Abstract
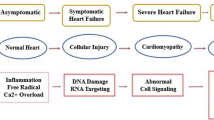
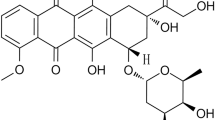
Doxorubicin (DOX) is the cornerstone of chemotherapy. However, it has dose-dependent cardiotoxic events that limit its clinical use. This study was intended to investigate the efficiency of DOX as an anti-cancer against the MCF-7 cell line in the presence of diosmin (DIO) and to appraise the protective impact of DIO against DOX cardiotoxicity in vivo. In vitro study was carried out to establish the conservation of DOX cytotoxicity in the presence of DIO. In vivo study was conducted on 42 adult female Wistar rats that were equally allocated into 6 groups; control, DIO (100 mg/kg), DIO (200 mg/kg), DOX (20 mg/kg, single dose i.p.), DIO (100 mg/kg) + DOX, received DIO orally (100 mg/kg) for 30 days, then administrated with a single dose of DOX and DIO (200 mg/kg) + DOX, received DIO orally (200 mg/kg) for 30 days, then administrated with DOX. In vitro study showed preservation of cytotoxic activity of DOX on MCF-7 in the presence of DIO. In vivo study indicated that DOX altered electrocardiograph (ECG) parameters. Also, it yielded a significant rise in CK-MB, cTnT and LDH serum levels and cardiac contents of MDA, IL-1β; paralleled by a significant drop in cardiac IL-10 and SOD. Moreover, significant upregulation of Bax, TNF-α, and HIF-1α, in concomitant with significant downregulation of Bcl-2 mRNA in cardiac tissue have been recorded in the DOX group. Furthermore, histopathological description of cardiac tissues showed that DOX alters normal cardiac histoarchitecture. On the opposite side, DIO pretreatment could ameliorate ECG parameters, suppress IL-1β and enhanceIL-10, promote activity of SOD and repress MDA. Additionally, downregulation of Bax, TNF-α, HIF-1α and upregulation of Bcl-2 have been demonstrated in DIO-pretreated rats. Furthermore, the histopathological examination of cardiac tissues illustrated that DIO had a favorable impact on the protection of heart histoarchitecture. DIO is suggested for protection against acute cardiotoxicity caused by DOX without affecting antitumor activity.



Similar content being viewed by others
References
Attachaipanich, T., Chattipakorn, S. C., & Chattipakorn, N. (2023). Potential roles of melatonin in doxorubicin-induced cardiotoxicity: From cellular mechanisms to clinical application. Pharmaceutics, 15(3), 785.
Cheah, I. K., Tang, R. M., Wang, X., Sachaphibulkij, K., Chong, S. Y., Lim, L. H., & Halliwell, B. (2023). Protection against doxorubicin-induced cardiotoxicity by ergothioneine. Antioxidants, 12(2), 320.
Raj, P., Louis, X. L., Thandapilly, S. J., Movahed, A., Zieroth, S., & Netticadan, T. (2014). Potential of resveratrol in the treatment of heart failure. Life Sciences, 95(2), 63–71.
Swain, S. M., Whaley, F. S., & Ewer, M. S. (2003). Congestive heart failure in patients treated with doxorubicin: A retrospective analysis of three trials. Cancer: Interdisciplinary International Journal of the American Cancer Society, 97(11), 2869–2879.
Rawat, P. S., Jaiswal, A., Khurana, A., Bhatti, J. S., & Navik, U. (2021). Doxorubicin-induced cardiotoxicity: An update on the molecular mechanism and novel therapeutic strategies for effective management. Biomedicine & Pharmacotherapy, 139, 111708.
Li, S., Amat, D., Peng, Z., Vanni, S., Raskin, S., De Angulo, G., & Leblanc, R. M. (2016). Transferrin conjugated nontoxic carbon dots for doxorubicin delivery to target pediatric brain tumor cells. Nanoscale, 8(37), 16662–16669.
Menna, P., & Salvatorelli, E. (2017). Primary prevention strategies for anthracycline cardiotoxicity: A brief overview. Chemotherapy, 62(3), 159–168.
Rocha, P. D. S. D., Campos, J. F., Nunes-Souza, V., Vieira, M. D. C., Boleti, A. P. D. A., Rabelo, L. A., & de Picoli Souza, K. (2018). Antioxidant and protective effects of schinus terebinthifolius raddi against doxorubicin-induced toxicity. Applied Biochemistry and Biotechnology, 184, 869–884.
Jang, H. M., Lee, J. Y., An, H. S., Ahn, Y. J., Jeong, E. A., Shin, H. J., & Roh, G. S. (2022). LCN2 deficiency ameliorates doxorubicin-induced cardiomyopathy in mice. Biochemical and Biophysical Research Communications, 588, 8–14.
Seara, F. A., Kasai-Brunswick, T. H., Nascimento, J. H., & Campos-de-Carvalho, A. C. (2022). Anthracycline-induced cardiotoxicity and cell senescence: New therapeutic option? Cellular and Molecular Life Sciences, 79(11), 568.
Cheng, X., Liu, D., Song, H., Tian, X., Yan, C., & Han, Y. (2021). Overexpression of Kininogen-1 aggravates oxidative stress and mitochondrial dysfunction in DOX-induced cardiotoxicity. Biochemical and Biophysical Research Communications, 550, 142–150.
Mizuta, Y., Akahoshi, T., Eto, H., Hyodo, F., Murata, M., Tokuda, K., & Yamaura, K. (2022). Noninvasive diagnosis of the mitochondrial function of doxorubicin-induced cardiomyopathy using in vivo dynamic nuclear polarization–magnetic resonance imaging. Antioxidants, 11(8), 1454.
Kajarabille, N., & Latunde-Dada, G. O. (2019). Programmed cell-death by ferroptosis: Antioxidants as mitigators. International Journal of Molecular Sciences, 20(19), 4968.
Kourek, C., Touloupaki, M., Rempakos, A., Loritis, K., Tsougkos, E., Paraskevaidis, I., & Briasoulis, A. (2022). Cardioprotective strategies from cardiotoxicity in cancer patients: A comprehensive review. Journal of Cardiovascular Development and Disease, 9(8), 259.
Injac, R., Boskovic, M., Perse, M., Koprivec-Furlan, E., Cerar, A., Djordjevic, A., & Strukelj, B. (2008). Acute doxorubicin nephrotoxicity in rats with malignant neoplasm can be successfully treated with fullerenol C60 (OH) 24 via suppression of oxidative stress. Pharmacological Reports, 60(5), 742.
Salzer, W. L., Devidas, M., Carroll, W. L., Winick, N., Pullen, J., Hunger, S. P., & Camitta, B. A. (2010). Long-term results of the pediatric oncology group studies for childhood acute lymphoblastic leukemia 1984–2001: A report from the children’s oncology group. Leukemia, 24(2), 355–370.
Zhang, Y., Ma, X. Y., Zhang, T., Qin, M., Sun, B., Li, Q., Hu, D.-W., & Ren, L. Q. (2019). Protective effects of apocynum venetum against pirarubicin-induced cardiotoxicity. The American Journal of Chinese Medicine, 47(05), 1075–1097.
Jones, R. L. (2008). Utility of dexrazoxane for the reduction of anthracycline-induced cardiotoxicity. Expert Review of Cardiovascular Therapy, 6(10), 1311–1317.
Silber, J. H. (2004). Can dexrazoxane reduce myocardial injury in anthracycline-treated children with acute lymphoblastic leukemia? Nature Clinical Practice Oncology, 1(1), 16–17.
Shaikh, F., Dupuis, L. L., Alexander, S., Gupta, A., Mertens, L., & Nathan, P. C. (2015). Cardioprotection and second malignant neoplasms associated with dexrazoxane in children receiving anthracycline chemotherapy: A systematic review and meta-analysis. JNCI: Journal of the National Cancer Institute, 108(4), djv357.
Psotová, J. (2004). Chemoprotective effect of plant phenolics against anthracycline-induced toxicity on rat cardiomyocytes. Part III. Apigenin, baicalelin, kaempherol, luteolin and quercetin. Phytotherapy Research, 18, 516–521.
Eraslan, G., Sarıca, Z. S., Bayram, L. Ç., Tekeli, M. Y., Kanbur, M., & Karabacak, M. (2017). The effects of diosmin on aflatoxin-induced liver and kidney damage. Environmental Science and Pollution Research, 24, 27931–27941.
Rashid, S., Ali, N., Nafees, S., Ahmad, S. T., Arjumand, W., Hasan, S. K., & Sultana, S. (2013). Alleviation of doxorubicin-induced nephrotoxicity and hepatotoxicity by chrysin in Wistar rats. Toxicology Mechanisms and Methods, 23(5), 337–345.
Ağır, M. S., & Eraslan, G. (2019). The effect of diosmin against liver damage caused by cadmium in rats. Journal of Food Biochemistry, 43(9), e12966.
Shalkami, A. S., Hassan, M. I. A., & Bakr, A. G. (2018). Anti-inflammatory, antioxidant and anti-apoptotic activity of diosmin in acetic acid-induced ulcerative colitis. Human & Experimental Toxicology, 37(1), 78–86.
Abdel-Daim, M. M., Khalifa, H. A., Abushouk, A. I., Dkhil, M. A., & Al-Quraishy, S. A. (2017). Diosmin attenuates methotrexate-induced hepatic, renal, and cardiac injury: A biochemical and histopathological study in mice. Oxidative Medicine and Cellular Longevity, 2017, 3281670.
Skehan, P., Storeng, R., Scudiero, D., Monks, A., McMahon, J., Vistica, D., & Boyd, M. R. (1990). New colorimetric cytotoxicity assay for anticancer-drug screening. JNCI: Journal of the National Cancer Institute, 82(13), 1107–1112.
Mahgoub, S., Sallam, A. O., Sarhan, H. K., Ammar, A. A., & Soror, S. H. (2020). Role of Diosmin in protection against the oxidative stress induced damage by gamma-radiation in Wistar albino rats. Regulatory Toxicology and Pharmacology, 113, 104622.
Rehman, Tahir, M. U., Khan, M., Khan, A. Q., Oday-O-Hamiza, R., Lateef, A., & Sultana, S. (2014). D-limonene suppresses doxorubicin-induced oxidative stress and inflammation via repression of COX-2, iNOS, and NFκB in kidneys of Wistar rats. Experimental Biology and Medicine, 239(4), 465–476.
Hajrasouliha, A. R., Tavakoli, S., Jabehdar-Maralani, P., Shafaroodi, H., Borhani, A. A., Houshmand, G., & Dehpour, A. R. (2004). Resistance of cholestatic rats against epinephrine-induced arrhythmia: The role of nitric oxide and endogenous opioids. European Journal of Pharmacology, 499(3), 307–313.
Mustafa, H. N., Hegazy, G. A., El Awdan, S. A., & AbdelBaset, M. (2017). Protective role of CoQ10 or L-carnitine on the integrity of the myocardium in doxorubicin induced toxicity. Tissue and Cell, 49(3), 410–426.
Banchroft, J. D., Stevens, A., & Turner, D. R. (1996) Theory and practice of histological techniques (4th ed.). Churchill Livingstone.
McGowan, J. V., Chung, R., Maulik, A., Piotrowska, I., Walker, J. M., & Yellon, D. M. (2017). Anthracycline chemotherapy and cardiotoxicity. Cardiovascular Drugs and Therapy, 31, 63–75.
Mitry, M. A., & Edwards, J. G. (2016). Doxorubicin induced heart failure: Phenotype and molecular mechanisms. IJC Heart & Vasculature, 10, 17–24.
Nebigil, C. G., & Désaubry, L. (2018). Updates in anthracycline-mediated cardiotoxicity. Frontiers in Pharmacology, 9, 1262.
Angsutararux, P., Luanpitpong, S., & Issaragrisil, S. (2015). Chemotherapy-induced cardiotoxicity: Overview of the roles of oxidative stress. Oxidative Medicine and Cellular Longevity, 2015, 795602.
Xiao, J., Sun, G. B., Sun, B., Wu, Y., He, L., Wang, X., & Sun, X. B. (2012). Kaempferol protects against doxorubicin-induced cardiotoxicity in vivo and in vitro. Toxicology, 292(1), 53–62.
Goyal, V., Bews, H., Cheung, D., Premecz, S., Mandal, S., Shaikh, B., & Jassal, D. S. (2016). The cardioprotective role of N-acetyl cysteine amide in the prevention of doxorubicin and trastuzumab–mediated cardiac dysfunction. Canadian Journal of Cardiology, 32(12), 1513–1519.
Cappetta, D., Rossi, F., Piegari, E., Quaini, F., Berrino, L., Urbanek, K., & De Angelis, A. (2018). Doxorubicin targets multiple players: A new view of an old problem. Pharmacological Research, 127, 4–14.
Annapurna, A., Reddy, C. S., Akondi, R. B., & Rao, S. R. (2009). Cardioprotective actions of two bioflavonoids, quercetin and rutin, in experimental myocardial infarction in both normal and streptozotocin-induced type I diabetic rats. Journal of Pharmacy and Pharmacology, 61(10), 1365–1374.
Ammar, E. S. M., Said, S. A., El-Damarawy, S. L., & Suddek, G. M. (2013). Cardioprotective effect of grape-seed proanthocyanidins on doxorubicin-induced cardiac toxicity in rats. Pharmaceutical Biology, 51(3), 339–344.
Momin, F. N., Kalai, B. R., Shikalgar, T. S., & Naikwade, N. S. (2012). Cardioprotective effect of methanolic extract of Ixora coccinea Linn. leaves on doxorubicin-induced cardiac toxicity in rats. Indian Journal of Pharmacology, 44(2), 178–183.
Sandamali, J. A., Hewawasam, R. P., Jayatilaka, K. A., & Mudduwa, L. K. (2020). Cardioprotective potential of Murraya koenigii (L.) Spreng. leaf extract against doxorubicin-induced cardiotoxicity in rats. Evidence-Based Complementary and Alternative Medicine, 2020, 6023737.
Khames, A., Khalaf, M. M., Gad, A. M., Abd El-raouf, O. M., & Kandeil, M. A. (2019). Nicorandil combats doxorubicin–induced nephrotoxicity via amendment of TLR4/P38 MAPK/NFκ-B signaling pathway. Chemico-Biological Interactions, 311, 108777.
Dudka, J., Gieroba, R., Korga, A., Burdan, F., Matysiak, W., Jodlowska-Jedrych, B., & Murias, M. (2012). Different effects of resveratrol on dose-related doxorubicin-induced heart and liver toxicity. Evidence-Based Complementary and Alternative Medicine, 2012, 10 .
Quagliariello, V., Vecchione, R., Coppola, C., Di Cicco, C., De Capua, A., Piscopo, G., & Maurea, N. (2018). Cardioprotective effects of nanoemulsions loaded with anti-inflammatory nutraceuticals against doxorubicin-induced cardiotoxicity. Nutrients, 10(9), 1304.
Wu, R., Mei, X., Wang, J., Sun, W., Xue, T., Lin, C., & Xu, D. (2019). Zn (ii)-Curcumin supplementation alleviates gut dysbiosis and zinc dyshomeostasis during doxorubicin-induced cardiotoxicity in rats. Food & Function, 10(9), 5587–5604.
Baiyun, R., Li, S., Liu, B., Lu, J., Lv, Y., Xu, J., & Zhang, Z. (2018). Luteolin-mediated PI3K/AKT/Nrf2 signaling pathway ameliorates inorganic mercury-induced cardiac injury. Ecotoxicology and Environmental Safety, 161, 655–661.
Arunachalam, S., Nagoor Meeran, M. F., Azimullah, S., Sharma, C., Goyal, S. N., & Ojha, S. (2021). Nerolidol attenuates oxidative stress, inflammation, and apoptosis by modulating Nrf2/MAPK signaling pathways in doxorubicin-induced acute cardiotoxicity in rats. Antioxidants, 10(6), 984.
Germoush, M. O. (2016). Diosmin protects against cyclophosphamide-induced liver injury through attenuation of oxidative stress, inflammation and apoptosis. International Journal of Pharmacology, 12(6), 644–654.
Ali, N., AlAsmari, A. F., Imam, F., Ahmed, M. Z., Alqahtani, F., Alharbi, M., & Alanazi, M. M. (2021). Protective effect of diosmin against doxorubicin-induced nephrotoxicity. Saudi Journal of Biological Sciences, 28(8), 4375–4383.
Queenthy, S. S., & John, B. (2013). Diosmin exhibits anti-hyperlipidemic effects in isoproterenol induced myocardial infarcted rats. European Journal of Pharmacology, 718(1-3), 213–218.
Elblehi, S. S., El-Sayed, Y. S., Soliman, M. M., & Shukry, M. (2021). Date palm pollen extract avert doxorubicin-induced cardiomyopathy fibrosis and associated oxidative/ nitrosative stress, inflammatory cascade, and apoptosis-targeting Bax/Bcl-2 and Caspase-3 signaling pathways. Animals, 11, 886.
Bai, Z., & Wang, Z. (2019). Genistein protects against doxorubicin‐induced cardiotoxicity through Nrf‐2/HO‐1 signaling in mice model. Environmental Toxicology, 34(5), 645–651.
Alanazi, A. M., Fadda, L., Alhusaini, A., Ahmad, R., Hasan, I. H., & Mahmoud, A. M. (2020). Liposomal resveratrol and/or carvedilol attenuate doxorubicin-induced cardiotoxicity by modulating inflammation, oxidative stress and S100A1 in rats. Antioxidants, 9(2), 159.
Hafez, H. M., & Hassanein, H. (2022). Montelukast ameliorates doxorubicin-induced cardiotoxicity via modulation of p-glycoprotein and inhibition of ROS-mediated TNF-α/NF-κB pathways. Drug and Chemical Toxicology, 45(2), 548–559.
Hu, C., Zhang, X., Zhang, N., Wei, W. Y., Li, L. L., Ma, Z. G., & Tang, Q. Z. (2020). Osteocrin attenuates inflammation, oxidative stress, apoptosis, and cardiac dysfunction in doxorubicin‐induced cardiotoxicity. Clinical and Translational Medicine, 10(3), e124.
Bin Jardan, Y. A., Ansari, M. A., Raish, M., Alkharfy, K. M., Ahad, A., Al-Jenoobi, F. I., & Ahmad, A. (2020). Sinapic acid ameliorates oxidative stress, inflammation, and apoptosis in acute doxorubicin-induced cardiotoxicity via the NF-κB-mediated pathway. BioMed Research International, 2020, 3921796.
Elsherbiny, N. M., & El-Sherbiny, M. (2014). Thymoquinone attenuates Doxorubicin-induced nephrotoxicity in rats: Role of Nrf2 and NOX4. Chemico-Biological Interactions, 223, 102–108.
Rashid, M. I., Fareed, M. I., Rashid, H., Aziz, H., Ehsan, N., Khalid, S., & Hakeem, K. R. (2017). Flavonoids and their biological secrets. Plant and Human Health: Phytochemistry and Molecular Aspects, 2, 579–605.
Wali, A. F., Rashid, S., Rashid, S. M., Ansari, M. A., Khan, M. R., Haq, N., Alhareth, D. Y., Ahmad, A., & Rehman, M. U. (2020). Naringenin regulates doxorubicin-induced liver dysfunction: Impact on oxidative stress and inflammation. Plants, 9, 550.
Ahmed, S., Mundhe, N., Borgohain, M., Chowdhury, L., Kwatra, M., Bolshette, N., & Lahkar, M. (2016). Diosmin modulates the NF-kB signal transduction pathways and downregulation of various oxidative stress markers in alloxan-induced diabetic nephropathy. Inflammation, 39, 1783–1797.
Eisvand, F., Imenshahidi, M., Ghasemzadeh Rahbardar, M., Tabatabaei Yazdi, S. A., Rameshrad, M., Razavi, B. M., & Hosseinzadeh, H. (2022). Cardioprotective effects of alpha‐mangostin on doxorubicin‐induced cardiotoxicity in rats. Phytotherapy Research, 36(1), 506–524.
Kim, Y. I., Park, S. W., Kang, I. J., Shin, M. K., & Lee, M. H. (2015). Activin suppresses LPS-induced Toll-like receptor, cytokine and inducible nitric oxide synthase expression in normal human melanocytes by inhibiting NF-κB and MAPK pathway activation. International Journal of Molecular Medicine, 36(4), 1165–1172.
Xiao, Q., Qu, Z., Zhao, Y., Yang, L., & Gao, P. (2017). Orientin ameliorates LPS-induced inflammatory responses through the inhibitory of the NF-κB pathway and NLRP3 inflammasome. Evidence-Based Complementary and Alternative Medicine, 2017, 2495496.
Kerkelä, R., Ilves, M., Pikkarainen, S., Tokola, H., Ronkainen, V. P., Majalahti, T., & Ruskoaho, H. (2011). Key roles of endothelin-1 and p38 MAPK in the regulation of atrial stretch response. American Journal of Physiology-Regulatory, Integrative and Comparative Physiology, 300(1), R140–R149.
Oeckinghaus, A., & Ghosh, S. (2009). The NF-κB family of transcription factors and its regulation. Cold Spring Harbor Perspectives in Biology, 1(4), a000034.
Imam, F., Al-Harbi, N. O., Al-Harbi, M. M., Ansari, M. A., Al-Asmari, A. F., Ansari, M. N., & Alotaibi, M. R. (2018). Apremilast prevent doxorubicin-induced apoptosis and inflammation in heart through inhibition of oxidative stress mediated activation of NF-κB signaling pathways. Pharmacological Reports, 70, 993–1000.
Tahir, M., Rehman, M. U., Lateef, A., Khan, R., Khan, A. Q., Qamar, W., & Sultana, S. (2013). Diosmin protects against ethanol-induced hepatic injury via alleviation of inflammation and regulation of TNF-α and NF-κB activation. Alcohol, 47(2), 131–139.
Ichihara, S., Ichihara, G., Kawai, Y., Osawa, T., & Yamada, Y. (2006). Regulatory role of hypoxia-inducible factor-1α and redox-regulated transcription factor in doxorubicin cardiotoxicity. Circulation, 114, 414–415.
van Uden, P., Kenneth, N. S., & Rocha, S. (2008). Regulation of hypoxia-inducible factor-1α by NF-κB. Biochemical Journal, 412(3), 477–484.
Ibrahim, K. M., Mantawy, E. M., Elanany, M. M., Abdelgawad, H. S., Khalifa, N. M., Hussien, R. H., & El-Demerdash, E. (2020). Protection from doxorubicin-induced nephrotoxicity by clindamycin: Novel antioxidant, anti-inflammatory and anti-apoptotic roles. Naunyn-Schmiedeberg’s Archives of Pharmacology, 393, 739–748.
Li, L. L., Wei, L., Zhang, N., Wei, W. Y., Hu, C., Deng, W., & Tang, Q. Z. (2020). Levosimendan protects against doxorubicin-induced cardiotoxicity by regulating the PTEN/Akt pathway. BioMed Research International, 2020, 11.
Radhiga, T., Rajamanickam, C., Sundaresan, A., Ezhumalai, M., & Pugalendi, K. V. (2012). Effect of ursolic acid treatment on apoptosis and DNA damage in isoproterenol-induced myocardial infarction. Biochimie, 94, 1135–1142.
Su, Z., Ye, J., Qin, Z., & Ding, X. (2015). Protective effects of madecassoside against doxorubicin induced nephrotoxicity in vivo and in vitro. Scientific Reports, 5(1), 18314.
Mobaraki, M., Faraji, A., Zare, M., Dolati, P., Ataei, M., & Manshadi, H. D. (2017). Molecular mechanisms of cardiotoxicity: A review on major side-effect of doxorubicin. Indian Journal of Pharmaceutical Sciences, 79(3), 335–344.
Abdel Aziz, M. T., Wassef, M. A. A., Ahmed, H. H., Rashed, L., Mahfouz, S., Aly, M. I., & Abdelaziz, M. (2014). The role of bone marrow derived-mesenchymal stem cells in attenuation of kidney function in rats with diabetic nephropathy. Diabetology & Metabolic Syndrome, 6, 1–10.
Thangarajan, S., Ramachandran, S., & Krishnamurthy, P. (2016). Chrysin exerts neuroprotective effects against 3-Nitropropionic acid induced behavioral despair—Mitochondrial dysfunction and striatal apoptosis via upregulating Bcl-2 gene and downregulating Bax—Bad genes in male wistar rats. Biomedicine & Pharmacotherapy, 84, 514–525.
Yang, Z., Zhang, X. R., Zhao, Q., Wang, S. L., Xiong, L. L., Zhang, P., Wang, T. H., & Zhang, Y. H. (2018). Knockdown of TNF-α alleviates acute lung injury in rats with intestinal ischemia and reperfusion injury by upregulating IL-10 expression. International Journal of Molecular Medicine, 42(2), 926–934.
Yu, X., Lu, C., Liu, H., Rao, S., Cai, J., Liu, S., & Ding, X. (2013). Hypoxic preconditioning with cobalt of bone marrow mesenchymal stem cells improves cell migration and enhances therapy for treatment of ischemic acute kidney injury. PLoS ONE, 8(5), e62703.
Wu, X. H., Liu, C. P., Xu, K. F., Mao, X. D., Zhu, J., Jiang, J. J., & Liu, C. (2007). Reversal of hyperglycemia in diabetic rats by portal vein transplantation of islet-like cells generated from bone marrow mesenchymal stem cells. World Journal of Gastroenterology, 13(24), 3342.
Author information
Authors and Affiliations
Contributions
Rehab S. Abohashem conceived and designed the idea, performed the in vivo study and participated in the biochemical and data analysis, and wrote the manuscript. Hanaa H. Ahmed conceived and designed the idea, revised the manuscript, and provided the administrative support. Alaa H. Sayed participated in the biochemical and data analysis. Heba Effat performed the in vitro study and molecular genetic analysis, participated in data analysis and writing the manuscript. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Ethical Approval
The experimental protocol was conducted in compliance with the National Institute of Health guidelines and with the approval of Institutional Ethical Committee for Medical Research, National Research Centre, Egypt (Code No. 62311122022).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abohashem, R.S., Ahmed, H.H., Sayed, A.H. et al. Primary Protection of Diosmin Against Doxorubicin Cardiotoxicity via Inhibiting Oxido-Inflammatory Stress and Apoptosis in Rats. Cell Biochem Biophys (2024). https://doi.org/10.1007/s12013-024-01289-7
Accepted:
Published:
DOI: https://doi.org/10.1007/s12013-024-01289-7