Abstract
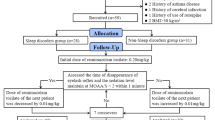
Insomnia, defined as difficulty in falling asleep and/or staying asleep, short sleep duration, or poor quality sleep, is a common sleep disorder affecting 30–40% of adult population. We have conducted a randomized, double-blind, placebo-controlled study to test if anesthesia is therapeutically beneficial in patients with refractory chronic primary insomnia. We have assessed the efficacy and safety of propofol-induced sleep in these patients. This study comprised of 103 patients with refractory chronic primary insomnia (including 59 non-pregnant, non-lactating women; 28–60 years) and the participants were randomized to receive either physiological saline (placebo) (n = 39) or 3.0 g/l propofol (n = 64) in a 2-h continuous intravenous infusion for five consecutive nights. The Leeds Sleep Evaluation Questionnaire was used for the subjective assessment of sleep, and polysomnography was used for the objective measurement of sleep architecture and patterns. The assessments were done prior to and at the end of the 5-day treatment and 6 months after treatment period. The adverse effects of the treatment were also recorded. A 2-h continuous intravenous infusion of 3.0 g/l propofol for five consecutive nights improved the subjective and objective assessments of sleep in 64 patients with refractory chronic primary insomnia. This improvement occurred immediately after the therapy and persisted for 6 months. No serious adverse events were noticed during the period of drug administration or 6 months after the treatment. Propofol therapy is an efficacious and safe choice for restoring normal sleep in patients with refractory chronic primary insomnia.
Similar content being viewed by others
References
Ramakrishnan, K., & Scheid, D. C. (2007). Treatment options for insomnia. American Family Physician, 76, 517–526.
Kuppermann, M., Lubeck, D. P., Mazonson, P. D., Patrick, D. L., Stewart, A. L., et al. (1995). Sleep problems and their correlates in a working population. Journal of General Internal Medicine, 10, 25–32.
Eaker, E. D., Pinsky, J., & Castelli, W. P. (1992). Myocardial infarction and coronary death among women: Psychosocial predictors from a 20-year follow-up of women in the Framingham Study. American Journal of Epidemiology, 135, 854–864.
Leineweber, C., Kecklund, G., Janszky, I., Akerstedt, T., & Orth-Gomer, K. (2003). Poor sleep increases the prospective risk for recurrent events in middle-aged women with coronary disease. The Stockholm Female Coronary Risk Study. Journal of Psychosomatic Research, 54, 121–127.
Ayas, N. T., White, D. P., Manson, J. E., Stampfer, M. J., Speizer, F. E., et al. (2003). A prospective study of sleep duration and coronary heart disease in women. Archives of Internal Medicine, 163, 205–209.
Irwin, M., Clark, C., Kennedy, B., Christian Gillin, J., & Ziegler, M. (2003). Nocturnal catecholamines and immune function in insomniacs, depressed patients, and control subjects. Brain, Behavior, and Immunity, 17, 365–372.
Savard, J., Laroche, L., Simard, S., Ivers, H., & Morin, C. M. (2003). Chronic insomnia and immune functioning. Psychosomatic Medicine, 65, 211–221.
Morin, A. K. (2006). Strategies for treating chronic insomnia. American Journal of Managed Care, 12, S230–S245.
Lydic, R., & Biebuyck, J. F. (1994). Sleep neurobiology: Relevance for mechanistic studies of anaesthesia. British Journal of Anaesthesia, 72, 506–508.
Alkire, M. T., Pomfrett, C. J., Haier, R. J., Gianzero, M. V., Chan, C. M., et al. (1999). Functional brain imaging during anesthesia in humans: Effects of halothane on global and regional cerebral glucose metabolism. Anesthesiology, 90, 701–709.
Tung, A., Szafran, M. J., Bluhm, B., & Mendelson, W. B. (2002). Sleep deprivation potentiates the onset and duration of loss of righting reflex induced by propofol and isoflurane. Anesthesiology, 97, 906–911.
Nelson, L. E., Lu, J., Guo, T., Saper, C. B., Franks, N. P., et al. (2003). The alpha2-adrenoceptor agonist dexmedetomidine converges on an endogenous sleep-promoting pathway to exert its sedative effects. Anesthesiology, 98, 428–436.
Ito, H., Watanabe, Y., Isshiki, A., & Uchino, H. (1999). Neuroprotective properties of propofol and midazolam, but not pentobarbital, on neuronal damage induced by forebrain ischemia, based on the GABAA receptors. Acta Anaesthesiologica Scandinavica, 43, 153–162.
Kakehata, J., Togashi, H., Yamaguchi, T., Morimoto, Y., & Yoshioka, M. (2007). Effects of propofol and halothane on long-term potentiation in the rat hippocampus after transient cerebral ischaemia. European Journal of Anaesthesiology, 24, 1021–1027.
Nakahata, K., Kinoshita, H., Azma, T., Matsuda, N., Hama-Tomioka, K., et al. (2008). Propofol restores brain microvascular function impaired by high glucose via the decrease in oxidative stress. Anesthesiology, 108, 269–275.
Tung, A., Bergmann, B. M., Herrera, S., Cao, D., & Mendelson, W. B. (2004). Recovery from sleep deprivation occurs during propofol anesthesia. Anesthesiology, 100, 1419–1426.
Jiang, X., Li, W., Li, X., Hu, Y., & Zhang, Y. (2009). Effects of anesthesia on treatment of patients with chronic primary insomnia. 23rd Annual Meeting of the Associated Professional Sleep Societies, LLC (pp. A276–A277). Seattle, Washington: Sleep.
Daskalopoulos, R., Korcok, J., Farhangkhgoee, P., Karmazyn, M., Gelb, A. W., et al. (2001). Propofol protection of sodium-hydrogen exchange activity sustains glutamate uptake during oxidative stress. Anesthesia and Analgesia, 93, 1199–1204.
Acknowledgments
The authors wish to thank the volunteer work of the physicians in the out-patient Department of the Departments of Neurology and Anesthesia, Daping Hospital. The study was supported by a grant from the Foundation of Chongqing.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Xu, Z., Jiang, X., Li, W. et al. Propofol-Induced Sleep: Efficacy and Safety in Patients with Refractory Chronic Primary Insomnia. Cell Biochem Biophys 60, 161–166 (2011). https://doi.org/10.1007/s12013-010-9135-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12013-010-9135-7