterogeneous duration of illness and recurrence, all patients benefited from IVIG administration, even when the neuropsychiatric symptoms had been present for several years prior to treatment [77]. IVIG is believed mechanistically to inactivate cross-reactive antibodies even after a single course. The study was limited in its retrospective nature, and patients were treated with multiple medications, including antibiotics and behavioral therapies. Controversy surrounds both the diagnosis of PANDAS and reliable ways to measure treatment response to IVIG, as symptoms may self-resolve with time irrespective of therapy administered [78, 79]. Moreover, the lack of observed association between therapeutic response and the rate of antibody removal and how antibody-mediated processes in the periphery can induce neuropsychiatric symptoms remains difficult to answer [78]. Small studies from the late 1990s [78, 79] suggested potential promise for highly select patients; however, no further prospective, controlled studies have since been performed to clarify the therapeutic benefit of IVIG.
Autism spectrum disorders (ASD) refer to neurodevelopmental diagnoses characterized by impaired social interactions, communication, and restricted interests and activities [80]. Multiple environmental, genetic, and immunologic factors have been theorized to contribute to the pathophysiology of ASD. Speculation on the presence of autoantibodies to neural antigens and immunologic alterations in lymphocyte subsets, serum immunoglobulin subclasses, and cytokine production has also been proposed [81]. Reportedly, the strongest evidence lay in immunogenetic studies showing increased genetic abnormalities in HLA genes such as those encoding complement C4b and HLA-DR found in children with ASD [81]. In small studies of ASD children, a low serum IgA and selective IgA deficiency was reported [82], while NK cells and CD4 T cells were also decreased compared to non-ASD children [83]. Other research debunks an immunologic basis for ASD and attributes associations to epiphenomena [83]. The authors identified that autoimmune factors were associated when improvement was observed after IVIG; however, this study lacked objective behavioral assessments [84]. A subsequent pilot study of seven autistic children by DelGuidice-Asch et al. suggested that IVIG did not improve autism symptom scores [85]. No randomized, placebo-controlled studies of IVIG in ASD have been performed to date, and its application remains largely speculative.
Finally, bone marrow or hematopoietic stem cell transplantation (BMT/HSCT) and solid organ transplantation are additional contexts in which IVIG offers immunomodulatory functions and passive immunity. In adults, bone marrow transplantation is an FDA-approved indication for IVIG and provides passive antibodies to prevent infection, reduces the occurrence of graft-versus-host disease (GVHD), and interrupts acute antibody-mediated rejection (AMR) [59]. IVIG (1–2 g/kg) treats patients with established AMR and preemptively treats patients with positive cross-match.
In the pre-ganciclovir era, randomized trials showed that IVIG and hyperimmune anti-cytomegalovirus (CMV) IVIG reduced the incidence of CMV infection in BMT patients. However, a systemic review of both adult and pediatric transplant patients treated with IVIG showed no difference in mortality, infection-associated outcomes, or acute rejection [86]. While decreased interstitial pneumonitis was documented, this benefit was outweighed by the deleterious increased risk of hepatic veno-occlusive disease, associated with IVIG. Such conclusions were derived from studies performed in the 1980s–1990s, and newer pre-transplant conditioning techniques have since emerged, which raise question to the applicability of older studies.
For acute GVHD, earlier studies and animal models showed that IgG and F(ab′)2 fragment protect against acute but not chronic GVHD [59]. In a multicenter study of adult and pediatric patients across 10 centers, weekly IVIG (500 mg/kg) was significantly associated with less acute GVHD given over 16 weeks post-transplant (44 versus 58 %) [87].
In solid organ transplantation, a small prospective study of pediatric liver transplant patients showed that IVIG in combination with low-dose immunosuppression was associated with a lower incidence of CMV disease, making IVIG an attractive alternative to the antiviral ganciclovir [88]. However, this study did not properly account for late-onset CMV infection. In pediatric renal transplant patients, BK virus infection and BK virus nephropathy are additional complications that can cause graft rejection. IVIG containing these anti-polyomavirus antibodies confer passive humoral immunity and immunomodulatory effects augmenting viral clearance [89].
Role of Subcutaneous Immunoglobulin (SCIg)
For the last few decades, Ig therapy in the form of SCIg has been increasingly utilized and favored in the treatment of primary immunodeficiency for its improved side effect profile, convenience with home infusions, and improved steady state serum IgG levels [87]. Recent research into applications of SCIg in non-primary immunodeficiencies has focused primarily on CIPD and inflammatory myopathies (polymyositis, dermatomyositis) in adults [90–92]. Preliminary studies in small numbers of patients in primarily European studies suggest improved tolerability, patient satisfaction, and cost in the disease stabilization period of these disorders [90, 93–95], although long-term efficacy and randomized controlled studies are unavailable, and these studies were performed in patients who received SCIg after IVIG. Moreover, there are speculative theoretical advantages of achieving peak IgG levels via IVIG in the acute phase of diseases like KD and ITP, and IVIG has been proposed to primarily target the humoral immune component whereas SCIg is postulated to better target the cellular component of the immune modulatory response [91].
Conclusion
This review highlights the potential of IVIG therapy in major pediatric diseases with a unique focus on immunologic mechanisms and the role of IVIG in non-primary immunodeficiency. The diverse applications of IVIG extend to inflammatory diseases such as Kawasaki disease, ITP, and Guillain-Barré syndrome, diseases characterized by impaired immunity such as in neonatal sepsis, HIV-1, and those with still incompletely defined mechanisms such as intractable childhood epilepsy. Additional applications in pediatric asthma, atopic dermatitis, cystic fibrosis, PANDAS, autism, and transplantation represent diverse conditions in which IVIG has been applied with varying clinical results. The studies describing mechanism of action are limited in the extrapolated nature of the data from in vitro or animal-based studies but nevertheless offer insight into the disease and the broad-reaching impact of IVIG itself. We currently embark upon an exciting era in immunology. Our review highlights the diverse functions of IVIG in pediatric disease across the spectrum from deficiency to autoimmunity. Uncovering the still undefined immunopathology underlying many pediatric diseases remains a challenge to be embraced.
References
Bruton OC (1952) Agammaglobulinemia. Pediatrics 9(6):722–728
Behring EAK, Ueber S (1890) das zustandekommen der diphtherie-immunitat und der tetanus-immunitat bei thieren. Dtsch Med Wochenschr 16:1113–1114
Gelfand EW (2012) Intravenous immune globulin in autoimmune and inflammatory diseases. N Engl J Med 367(21):2015–2025
Stangel M, Pul R (2006) Basic principles of intravenous immunoglobulin (IVIg) treatment. J Neurol 253(Suppl 5):V18–V24
Eleftheriou D et al (2014) Management of Kawasaki disease. Arch Dis Childhood 99(1):74–83
Galeotti C et al (2010) Kawasaki disease: aetiopathogenesis and therapeutic utility of intravenous immunoglobulin. Autoimmun Rev 9(6):441–448
Kaneko K et al (2012) Intravenous immunoglobulin counteracts oxidative stress in Kawasaki disease. Pediatr Cardiol 33(7):1086–1088
Kobayashi T et al (2006) Prediction of intravenous immunoglobulin unresponsiveness in patients with Kawasaki disease. Circulation 113(22):2606–2612
Abe J et al (1992) Selective expansion of T cells expressing T-cell receptor variable regions V beta 2 and V beta 8 in Kawasaki disease. Proc Natl Acad Sci U S A 89(9):4066–4070
Olivito B et al (2010) Defective FOXP3 expression in patients with acute Kawasaki disease and restoration by intravenous immunoglobulin therapy. Clin Exp Rheumatol 28(1 Suppl 57):93–97
Abe J et al (2005) Gene expression profiling of the effect of high-dose intravenous Ig in patients with Kawasaki disease. J Immunol 174(9):5837–5845
Kuo HC et al (2007) The relationship of eosinophilia to intravenous immunoglobulin treatment failure in Kawasaki disease. Pediatr Allergy Immunol: Off Publ Eur Soc Pediatr Allergy Immunol 18(4):354–359
Gadner H (2001) Management of immune thrombocytopenic purpura in children. Rev Clin Exp Hematol 5(3):201–221, discussion 311-2
Butros LJ, Bussel JB (2003) Intracranial hemorrhage in immune thrombocytopenic purpura: a retrospective analysis. J Pediatr Hematol Oncol 25(8):660–664
Holt D et al (2003) Response to intravenous immunoglobulin predicts splenectomy response in children with immune thrombocytopenic purpura. Pediatrics 111(1):87–90
Nugent D et al (2009) Pathogenesis of chronic immune thrombocytopenia: increased platelet destruction and/or decreased platelet production. Br J Haematol 146(6):585–596
Taub JW et al (1995) Characterization of autoantibodies against the platelet glycoprotein antigens IIb/IIIa in childhood idiopathic thrombocytopenia purpura. Am J Hematol 48(2):104–107
McMillan R et al (2004) Suppression of in vitro megakaryocyte production by antiplatelet autoantibodies from adult patients with chronic ITP. Blood 103(4):1364–1369
Bussel JB et al (2006) AMG 531, a thrombopoiesis-stimulating protein, for chronic ITP. N Engl J Med 355(16):1672–1681
Imbach P et al (1981) High-dose intravenous gammaglobulin for idiopathic thrombocytopenic purpura in childhood. Lancet 1(8232):1228–1231
Hansen RJ, Balthasar JP (2004) Mechanisms of IVIG action in immune thrombocytopenic purpura. Clin Lab 50(3-4):133–140
Katz U, Shoenfeld Y (2005) Review: intravenous immunoglobulin therapy and thromboembolic complications. Lupus 14(10):802–808
Al-Riyami AZ et al (2011) Cerebral sinus thrombosis following IV immunoglobulin therapy of immune thrombocytopenia purpura. Pediatr Blood Cancer 57(1):157–159
Niebanck AE, Kwiatkowski JL, Raffini LJ (2005) Neutropenia following IVIG therapy in pediatric patients with immune-mediated thrombocytopenia. J Pediatr Hematol Oncol 27(3):145–147
Hughes RA, Swan AV, van Doorn PA (2012) Intravenous immunoglobulin for Guillain-Barre syndrome. Cochrane Database Syst Rev 7, CD002063
Vajsar J, Fehlings D, Stephens D (2003) Long-term outcome in children with Guillain-Barre syndrome. J Pediatr 142(3):305–309
Said G, Hontebeyrie-Joskowicz M (1992) Nerve lesions induced by macrophage activation. Res Immunol 143(6):589–599
Hartung HP et al (1995) Immunopathogenesis and treatment of the Guillain-Barre syndrome—part I. Muscle Nerve 18(2):137–153
Cruz M et al (1988) Occurrence and isotype of antibodies against peripheral nerve myelin in serum from patients with peripheral neuropathy and healthy controls. J Neurol Neurosurg Psychiatry 51(6):820–825
Hartung HP et al (1995) Immunopathogenesis and treatment of the Guillain-Barre syndrome—part II. Muscle Nerve 18(2):154–164
Koul R et al (2003) Ten-year prospective study (clinical spectrum) of childhood Guillain-Barre syndrome in the Arabian peninsula: comparison of outcome in patients in the pre- and post-intravenous immunoglobulin eras. J Child Neurol 18(11):767–771
Tasdemir HA et al (2006) Intravenous immunoglobulin for Guillain-Barre syndrome: how effective? J Child Neurol 21(11):972–974
Gabriel CM et al (1997) Human immunoglobulin ameliorates rat experimental autoimmune neuritis. Brain: J Neurol 120(Pt 9):1533–1540
van Engelen BG et al (1994) Promotion of remyelination by polyclonal immunoglobulin in Theiler's virus-induced demyelination and in multiple sclerosis. J Neurol Neurosurg Psychiatry 57(Suppl):65–68
Kuhlmann T, Bruck W (1999) Immunoglobulins induce increased myelin debris clearance by mouse macrophages. Neurosci Lett 275(3):191–194
Jenson HB, Pollock BH (1998) The role of intravenous immunoglobulin for the prevention and treatment of neonatal sepsis. Semin Perinatol 22(1):50–63
Baley JE (1988) Neonatal sepsis: the potential for immunotherapy. Clin Perinatol 15(4):755–771
Soll RF (2013) Calling time on intravenous immunoglobulin for preterm infants? Cochrane Database System Rev 7, ED000062
Ohlsson A, Lacy JB (2013) Intravenous immunoglobulin for preventing infection in preterm and/or low birth weight infants. Cochrane Database Syst Rev 7, CD000361
Cross AS et al (1984) Intravenous immune globulin: a cautionary note. Lancet 1(8382):912
Sandberg K et al (2000) Preterm infants with low immunoglobulin G levels have increased risk of neonatal sepsis but do not benefit from prophylactic immunoglobulin G. J Pediatr 137(5):623–628
Fischer GW (1994) Use of intravenous immune globulin in newborn infants. Clin Exp Immunol 97(Suppl 1):73–77
Brocklehurst P et al (2011) Treatment of neonatal sepsis with intravenous immune globulin. N Engl J Med 365(13):1201–1211
Wynn JL, Seed PC, Cotten CM (2010) Does IVIg administration yield improved immune function in very premature neonates? J Perinatol 30(10):635–642
Kallman J et al (1998) Impaired phagocytosis and opsonisation towards group B streptococci in preterm neonates. Archives of disease in childhood. Fetal Neonatal Ed 78(1):F46–F50
Lassiter HA et al (1990) Complement C3 deposition onto bacteria by neonatal serum is not enhanced after the infusion of intravenous immunoglobulin. J Perinatol: Off J California Perinatal Assoc 10(1):27–31
UNAIDS Report on the Global AIDS Epidemic, 2012 (2012 04 June 2014]; Available from: http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2012/gr2012/20121120_UNAIDS_Global_Report_2012_with_annexes_en.pdf
Mofenson LM, Moye J Jr (1993) Intravenous immune globulin for the prevention of infections in children with symptomatic human immunodeficiency virus infection. Pediatr Res 33(1 Suppl):S80–S87, discussion S87-9
Mann DL et al (1987) HTLV-III large envelope protein (gp120) suppresses PHA-induced lymphocyte blastogenesis. J Immunol 138(8):2640–2644
Pahwa S (1990) Immune defects in pediatric AIDS, their pathogenesis, and role of immunotherapy. Crit Care Med 18(2 Suppl):S138–S143
Moir S et al (2003) Perturbations in B cell responsiveness to CD4+ T cell help in HIV-infected individuals. Proc Natl Acad Sci U S A 100(10):6057–6062
Bekker V et al (2006) Persistent humoral immune defect in highly active antiretroviral therapy-treated children with HIV-1 infection: loss of specific antibodies against attenuated vaccine strains and natural viral infection. Pediatrics 118(2):e315–e322
Pahwa S (1989) Intravenous immune globulin in patients with acquired immune deficiency syndrome. J Allergy Clin Immunol 84(4 Pt 2):625–630, discussion 630-1
Classification system for human immunodeficiency virus (HIV) infection in children under 13 years of age. MMWR. Morbidity and mortality weekly report, 1987. 36(15): p. 225-30, 235-6
Deener A et al (2008) Intravenous gammaglobulin treatment in HIV-1 infection. Immunol Allergy Clin North Am 28(4):851–859, x
Intravenous immune globulin for the prevention of bacterial infections in children with symptomatic human immunodeficiency virus infection. The National Institute of Child Health and Human Developments Intravenous Immunoglobulin Study Group. N Engl J Med, 1991. 325(2): p. 73-80
Spector SA et al (1994) A controlled trial of intravenous immune globulin for the prevention of serious bacterial infections in children receiving zidovudine for advanced human immunodeficiency virus infection. Pediatric AIDS Clinical Trials Group. N Engl J Med 331(18):1181–1187
van Rijckevorsel K (1999) Immunological mechanisms in the aetiology of epilepsy: implications for treatment. Bio Drugs: Clin Immunother Biopharmaceuticals Gene Ther 12(2):115–127
Orange JS et al (2006) Use of intravenous immunoglobulin in human disease: a review of evidence by members of the Primary Immunodeficiency Committee of the American Academy of Allergy, Asthma and Immunology. J Allergy Clin Immunol 117(4 Suppl):S525–S553
Bien CG, Scheffer IE (2011) Autoantibodies and epilepsy. Epilepsia 52(Suppl 3):18–22
Geva-Dayan K et al (2012) Immunoglobulin treatment for severe childhood epilepsy. Pediatric Neurol 46(6):375–381
Duse M et al (1996) Intravenous immune globulin in the treatment of intractable childhood epilepsy. Clin Exp Immunol 104(Suppl 1):71–76
Billiau AD et al (2007) Intravenous immunoglobulins in refractory childhood-onset epilepsy: effects on seizure frequency, EEG activity, and cerebrospinal fluid cytokine profile. Epilepsia 48(9):1739–1749
Mikati MA et al (2010) Intravenous immunoglobulin therapy in intractable childhood epilepsy: open-label study and review of the literature. Epilepsy Behav: E&B 17(1):90–94
Jakobsson T et al (1994) Slight steroid-sparing effect of intravenous immunoglobulin in children and adolescents with moderately severe bronchial asthma. Allergy 49(6):413–420
Mazer BD, Gelfand EW (1991) An open-label study of high-dose intravenous immunoglobulin in severe childhood asthma. J Allergy Clin Immunol 87(5):976–983
Kishiyama JL et al (1999) A multicenter, randomized, double-blind, placebo-controlled trial of high-dose intravenous immunoglobulin for oral corticosteroid-dependent asthma. Clin Immunol 91(2):126–133
Niggemann B et al (1998) Prospective, double-blind, placebo-controlled, multicentre study on the effect of high-dose, intravenous immunoglobulin in children and adolescents with severe bronchial asthma. Clin Exp Allergy 28(2):205–210
Jolles S, Hughes J, Rustin M (2000) The treatment of atopic dermatitis with adjunctive high-dose intravenous immunoglobulin: a report of three patients and review of the literature. Br J Dermatol 142(3):551–554
Wakim M et al (1998) High dose intravenous immunoglobulin in atopic dermatitis and hyper-IgE syndrome. Ann Allergy Asthma Immunol 81(2):153–158
Grewe M et al (1998) A role for Th1 and Th2 cells in the immunopathogenesis of atopic dermatitis. Immunol Today 19(8):359–361
Jee SJ et al (2011) Long-term efficacy of intravenous immunoglobulin therapy for moderate to severe childhood atopic dermatitis. Allergy Asthma Immunol Res 3(2):89–95
Jolles S et al (2003) Adjunctive high-dose intravenous immunoglobulin treatment for resistant atopic dermatitis: efficacy and effects on intracellular cytokine levels and CD4 counts. Acta Derm Venereol 83(6):433–437
Bentur L et al (1990) Advanced lung disease in a patient with cystic fibrosis and hypogammaglobulinemia: response to intravenous immune globulin therapy. J Pediatr 117(5):741–743
Matthews WJ Jr et al (1980) Hypogammaglobulinemia in patients with cystic fibrosis. N Engl J Med 302(5):245–249
Wheeler WB et al (1984) Progression of cystic fibrosis lung disease as a function of serum immunoglobulin G levels: a 5-year longitudinal study. J Pediatr 104(5):695–699
Kovacevic M, Grant P, Swedo SE (2015) Use of intravenous immunoglobulin in the treatment of twelve youths with pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections. J Child Adolesc Psychopharmacol 25(1):65–69
Singer HS (1999) PANDAS and immunomodulatory therapy. Lancet 354(9185):1137–1138
Perlmutter SJ et al (1999) Therapeutic plasma exchange and intravenous immunoglobulin for obsessive-compulsive disorder and tic disorders in childhood. Lancet 354(9185):1153–1158
Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Text Revision (DSM-IV-TR). 2000, American Psychiatric Association
Gupta S (1999) Treatment of children with autism with intravenous immunoglobulin. J Child Neurol 14(3):203–205
Gupta S, Aggarwal S, Heads C (1996) Dysregulated immune system in children with autism: beneficial effects of intravenous immune globulin on autistic characteristics. J Autism Dev Disord 26(4):439–452
Gupta S (2000) Immunological treatments for autism. J Autism Dev Disord 30(5):475–479
Plioplys AV (1998) Intravenous immunoglobulin treatment of children with autism. J Child Neurol 13(2):79–82
DelGiudice-Asch G et al (1999) Brief report: a pilot open clinical trial of intravenous immunoglobulin in childhood autism. J Autism Dev Disord 29(2):157–160
Raanani P et al (2008) Immunoglobulin prophylaxis in hematological malignancies and hematopoietic stem cell transplantation. Cochrane Database Syst Rev 4, CD006501
Abdel-Mageed A et al (1999) Comparison of two doses of intravenous immunoglobulin after allogeneic bone marrow transplants. Bone Marrow Transplant 23(9):929–932
Krampe K et al (2010) The value of immunoprophylaxis for cytomegalovirus infection with intravenous immunoglobulin in pediatric liver transplant recipients receiving a low-dose immunosupressive regimen. Pediatr Transplant 14(1):67–71
Anyaegbu EI et al (2012) Intravenous immunoglobulin therapy in the treatment of BK viremia and nephropathy in pediatric renal transplant recipients. Pediatr Transplant 16(1):E19–E24
Hadden RD, Marreno F (2015) Switch from intravenous to subcutaneous immunoglobulin in CIDP and MMN: improved tolerability and patient satisfaction. Ther Adv Neurol Disord 8(1):14–19
Danieli MG et al (2014) Subcutaneous IgG in immune-mediate diseases: proposed mechanisms of action and literature review. Autoimmunity Rev 13(12):1182–1188
Danieli MG et al (2011) Subcutaneous immunoglobulin in polymyositis and dermatomyositis: a novel application. Autoimmunity Rev 10(3):144–149
Lazzaro C, Lopiano L, Cocito D (2014) Subcutaneous vs intravenous administration of immunoglobulin in chronic inflammatory demyelinating polyneuropathy: an Italian cost-minimization analysis. Neurol Sci: Off J Italian Neurol Soc Italian Soc Clin Neurophysiology 35(7):1023–1034
Berger M (2014) Subcutaneous IgG in neurologic diseases. Immunotherapy 6(1):71–83
Rajabally YA (2015) Long-term immunoglobulin therapy for chronic inflammatory demyelinating polyradiculoneuropathy. Muscle Nerve 51(5):657–661
Conflict of Interest
The authors declare that they have no competing interests.
Disclaimer
The opinions expressed on this document are solely those of the author(s) and do not represent an endorsement by or the views of the US Air Force, the Department of Defense, or the US Government.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wong, P.H., White, K.M. Impact of Immunoglobulin Therapy in Pediatric Disease: a Review of Immune Mechanisms. Clinic Rev Allerg Immunol 51, 303–314 (2016). https://doi.org/10.1007/s12016-015-8499-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12016-015-8499-2