Abstract
Hematopoietic stem cells are maintained in a specialized microenvironment, known as the ‘niche’, within the bone marrow. Understanding the contribution of cellular and molecular components within the bone marrow niche for the maintenance of hematopoietic stem cells is crucial for the success of therapeutic applications. So far, the roles of crucial mechanisms within the bone marrow niche have been explored in transgenic animals in which genetic modifications are ubiquitously introduced in the whole body. The lack of precise tools to explore genetic alterations exclusively within the bone marrow prevents our determination of whether the observed outcomes result from confounding effects from other organs. Here, we developed a new method – ‘whole bone subcutaneous transplantation’- to study the bone marrow niche in transgenic animals precisely. Using immunolabeling of CD45.1 (donor) vs. CD45.2 (recipient) hematopoeitic stem cells, we demonstrated that hematopoeitic stem cells from the host animals colonize the subcutaneously transplanted femurs after transplantation, while the hematopoietic stem cells from the donor disappear. Strikinlgy, the bone marrow niche of these subcutaneously transplanted femurs remain from the donor mice, enabling us to study specifically cells of the bone marrow niche using this model. We also showed that genetic ablation of peri-arteriolar cells specifically in donor femurs reduced the numbers of hematopoietic stem cells in these bones. This supports the use of this strategy as a model, in combination with genetic tools, to evaluate how bone marrow niche specific modifications may impact non-modified hematopoietic stem cells. Thus, this approach can be utilized for genetic manipulation in vivo of specific cell types only within the bone marrow. The combination of whole bone subcutaneous transplantation with rodent transgenic models will facilitate a more precise, complex and comprehensive understanding of existing problems in the study of the hematopoietic stem cell bone marrow niche.
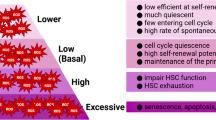
Graphical Abstract













Similar content being viewed by others
Data Availability
Data will be made available on reasonable request.
Abbreviations
- BM:
-
Bone Marrow
- BSA:
-
Bovine Serum Albumin
- CAR:
-
Abundant Reticular Stromal cells
- Cas9:
-
CRISPR-Associated protein 9
- CD:
-
Cluster Differentiation
- CEUA:
-
Ethics Animal Care and Use Committee
- CRE-ER:
-
Cre-Estrogen Receptor (ER)
- CRISPR:
-
Clustered Regularly Interspaced Short Palindromic Repeats
- CXCL12:
-
Chemokine (C-X-C motif) Ligand 12
- DMEM:
-
Dulbecco’s Modified Eagle Mediu
- DT:
-
Diphtheria Toxin
- FBS:
-
Fetal Bovine Serum
- FSC-A:
-
Forward Scatter Area
- FSC-H:
-
Forward Scatter Height
- GFP:
-
Green Fluorescent Protein
- HSC:
-
Hematopoietic Stem Cells
- iDTR:
-
inducible Diphtheria Toxin Receptor
- LKS:
-
Lineage (Lin)− Sca-1+ c-Kit+
- Myh11:
-
Myosin Heavy Chain 11
- NK:
-
Natural Killer
- NOD/SCID:
-
Nonobese Diabetic/Severe Combined Immunodeficiency
- OCT:
-
Tissue-Tek
- PBS:
-
Phosphate-Buffered Saline
- PCR:
-
Polymerase Chain Reaction
- PFA:
-
Paraformaldehyde
- SEM:
-
Standard Error
- TH:
-
Tyrosine Hydroxylase
- UFMG:
-
Federal University of Minas Gerais
- WT:
-
Wild-Type
References
Busch, K., Klapproth, K., Barile, M., Flossdorf, M., Holland-Letz, T., Schlenner, S. M., Reth, M., Hofer, T., & Rodewald, H. R. (2015). Fundamental properties of unperturbed haematopoiesis from stem cells in vivo. Nature, 518(7540), 542–546. https://doi.org/10.1038/nature14242
Naik, S. H., Perie, L., Swart, E., Gerlach, C., van Rooij, N., de Boer, R. J., & Schumacher, T. N. (2013). Diverse and heritable lineage imprinting of early haematopoietic progenitors. Nature, 496(7444), 229–232. https://doi.org/10.1038/nature12013
Schofield, R. (1978). The relationship between the spleen colony-forming cell and the haemopoietic stem cell. Blood Cells, 4(1–2), 7–25.
Birbrair, A., & Frenette, P. S. (2016). Niche heterogeneity in the bone marrow. Annals of the New York Academy of Sciences, 1370(1), 82–96. https://doi.org/10.1111/nyas.13016
Isadora F.G., Sena Pedro H.D.M., Prazeres Gabryella S.P., Santos Isabella T., Borges Patrick O., Azevedo Julia P., Andreotti Viviani M., Almeida Ana E., Paiva Daniel A.P., Guerra Luiza, Lousado Luanny, Souto Akiva, Mintz Alexander, Birbrair (2017) Identity of Gli1+ cells in the bone marrow. Experimental Hematology 5412-16 S0301472X17306124 10.1016/j.exphem.2017.06.349
Daniel A. P., Guerra Ana E., Paiva Isadora F. G., Sena Patrick O., Azevedo Miguel Luiz, Batista Akiva, Mintz Alexander, Birbrair (2018) Adipocytes role in the bone marrow niche. Cytometry Part A 93(2) 167-171 10.1002/cyto.a.23301
Isadora F. G., Sena Isabella T., Borges Luiza, Lousado Patrick O., Azevedo Julia P., Andreotti Viviani M., Almeida Ana E., Paiva Gabryella S. P., Santos Daniel A. P., Guerra Pedro H. D. M., Prazeres Luanny, Souto Akiva, Mintz Alexander, Birbrair (2017) LepR+ cells dispute hegemony with Gli1+ cells in bone marrow fibrosis. Cell Cycle 16(21) 2018-2022 8 10.1080/15384101.2017.1367072
Erika Costa, de Alvarenga Walison N., Silva Rebecca, Vasconcellos Edgar J., Paredes-Gamero Akiva, Mintz Alexander, Birbrair (2018) Promyelocytic leukemia protein in mesenchymal stem cells is essential for leukemia progression. Annals of Hematology 97(10) 1749-1755 10.1007/s00277-018-3463-x
Sawai, C. M., Babovic, S., Upadhaya, S., Knapp, D., Lavin, Y., Lau, C. M., Goloborodko, A., Feng, J., Fujisaki, J., Ding, L., Mirny, L. A., Merad, M., Eaves, C. J., & Reizis, B. (2016). Hematopoietic stem cells are the major source of multilineage hematopoiesis in adult animals. Immunity, 45(3), 597–609. https://doi.org/10.1016/j.immuni.2016.08.007
Wilkinson, A. C., Igarashi, K. J., & Nakauchi, H. (2020). Haematopoietic stem cell self-renewal in vivo and ex vivo. Nature Reviews Genetics, 21(9), 541–554. https://doi.org/10.1038/s41576-020-0241-0
Morrison, S. J., & Scadden, D. T. (2014). The bone marrow niche for haematopoietic stem cells. Nature, 505(7483), 327–334. https://doi.org/10.1038/nature12984
Baccin, C., Al-Sabah, J., Velten, L., Helbling, P. M., Grünschläger, F., Hernández-Malmierca, P., Nombela-Arrieta, C., Steinmetz, L. M., Trumpp, A., & Haas, S. (2020). Combined single-cell and spatial transcriptomics reveal the molecular, cellular and spatial bone marrow niche organization. Nature Cell Biology, 22(1), 38–48. https://doi.org/10.1038/s41556-019-0439-6
Wolock, S. L., Krishnan, I., Tenen, D. E., Matkins, V., Camacho, V., Patel, S., Agarwal, P., Bhatia, R., Tenen, D. G., Klein, A. M., & Welner, R. S. (2019). Mapping distinct bone marrow niche populations and their differentiation Paths. Cell Reports, 28(2), 302-311e305. https://doi.org/10.1016/j.celrep.2019.06.031
Khan, J. A., Mendelson, A., Kunisaki, Y., Birbrair, A., Kou, Y., Arnal-Estape, A., Pinho, S., Ciero, P., Nakahara, F., Ma’ayan, A., Bergman, A., Merad, M., & Frenette, P. S. (2016). Fetal liver hematopoietic stem cell niches associate with portal vessels. Science, 351(6269), 176–180. https://doi.org/10.1126/science.aad0084
Pinho, S., & Frenette, P. S. (2019). Haematopoietic stem cell activity and interactions with the niche. Nature Reviews Molecular Cell Biology, 20(5), 303–320. https://doi.org/10.1038/s41580-019-0103-9
Sánchez-Lanzas, R., Kalampalika, F., & Ganuza, M. ‘Cell-ebrating’ diversity in the bone marrow niche: Classic and novel strategies to uncover niche composition. British Journal of Haematology. https://doi.org/10.1111/bjh.18355
Asada, N., Kunisaki, Y., Pierce, H., Wang, Z., Fernandez Nicolas, F., Birbrair, A., Ma’ayan, A., & Frenette Paul, S. (2017). Differential cytokine contributions of perivascular haematopoietic stem cell niches. Nature Cell Biology, 19(3), 214–223. https://doi.org/10.1038/ncb3475
Miao, R., Chun, H., Feng, X., Gomes, A. C., Choi, J., & Pereira, J. P. (2022). Competition between hematopoietic stem and progenitor cells controls hematopoietic stem cell compartment size. Nature Communications, 13(1), 4611. https://doi.org/10.1038/s41467-022-32228-w
Upadhaya, S., Krichevsky, O., Akhmetzyanova, I., Sawai, C. M., Fooksman, D. R., & Reizis, B. (2020). Intravital Imaging reveals motility of adult hematopoietic stem cells in the bone marrow niche. Cell Stem Cell, 27(2), 336-345e334. https://doi.org/10.1016/j.stem.2020.06.003
Tikhonova, A. N., Dolgalev, I., Hu, H., Sivaraj, K. K., Hoxha, E., Cuesta-Domínguez, Á, Pinho, S., Akhmetzyanova, I., Gao, J., Witkowski, M., Guillamot, M., Gutkin, M. C., Zhang, Y., Marier, C., Diefenbach, C., Kousteni, S., Heguy, A., Zhong, H., Fooksman, D. R., … Aifantis, I. (2019). The bone marrow microenvironment at single-cell resolution. Nature, 569(7755), 222–228. https://doi.org/10.1038/s41586-019-1104-8
Joseph, C., Quach Julie, M., Walkley Carl, R., Lane Steven, W., Lo Celso, C., & Purton Louise, E. (2013). Deciphering hematopoietic stem cells in their niches: a critical Appraisal of genetic models, lineage tracing, and imaging strategies. Cell Stem Cell, 13(5), 520–533. https://doi.org/10.1016/j.stem.2013.10.010
Nobre, A. R., Risson, E., Singh, D. K., Martino, J. D., Cheung, J. F., Wang, J., Johnson, J., Russnes, H. G., Bravo-Cordero, J. J., Birbrair, A., Naume, B., Azhar, M., Frenette, P. S., & JA, A.-G. (2021). Bone marrow NG2+/Nestin + mesenchymal stem cells drive DTC dormancy via TGFβ2. Nature Cancer, 2, 327–339.
Paiva, A. E., Lousado, L., Guerra, D. A. P., Azevedo, P. O., Sena, I. F. G., Andreotti, J. P., Santos, G. S. P., Goncalves, R., Mintz, A., & Birbrair, A. (2018). Pericytes in the Premetastatic Niche. Cancer Research, 78(11), 2779–2786. https://doi.org/10.1158/0008-5472.CAN-17-3883
Picoli, C. C., Goncalves, B. O. P., Santos, G. S. P., Rocha, B. G. S., Costa, A. C., Resende, R. R., & Birbrair, A. (2021). Pericytes cross-talks within the tumor microenvironment. Biochimica Et Biophysica Acta - Reviews on Cancer, 1876(2), 188608. https://doi.org/10.1016/j.bbcan.2021.188608
Picoli, C. C., Costa, A. C., Rocha, B. G. S., Silva, W. N., Santos, G. S. P., Prazeres, P., Costa, P. A. C., Oropeza, A., da Silva, R. A., Azevedo, V. A. C., Resende, R. R., Cunha, T. M., Mintz, A., & Birbrair, A. (2021). Sensory nerves in the spotlight of the stem cell niche. Stem Cells Translational Medicine, 10(3), 346–356. https://doi.org/10.1002/sctm.20-0284
McLellan, M. A., Rosenthal, N. A., & Pinto, A. R. (2017). Cre-loxp-mediated recombination: general principles and experimental considerations. Current Protocols in Mouse Biology, 7(1), 1–12. https://doi.org/10.1002/cpmo.22
Janssens, R., Struyf, S., & Proost, P. (2018). The unique structural and functional features of CXCL12. Cellular & Molecular Immunology, 15(4), 299–311. https://doi.org/10.1038/cmi.2017.107
Turan, S., Galla, M., Ernst, E., Qiao, J., Voelkel, C., Schiedlmeier, B., Zehe, C., & Bode, J. (2011). Recombinase-mediated Cassette Exchange (RMCE): traditional concepts and current challenges. Journal of Molecular Biology, 407(2), 193–221. https://doi.org/10.1016/j.jmb.2011.01.004
Madisen, L., Zwingman, T. A., Sunkin, S. M., Oh, S. W., Zariwala, H. A., Gu, H., Ng, L. L., Palmiter, R. D., Hawrylycz, M. J., Jones, A. R., Lein, E. S., & Zeng, H. (2010). A robust and high-throughput cre reporting and characterization system for the whole mouse brain. Nature Neuroscience, 13(1), 133–140. https://doi.org/10.1038/nn.2467
Prazeres, P., Leonel, C., Silva, W. N., Rocha, B. G. S., Santos, G. S. P., Costa, A. C., Picoli, C. C., Sena, I. F. G., Goncalves, W. A., Vieira, M. S., Costa, P. A. C., Campos, L., Lopes, M. T. P., Costa, M. R., Resende, R. R., Cunha, T. M., Mintz, A., & Birbrair, A. (2020). Ablation of sensory nerves favours melanoma progression. Journal of Cellular and Molecular Medicine. https://doi.org/10.1111/jcmm.15381
Costa, P. A. C., Silva, W. N., Prazeres, P., Picoli, C. C., Guardia, G. D. A., Costa, A. C., Oliveira, M. A., Guimaraes, P. P. G., Goncalves, R., Pinto, M. C. X., Amorim, J. H., Azevedo, V. A. C., Resende, R. R., Russo, R. C., Cunha, T. M., Galante, P. A. F., Mintz, A., & Birbrair, A. (2021). Chemogenetic modulation of sensory neurons reveals their regulating role in melanoma progression. Acta Neuropathologica Communications, 9(1), 183. https://doi.org/10.1186/s40478-021-01273-9
Tenza-Ferrer, H., Collodetti, M., Nicolau, E. S., Birbrair, A., Magno, L. A. V., & Romano-Silva, M. A. (2022). Transiently Nav1.8-expressing neurons are capable of sensing noxious stimuli in the brain. Frontiers in Cellular Neuroscience, 16, 933874. https://doi.org/10.3389/fncel.2022.933874
Rocha, B. G. S., Picoli, C. C., Gonçalves, B. O. P., Silva, W. N., Costa, A. C., Moraes, M. M., Costa, P. A. C., Santos, G. S. P., Almeida, M. R., Silva, L. M., Singh, Y., Falchetti, M., Guardia, G. D. A., Guimaraes, P. P. G., Russo, R. C., Resende, R. R., Pinto, M. C. X., Amorim, J. H., Azevedo, V. A. C., … Birbrair, A. (2022). Tissue–resident glial cells associate with tumoral vasculature and promote cancer progression. Angiogenesis. In press. https://doi.org/10.1007/s10456-022-09858-1
Buch, T., Heppner, F. L., Tertilt, C., Heinen, T. J., Kremer, M., Wunderlich, F. T., Jung, S., & Waisman, A. (2005). A cre-inducible diphtheria toxin receptor mediates cell lineage ablation after toxin administration. Nature Methods, 2(6), 419–426. https://doi.org/10.1038/nmeth762
Mercier, F. E., Sykes, D. B., & Scadden, D. T. (2016). Single targeted exon mutation creates a true congenic mouse for competitive hematopoietic stem cell transplantation: the C57BL/6-CD45.1(STEM) mouse. Stem Cell Reports, 6(6), 985–992. https://doi.org/10.1016/j.stemcr.2016.04.010
Ara, T., Tokoyoda, K., Sugiyama, T., Egawa, T., Kawabata, K., & Nagasawa, T. J. I. (2003). Long-term hematopoietic stem cells require stromal cell-derived factor-1 for colonizing bone marrow during ontogeny. 19 (2):257–267
Yahata, T., Ando, K., Sato, T., Miyatake, H., Nakamura, Y., Muguruma, Y., Kato, S., & Hotta, T. (2003). A highly sensitive strategy for SCID-repopulating cell assay by direct injection of primitive human hematopoietic cells into NOD/SCID mice bone marrow. Blood 101 (8):2905–2913. https://doi.org/10.1182/blood-2002-07-1995
Herring, B. P., Hoggatt, A. M., Burlak, C., & Offermanns, S. (2014). Previously differentiated medial vascular smooth muscle cells contribute to neointima formation following vascular injury. Vasc Cell, 6, 21. https://doi.org/10.1186/2045-824X-6-21
Nikolakopoulou, A. M., Montagne, A., Kisler, K., Dai, Z., Wang, Y., Huuskonen, M. T., Sagare, A. P., Lazic, D., Sweeney, M. D., Kong, P., Wang, M., Owens, N. C., Lawson, E. J., Xie, X., Zhao, Z., & Zlokovic, B. V. (2019). Pericyte loss leads to circulatory failure and pleiotrophin depletion causing neuron loss. Nature Neuroscience, 22(7), 1089–1098. https://doi.org/10.1038/s41593-019-0434-z
Cha, J. H., Chang, M. Y., Richardson, J. A., & Eidels, L. (2003). Transgenic mice expressing the diphtheria toxin receptor are sensitive to the toxin. Molecular Microbiology, 49(1), 235–240. https://doi.org/10.1046/j.1365-2958.2003.03550.x
Hanoun, M., Zhang, D., Mizoguchi, T., Pinho, S., Pierce, H., Kunisaki, Y., Lacombe, J., Armstrong, S. A., Duhrsen, U., & Frenette, P. S. (2014). Acute myelogenous leukemia-induced sympathetic neuropathy promotes malignancy in an altered hematopoietic stem cell niche. Cell Stem Cell, 15(3), 365–375. https://doi.org/10.1016/j.stem.2014.06.020
Andrade, J., Ge, S., Symbatyan, G., Rosol, M. S., Olch, A. J., & Crooks, G. M. (2011). Effects of sublethal irradiation on patterns of engraftment after murine bone marrow transplantation. Biology of blood and marrow transplantation: journal of the American Society for Blood and Marrow Transplantation 17 (5):608–619. https://doi.org/10.1016/j.bbmt.2010.12.697
Sena, I. F. G., Rocha, B. G. S., Picoli, C. C., Santos, G. S. P., Costa, A. C., Goncalves, B. O. P., Garcia, A. P. V., Soltani-Asl, M., Coimbra-Campos, L. M. C., Silva, W. N., Costa, P. A. C., Pinto, M. C. X., Amorim, J. H., Azevedo, V. A. C., Resende, R. R., Heller, D., Cassali, G. D., Mintz, A., & Birbrair, A. (2021). C(3)1-TAg in C57BL/6 J background as a model to study mammary tumor development. Histochemistry And Cell Biology. https://doi.org/10.1007/s00418-021-01995-w
Gilson Sena, I. F., Fernandes, L. L., Lorandi, L. L., Santana, T. V., Cintra, L., Lima, I. F., Iwai, L. K., Kramer, J. M., Birbrair, A., & Heller, D. (2022). Identification of early biomarkers in saliva in genetically engineered mouse model C(3)1-TAg of breast cancer. Scientific Reports, 12(1), 11544. https://doi.org/10.1038/s41598-022-14514-1
Gomes, N. A., do Valle, I. B., Gleber-Netto, F. O., Silva, T. A., Oliveira, H. M. C., de Oliveira, R. F., Ferreira, L. A. Q., Castilho, L. S., Reis, P., Prazeres, P., Menezes, G. B., de Magalhaes, C. S., Mesquita, R. A., Marques, M. M., Birbrair, A., & Diniz, I. M. A. (2022). Nestin and NG2 transgenes reveal two populations of perivascular cells stimulated by photobiomodulation. Journal Of Cellular Physiology, 237(4), 2198–2210. https://doi.org/10.1002/jcp.30680
Coimbra-Campos, L. M. C., Silva, W. N., Baltazar, L. M., Costa, P. A. C., Prazeres, P., Picoli, C. C., Costa, A. C., Rocha, B. G. S., Santos, G. S. P., Oliveira, F. M. S., Pinto, M. C. X., Amorim, J. H., Azevedo, V. A. C., Souza, D. G., Russo, R. C., Resende, R. R., Mintz, A., & Birbrair, A. (2021). Circulating Nestin-GFP(+) cells participate in the pathogenesis of Paracoccidioides brasiliensis in the lungs. Stem Cell Rev Rep, 17(5), 1874–1888. https://doi.org/10.1007/s12015-021-10181-3
Birbrair, A., Sattiraju, A., Zhu, D., Zulato, G., Batista, I., Nguyen, V. T., Messi, M. L., Solingapuram Sai, K. K., Marini, F. C., Delbono, O., & Mintz, A. (2017). Novel peripherally derived neural-like Stem cells as therapeutic carriers for treating glioblastomas. Stem Cells Translational Medicine, 6(2), 471–481. https://doi.org/10.5966/sctm.2016-0007
Birbrair, A., Wang, Z. M., Messi, M. L., Enikolopov, G. N., & Delbono, O. (2011). Nestin-GFP transgene reveals neural precursor cells in adult skeletal muscle. PLoS One1, 6(2), e16816. https://doi.org/10.1371/journal.pone.0016816
Birbrair, A., Zhang, T., Files, D. C., Mannava, S., Smith, T., Wang, Z. M., Messi, M. L., Mintz, A., & Delbono, O. (2014). Type-1 pericytes accumulate after tissue injury and produce collagen in an organ-dependent manner. Stem Cell Research & Therapy, 5(6), 122. https://doi.org/10.1186/scrt512
Birbrair, A., Zhang, T., Wang, Z. M., Messi, M. L., Enikolopov, G. N., Mintz, A., & Delbono, O. (2013). Role of pericytes in skeletal muscle regeneration and fat accumulation. Stem Cells and Development, 22(16), 2298–2314. https://doi.org/10.1089/scd.2012.0647
Birbrair, A., Zhang, T., Wang, Z. M., Messi, M. L., Enikolopov, G. N., Mintz, A., & Delbono, O. (2013). Skeletal muscle pericyte subtypes differ in their differentiation potential. Stem Cell Res, 10(1), 67–84. https://doi.org/10.1016/j.scr.2012.09.003
Birbrair, A., Zhang, T., Wang, Z. M., Messi, M. L., Enikolopov, G. N., Mintz, A., & Delbono, O. (2013). Skeletal muscle neural progenitor cells exhibit properties of NG2-glia. Experimental Cell Research, 319(1), 45–63. https://doi.org/10.1016/j.yexcr.2012.09.008
Birbrair, A., Zhang, T., Wang, Z. M., Messi, M. L., Mintz, A., & Delbono, O. (2013). Type-1 pericytes participate in fibrous tissue deposition in aged skeletal muscle. American Journal of Physiology Cell Physiology, 305(11), C1098-1113. https://doi.org/10.1152/ajpcell.00171.2013
Birbrair, A., Zhang, T., Wang, Z. M., Messi, M. L., Olson, J. D., Mintz, A., & Delbono, O. (2014). Type-2 pericytes participate in normal and tumoral angiogenesis. American Journal of Physiology Cell Physiology, 307(1), C25-38. https://doi.org/10.1152/ajpcell.00084.2014
Kawamoto, T. (2003). Use of a new adhesive film for the preparation of multi-purpose fresh-frozen sections from hard tissues, whole-animals, insects and plants. Archives of Histology and Cytology, 66(2), 123–143. https://doi.org/10.1679/aohc.66.123
Kunisaki, Y., Bruns, I., Scheiermann, C., Ahmed, J., Pinho, S., Zhang, D., Mizoguchi, T., Wei, Q., Lucas, D., Ito, K., Mar, J. C., Bergman, A., & Frenette, P. S. (2013). Arteriolar niches maintain haematopoietic stem cell quiescence. Nature, 502(7473), 637–643. https://doi.org/10.1038/nature12612
Swamydas, M., & Lionakis, M. S. (2013). Isolation, purification and labeling of mouse bone marrow neutrophils for functional studies and adoptive transfer experiments. Journal of Visualized Experiments: JoVE, (77), e50586–e50586. https://doi.org/10.3791/50586.
Pinho, S., Lacombe, J., Hanoun, M., Mizoguchi, T., Bruns, I., Kunisaki, Y., & Frenette, P. S. (2013). PDGFRalpha and CD51 mark human nestin + sphere-forming mesenchymal stem cells capable of hematopoietic progenitor cell expansion. Journal of Experimental Medicine, 210(7), 1351–1367. https://doi.org/10.1084/jem.20122252
Hudson, W. A., Li, Q., Le, C., & Kersey, J. H. (1998). Xenotransplantation of human lymphoid malignancies is optimized in mice with multiple immunologic defects. Leukemia, 12(12), 2029–2033. https://doi.org/10.1038/sj.leu.2401236
Danesh-Sani, S. A., Tarnow, D., Yip, J. K., & Mojaver, R. (2017). The influence of cortical bone perforation on guided bone regeneration in humans. International Journal of Oral and Maxillofacial Surgery, 46(2), 261–266. https://doi.org/10.1016/j.ijom.2016.10.017
Yuuki, H., Yoshikai, Y., Kishihara, K., Matsuzaki, G., Ayukawa, K., & Nomoto, K. (1989). The expression and sequences of T cell antigen receptor beta-chain genes in the thymus at an early stage after sublethal irradiation. The Journal of Immunology, 142(10), 3683–3691.
Xiao, S., Shterev, I. D., Zhang, W., Young, L., Shieh, J. H., Moore, M., van den Brink, M., Sempowski, G. D., & Manley, N. R. (2017). Sublethal total body irradiation causes long-term deficits in Thymus function by reducing lymphoid progenitors. The Journal of Immunology, 199(8), 2701–2712. https://doi.org/10.4049/jimmunol.1600934
Wang, Y., Schulte, B. A., LaRue, A. C., Ogawa, M., & Zhou, D. (2006). Total body irradiation selectively induces murine hematopoietic stem cell senescence. Blood, 107(1), 358–366. https://doi.org/10.1182/blood-2005-04-1418
Agarwal, A., Morrone, K., Bartenstein, M., Zhao, Z. J., Verma, A., & Goel, S. (2016). Bone marrow fibrosis in primary myelofibrosis: pathogenic mechanisms and the role of TGF-beta. Stem Cell Investig, 3, 5. https://doi.org/10.3978/j.issn.2306-9759.2016.02.03
Borjesson, A. E., Windahl, S. H., Karimian, E., Eriksson, E. E., Lagerquist, M. K., Engdahl, C., Antal, M. C., Krust, A., Chambon, P., Savendahl, L., & Ohlsson, C. (2012). The role of estrogen receptor-alpha and its activation function-1 for growth plate closure in female mice. American Journal of Physiology. Endocrinology and Metabolism, 302(11), E1381-1389. https://doi.org/10.1152/ajpendo.00646.2011
Zhong, R. (1999). Organ transplantation in mice: current status and future prospects. Microsurgery, 19(2), 52–55. https://doi.org/10.1002/(sici)1098-2752(1999)19:2<52::aid-micr2>3.0.co;2-m
Mawdsley, R., & Harrison, G. A. (1963). Environmental factors determining the growth and development of whole bone transplants. Journal of Embryology and Experimental Morphology, 11, 537–547.
Felts, W. J. (1959). Transplantation studies of factors in skeletal organogenesis. I. The subcutaneously implanted immature long-bone of the rat and mouse. American Journal of Physical Anthropology, 17(3), 201–215. https://doi.org/10.1002/ajpa.1330170306
Acknowledgements
Alexander Birbrair is supported by a research productivity fellowship from Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq-PQ2), a grant from Instituto Serrapilheira/Serra-1708-15285, a grant from Pró-reitoria de Pesquisa/Universidade Federal de Minas Gerais (PRPq/UFMG) (Edital 05/2016); a grant from Fundação de Amparo à Pesquisa do Estado de Minas Gerais - FAPEMIG (Chamada N°01/2021 – Demanda Universal, APQ-01321-21); a grant from FAPEMIG [Rede Mineira de Pesquisa Translacional em Imunobiológicos e Biofármacos no Câncer (REMITRIBIC, RED-00031-21)]; a grant from FAPEMIG [Rede Mineira de Engenharia de Tecidos e Terapia Celular (REMETTEC, RED-00570-16)]; a grant from FAPEMIG [Rede De Pesquisa Em Doenças Infecciosas Humanas E Animais Do Estado De Minas Gerais (RED-00313-16)]; and a grant from MCTIC/CNPq Nº 28/2018 (Universal/Faixa A). Akiva Mintz is supported by the National Institute of Health (1R01CA179072-01A1) and by the American Cancer Society Mentored Research Scholar grant (124443-MRSG-13-121-01-CDD). This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001, as Thamires Righi was supported by a PrInt/CAPES fellowship. Caroline C. Picoli was supported by doctoral fellowships from CAPES. Patricia R. Martins was supported by a postdoctoral fellowship (PDJ) from CNPq. The authors also thank CAPI (UFMG) for microscopical technical support and Laboratory of Flow Cytometry at the Instituto de Ciências Biológicas/UFMG (http://labs.icb.ufmg.br/citometria/)” for providing the equipment and technical support for experiments involving flow cytometry.
Funding
Alexander Birbrair is supported by a research productivity fellowship from Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq-PQ2), a grant from Instituto Serrapilheira/Serra-1708-15285, a grant from Pró-reitoria de Pesquisa/Universidade Federal de Minas Gerais (PRPq/UFMG) (Edital 05/2016); a grant from Fundação de Amparo à Pesquisa do Estado de Minas Gerais - FAPEMIG (Chamada N°01/2021 – Demanda Universal, APQ-01321-21); a grant from FAPEMIG [Rede Mineira de Pesquisa Translacional em Imunobiológicos e Biofármacos no Câncer (REMITRIBIC, RED-00031-21)]; a grant from FAPEMIG [Rede Mineira de Engenharia de Tecidos e Terapia Celular (REMETTEC, RED-00570-16)]; a grant from FAPEMIG [Rede De Pesquisa Em Doenças Infecciosas Humanas E Animais Do Estado De Minas Gerais (RED-00313-16)]; and a grant from MCTIC/CNPq Nº 28/2018 (Universal/Faixa A). Akiva Mintz is supported by the National Institute of Health (1R01CA179072-01A1) and by the American Cancer Society Mentored Research Scholar grant (124443-MRSG-13-121-01-CDD). Caroline C. Picoli was supported by doctoral fellowships from CAPES. Patricia R. Martins was supported by a postdoctoral fellowship (PDJ) from CNPq. The authors also thank CAPI (UFMG) for microscopical technical support and Laboratory of Flow Cytometry at the Instituto de Ciências Biológicas/UFMG (http://labs.icb.ufmg.br/citometria/)” for providing the equipment and technical support for experiments involving flow cytometry.
Author information
Authors and Affiliations
Contributions
AB conceived and supervised the study; CCP, PRM, XLCW, TR, PPGG, MCXP, JHA, VACA, SRP, AK, FCC, RRR, AM, AB analyzed the data and discussed the results; AB and PSF were responsible for funding; AM and AB wrote the original draft; all authors contributed to and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Consent to Participate
Not applicable.
Consent to Publish
Not applicable.
Competing Interests
The authors indicate no potential conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Caroline C. Picoli and Patrícia Rocha Martins contributed equally and were co-first authors in this manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.

Supplementary Fig. 1
Transplantation of whole bone with the surrounding skeletal muscle does not improve the amount of hematopoietic stem cells in the subcutaneously transplanted bones. A C57BL6-derived femur with surrounding skeletal muscle subcutaneous transplantation into recipient NOD/SCID mice scheme. Whole femurs with muscle from C57BL6 mouse were implanted subcutaneously into NOD/SCID mice. After 45 days, the subcutaneously transplanted femurs from donor C57BL6 were collected for analysis. B Representative flow cytometry dot plots of bone marrow cells are shown. Data were assessed by flow cytometry analysis of bone marrow cells isolated from the femurs. Representative flow cytometry plots of femurs with surrounding skeletal muscle from C57BL6 mice implanted subcutaneously into C57BL6 mice analyzed after 45 days. The gating strategy was applied to analyze LSK (Sca-1 + c-kit + Lineage − gated). (PNG 429 KB)

Supplementary Fig. 2
Transplantation of whole bone with the surrounding skeletal muscle does not improve the amount of hematopoietic stem cells in the subcutaneously transplanted bones. A C57BL6-derived femur with surrounding skeletal muscle subcutaneous transplantation into recipient NOD/SCID mice scheme. Whole femurs with muscle from C57BL6 mouse were implanted subcutaneously into NOD/SCID mice. After 45 days, the subcutaneously transplanted femurs from donor C57BL6 were collected for analysis. B Representative flow cytometry dot plots of bone marrow cells are shown. Data were assessed by flow cytometry analysis of bone marrow cells isolated from the femurs. Representative flow cytometry plots of femurs with surrounding skeletal muscle from C57BL6 mice implanted subcutaneously into C57BL6 mice analyzed after 45 days. The gating strategy was applied to analyze LSK (Sca-1 + c-kit + Lineage − gated). (PNG 4.16 MB)

Supplementary Fig. 3
Subcutaneously transplanted bones lack sympathetic innervation. A Schematic diagram of femurs derived from Myh11CreER/TdTomato mice subcutaneously transplanted into C57BL6 WT mice. Femurs from Myh11CreER/TdTomato mice were dissected and transplanted subcutaneously into recipient C57BL6 WT mice. After 3 months, the animals were submitted to tamoxifen treatment for 5 days, and, after 2 days, the subcutaneously transplanted femurs were collected for analyses. B Representative photomicrograph of a femur section showing Myh11CreER+/TdTomato+ peri-arteriolar cells (red), CD31+/CD144+ blood vessels (blue), TH+ sympathetic nerve fibers (green) and DAPI+ nuclei (white). (PNG 3.05 MB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Picoli, C.C., Martins, P.R., Wong, X.L.C. et al. Whole bone subcutaneous transplantation as a strategy to study precisely the bone marrow niche. Stem Cell Rev and Rep 19, 906–927 (2023). https://doi.org/10.1007/s12015-022-10496-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12015-022-10496-9