Abstract
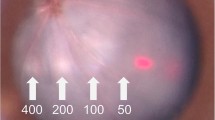
Many clinical trials have demonstrated the effectiveness of subthreshold phototherapy with no visible damage in retinal vascular diseases, such as diabetic retinopathy. We aimed primarily to investigate the effect of subthreshold diode micropulse laser (SDM) treatment on mouse retinal pigmented epithelium (RPE) cells. The expression of angiogenesis-modulating cytokines in response to SDM was also explored. The least toxic laser dose was selected by measuring cell viability with MTT assay and 5 % duty cycle (DC) was chosen for use in further experiments. RPE cells were treated with laser-induced radiation ranging from 0 to 400 mW for 24 h. The apoptotic rate of RPE cells was assessed by flow cytometry. Expressions of vascular endothelial growth factor A (VEGF-A), transforming growth factor beta (TGF-β), basic fibroblast growth factor (bFGF), and pigment epithelium-derived factor (PEDF) were determined by Western Blotting and real-time PCR, respectively. After 24 h of laser irradiation, cell viability was reduced dose dependently and the effect was significant compared to the controls (P < 0.05). In addition, laser treatment with intensities of 100 and 200 mW with DC of 5 % produced no significant effect on cell viability and apoptosis as compared with the control group (P > 0.05). The protein and mRNA expressions of angiogenic stimulators (VEGF-A, TGF-β, and bFGF) were significantly down-regulated (P < 0.05), whereas those of the angiogenic inhibitor (PEDF) were up-regulated (P < 0.05). No significant difference was found between the cells treated with different intensities of laser radiation (P > 0.05). Our results showed that SDM treatment of the RPE cells suppressed the expression of choroid neovasculization-promoting cytokines and up-regulated the angiogenic inhibitor, PEDF without damaging the cells. Further investigation is needed to understand the mechanism and to optimize the use of SDM as a novel method of treatment for retinal vascular diseases.





Similar content being viewed by others
References
Kiire, C., Sivaprasad, S., & Chong, V. (2011). Subthreshold micropulse laser therapy for retinal disorders. Retina Today, 1, 67–70.
Mainster, M. A. (1999). Decreasing retinal photocoagulation damage: Principles and techniques. Seminars in Ophthalmology, 14(4), 200–209.
Ferrara, N., Gerber, H. P., & LeCouter, J. (2003). The biology of VEGF and its receptors. Nature Medicine, 9, 669–676.
King, G. L., & Suzuma, K. (2000). Pigment-epithelium-derived factor—A key coordinator of retinal neuronal and vascular functions. New England Journal of Medicine, 342, 349–351.
The Diabetes Control and Complications Trial Research Group. (1993). The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. New England Journal of Medicine, 329, 977–986.
Shah, A. M., Bressler, N. M., & Jampol, L. M. (2011). Does laser still have a role in the management of retinal vascular and neovascular diseases? American Journal of Ophthalmology, 152, 332–339.
Schatz, H., Madeira, D., McDonald, H. R., & Johnson, R. N. (1991). Progressive enlargement of laser scars following grid laser photocoagulation for diffuse diabetic macular edema. Archives of Ophthalmology, 109, 1549–1551.
Early Treatment Diabetic Retinopathy Study Research Group. (1995). Focal photocoagulation treatment of diabetic macular edema. Relationship of treatment effect to fluorescein angiographic and other retinal characteristics at baseline: ETDRS report no. 19. Archives of Ophthalmology, 113, 1144–1155.
Luttrull, J. K., Sramek, C., Palanker, D., Spink, C. J., & Musch, D. C. (2012). Long-term safety, high-resolution imaging, and tissue temperature modeling of subvisible diode micropulse photocoagulation for retinovascular macular edema. Retina, 32, 375–386.
Ohkoshi, K., & Yamaguchi, T. (2010). Subthreshold micropulse diode laser photocoagulation for diabetic macular edema in Japanese patients. American Journal of Ophthalmology, 149, 133–139.
Figueira, J., Khan, J., Nunes, S., Sivaprasad, S., Rosa, A., et al. (2009). Prospective randomised controlled trial comparing sub-threshold micropulse diode laser photocoagulation and conventional green laser for clinically significant diabetic macular oedema. British Journal of Ophthalmology, 93, 1341–1344.
Gao, X., & Xing, D. (2009). Molecular mechanisms of cell proliferation induced by low power laser irradiation. Journal of Biomedical Science, 16, 4.
Vujosevic, S., Bottega, E., Casciano, M., et al. (2010). Microperimetry and fundus autofluorescence in diabetic macular edema: subthreshold micropulse diode laser versus modified early treatment diabetic retinopathy study laser photocoagulation. Retina., 30(6), 908–916.
Laursen, M. L., Moeller, F., Sander, B., & Sjoelie, A. K. (2004). Subthreshold micropulse diode laser treatment in diabetic macular oedema. British Journal of Ophthalmology, 88, 1173–1179.
Dorin, G. (2004). Evolution of retinal laser therapy: minimum intensity photocoagulation (MIP). Can the laser heal the retina without harming it? Seminars in Ophthalmology, 19, 62–68.
Luttrull, J. K., Musch, D. C., & Mainster, M. A. (2005). Subthreshold diode micropulse photocoagulation for the treatment of clinically significant diabetic macular oedema. British Journal of Ophthalmology, 89, 74–80.
Meyer, C. H., & Holz, F. G. (2011). Preclinical aspects of anti-VEGF agents for the treatment of wet AMD: Ranibizumab and bevacizumab. Eye (London), 25, 661–672.
Schatz, H., Madeira, D., McDonald, H. R., & Johnson, R. N. (1991). Progressive enlargement of laser scars following grid laser photocoagulation for diffuse diabetic macular edema. Archives of Ophthalmology, 109, 1549–1551.
Akrami, H., Soheili, Z.-S., Khalooghi, K., Ahmadieh, H., Rezaie-Kanavi, M., Samiei, S., et al. (2009). Retinal pigment epithelium culture; a potential source of retinal stem cells. Journal of Ophthalmic & Vision Research, 4(3), 134–141.
Dorin, G. (2003). Subthreshold and micropulse diode laser photocoagulation. Seminars in Ophthalmology, 18, 147–153.
Ohno-Matsui, K., Morita, I., Tombran-Tink, J., Mrazek, D., Onodera, M., et al. (2001). Novel mechanism for age-related macular degeneration: An equilibrium shift between the angiogenesis factors VEGF and PEDF. Journal of Cellular Physiology, 189, 323–333.
Sohn, H. J., Han, D. H., Kim, I. T., Oh, I. K., Kim, K. H., et al. (2011). Changes in aqueous concentrations of various cytokines after intravitreal triamcinolone versus bevacizumab for diabetic macular edema. American Journal of Ophthalmology, 152, 686–694.
Hogan, M. J., Alvarado, J. A., & Weddell, J. E. (1971). The retinal pigment epithelium. In M. J. Hogan, J. A. Alvarado, & J. E. Weddell (Eds.), Histology of the human eye (pp. 405–423). Philadelphia: W.B. Saunders.
Marmor, M. F. (1998). Structure, function, and disease of the retinal pigment epithelium. In M. F. Marmor & T. J. Wolfenberger (Eds.), The retinal pigment epithelium (pp. 3–12). New York: Oxford Press.
Folkman, J. (1995). Angiogenesis in cancer, vascular, rheumatoid, and other diseases. Nature Medicine, 1, 27–31.
Tatar, O., Kaiserling, E., Adam, A., Gelisken, F., Shinoda, K., et al. (2006). Consequences of verteporfin photodynamic therapy on choroidal neovascular membranes. Archives of Ophthalmology, 124, 815–823.
Chapman, J. A., & Beckey, C. (2006). Pegaptanib: A novel approach to ocular neovascularization. Annals of Pharmacotherapy, 40, 1322–1326.
Frank, R. N., Amin, R. H., Eliott, D., Puklin, J. E., & Abrams, G. W. (1996). Basic fibroblast growth factor and vascular endothelial growth factor are present in epiretinal and choroidal neovascular membranes. American Journal of Ophthalmology, 122, 393–403.
Matsuda, S., Gomi, F., Oshima, Y., Tohyama, M., & Tano, Y. (2005). Vascular endothelial growth factor reduced and connective tissue growth factor induced by triamcinolone in ARPE19 cells under oxidative stress. Investigative Ophthalmology & Visual Science, 46, 1062–1068.
Okamoto, N., Tobe, T., Hackett, S. F., Ozaki, H., Vinores, M. A., LaRochelle, W., et al. (1997). Transgenic mice with increased expression of vascular endothelial growth factor in the retina. A new model of intraretinal and subretinal neovascularization. American Journal of Pathology, 151, 281–291.
Dawson, D. W., Volpert, O. V., Gillis, P., Crawford, S. E., Xu, H., et al. (1999). Pigment epithelium-derived factor: A potent inhibitor of angiogenesis. Science, 285, 245–248.
Ogata, N., Wada, M., Otsuji, T., Jo, N., Tombran-Tink, J., et al. (2002). Expression of pigment epithelium-derived factor in normal adult rat eye and experimental choroidal neovascularization. Investigative Ophthalmology & Visual Science, 43, 1168–1175.
Bhutto, I. A., McLeod, D. S., Hasegawa, T., Kim, S. Y., Merges, C., et al. (2006). Pigment epithelium-derived factor (PEDF) and vascular endothelial growth factor (VEGF) in aged human choroid and eyes with age-related macular degeneration. Experimental Eye Research, 82, 99–110.
Kliffen, M., Sharma, H. S., Mooy, C. M., Kerkvliet, S., & de Jong, P. T. (1997). Increased expression of angiogenic growth factors in age-related maculopathy. British Journal of Ophthalmology, 81, 154–162.
Pertovaara, L., Kaipainen, A., Mustonen, T., Orpana, A., Ferrara, N., Saksela, O., et al. (1994). Vascular endothelial growth factor is induced in response to transforming growth factor-beta in fibroblastic and epithelial cells. Journal of Biological Chemistry, 269, 6271–6274.
Renno, R. Z., Youssri, A. I., Michaud, N., Gragoudas, E. S., & Miller, J. W. (2002). Expression of pigment epithelium–derived factor in experimental choroidal neovascularisation. Investigative Ophthalmology & Visual Science, 43, 1574–1580.
Flaxel, C., Bradle, J., Acott, T., & Samples, J. R. (2007). Retinal pigment epithelium produces matrix metalloproteinases after laser treatment. Retina, 27, 629–634.
Matsumoto, Miho., Yoshimura, Nagahisa., & Honda, Yoshihito. (1994). Increased production of transforming growth factor-β2 from cultured human retinal pigment epithelial cells by photocoagulation. Investigative Ophthalmology & Visual Science, 35, 4245–4252.
Acknowledgments
This work was generously supported by grants from the National Natural Science Foundation of China (Nos. 61378084).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, Z., Song, Y., Chen, X. et al. Biological Modulation of Mouse RPE Cells in Response to Subthreshold Diode Micropulse Laser Treatment. Cell Biochem Biophys 73, 545–552 (2015). https://doi.org/10.1007/s12013-015-0675-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12013-015-0675-8