Abstract
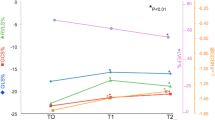
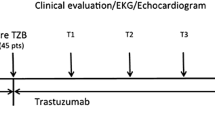
In a previous study of breast cancer patients, we found changes in cardiac function and size during the early stages of adjuvant trastuzumab (Herceptin®) therapy. Here we present a subgroup analysis of this patient cohort. This subgroup received a anthracycline-embedded chemotherapy followed by at least 3 months up to 6 months of adjuvant Herceptin® therapy. Twenty-seven female breast cancer patients with Her-2/-neu overexpression were studied using conventional echocardiography and 2D speckle tracking. These methods were done before anthracycline-embedded chemotherapy, before adjuvant trastuzumab therapy, and both 3 and 6 months after the start of the therapy (T3, T6). The LV–EF (Simpson biplane) decreased significantly from before the chemotherapy to after the chemotherapy and further decreased after 3 months of trastuzumab therapy (66.2 ± 1.5 vs. 58.7 ± 1.2 vs. 55.6 ± 1.3 vs. 55.9 ± 1.5 %; p < 0.05). The stroke volume index remained constant after chemotherapy (22.0 ± 0.8 vs. 22.6 ± 1.3 ml/m2; p = 0.9), but increased significantly during trastuzumab therapy (26.7 ± 1.1 and 27.3 ± 1.0 ml/m2; p < 0.01). Global longitudinal strain exclusively decreased during chemotherapy (−21.0 ± 0.5 vs. −18.9 ± 0.5 %, p < 0.001). Regional longitudinal strain decreased significantly after chemotherapy in septal, anteroseptal, anterolateral, and apex segments. Mitral valve regurgitation increased during the whole treatment, but especially during trastuzumab. Right ventricular function decreased exclusively during chemotherapy. Anthracycline-embedded chemotherapy in patients with breast cancer led to a decrease in LV function, especially of the septal and anterior segments, and did not worsen during adjuvant trastuzumab treatment.













Similar content being viewed by others
Abbreviations
- A′:
-
Late annular velocity
- AR:
-
Atrial reversal
- A :
-
Late diastolic velocity
- C :
-
Anthracycline-embedded chemotherapy
- CI:
-
Confidence interval (25/75 %)
- 2D-STE:
-
Two-dimensional speckle tracking echocardiography
- Doc:
-
Docetaxel
- DT:
-
Deceleration time
- EC:
-
Epirubicin–cyclophosphamide
- EC/TX/CAP:
-
Epirubicin–cyclophosphamide/paclitaxel/capecitabine
- EF:
-
Ejection fraction
- ERO:
-
Effective Regurgitate Orifice area
- ETC:
-
Epirubicin–paclitaxel–cyclophosphamide
- E′:
-
Early annular velocity
- E :
-
Early diastolic velocity
- FEC:
-
5-Fluorouracil–epirubicin–cyclophosphamide
- FS:
-
Fractional shortening
- GLS:
-
Global longitudinal strain
- IVRT:
-
Iso-volumetric relaxation time
- LA:
-
Left atrium
- LA-VI:
-
Left atrium volume index
- LV:
-
Left ventricle
- LV-DVI:
-
Left ventricle diastolic volume index
- LV-SVI:
-
Left ventricle systolic volume index
- ns.:
-
Non-significant
- nt.:
-
Not tested
- PVD:
-
Pulmonary diastolic flow velocity
- PVS:
-
Pulmonary systolic flow velocity
- RLS:
-
Regional longitudinal strain
- RV:
-
Right ventricle
- RVSP:
-
Right ventricle systolic pressure
- s′ :
-
TDI mitral valve annular systolic motion
- s a :
-
TDI tricuspid annular systolic motion
- SEM:
-
Standard error of mean
- SVI:
-
Stroke volume index
- T :
-
Trastuzumab
- TAC:
-
Docetaxel–doxorubicin–cyclophosphamide
- TAPSE:
-
Tricuspid annular plane systolic excursion
- TDI:
-
Tissue Doppler imaging
References
Seidman, A., Hudis, C., Pierri, M. K. et al. (2002). Cardiac dysfunction in the trastuzumab clinical trials experience. doi:10.1200/JCO.20.5.1215.
Ewer, M. S., Gibbs, H. R., Swafford, J., & Benjamin, R. S. (1999). Cardiotoxicity in patients receiving trastuzumab (Herceptin): Primary toxicity, synergistic or sequential stress, or surveillance artifact? Seminars in Oncology, 26, 96–101.
Keefe, D. L. (2002). Trastuzumab-associated cardiotoxicity. Cancer, 95, 1592–1600. doi:10.1002/cncr.10854.
Lange, S. A., Ebner, B., Astrid, W., et al. (2013). Echocardiography signs of early cardiac impairment in patients with breast cancer and trastuzumab therapy. Clinical Research in Cardiology, 100(1). http://medcontent.metapress.com/index/A65RM03P4874243N.pdf. Accessed December 4, 2013.
Biswas, M., Sudhakar, S., Nanda, N. C., et al. (2013). Two- and three-dimensional speckle tracking echocardiography: Clinical applications and future directions. Echocardiography., 30(1), 88–105. doi:10.1111/echo.12079.
Loibl, S., Conrad, B., Schneeweiss, A., et al. (2009). Pegfilgrastim on day 2 vs. day 4 within the prospective, multi-centered GAIN study: A phase III trial to compare ETC vs. EC-TX and ibandronate vs. observation in patients with node-positive primary breast cancer (GBG 33). Germany.
Cheitlin, M. D., Armstrong, W. F., Aurigemma, G. P., et al. (2003). ACC/AHA/ASE 2003 guideline update for the clinical application of echocardiography: Summary article: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASE Committee to Update the 1997 Guid. Circulation, 108(9), 1146–1162. doi:10.1161/01.CIR.0000073597.57414.A9.
Dujardin, K. S., Enriquez-Sarano, M., Bailey, K. R., Nishimura, R. A., Seward, J. B., & Tajik, A. J. (1997). Grading of mitral regurgitation by quantitative Doppler echocardiography: Calibration by left ventricular angiography in routine clinical practice. Circulation, 96, 3409–3415. doi:10.1161/01.CIR.96.10.3409.
Schiller, N., Shah, P., Crawford, M., et al. (1989). Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. Journal of the American Society of Echocardiography, 2(5), 358–367.
Lang, R. M., Bierig, M., Devereux, R. B., et al. (2006). Recommendations for chamber quantification. European Journal of Echocardiography, 7, 79–108. doi:10.1016/j.euje.2005.12.014.
Khoo, C. W., Krishnamoorthy, S., Lim, H. S., & Lip, G. Y. H. (2011). Assessment of left atrial volume: A focus on echocardiographic methods and clinical implications. Clinical Research in Cardiology, 100, 97–105. doi:10.1007/s00392-010-0222-y.
Hummel, Y. M., Klip, I. J. T., de Jong, R. M., Pieper, P. G., van Veldhuisen, D. J., & Voors, A. A. (2010). Diastolic function measurements and diagnostic consequences: A comparison of pulsed wave- and color-coded tissue Doppler imaging. Clinical Research in Cardiology, 99, 453–458. doi:10.1007/s00392-010-0141-y.
Butz, T., Piper, C., Langer, C., et al. (2010). Diagnostic superiority of a combined assessment of the systolic and early diastolic mitral annular velocities by tissue Doppler imaging for the differentiation of restrictive cardiomyopathy from constrictive pericarditis. Clinical Research in Cardiology, 99(4), 207–215.
Nagueh, S. F., Middleton, K. J., Kopelen, H. A., Zoghbi, W. A., & Quiñones, M. A. (1997). Doppler tissue imaging: A noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. Journal of the American College of Cardiology, 30, 1527–1533. doi:10.1016/S0735-1097(97)00344-6.
Nagueh, S. F., Appleton, C. P., Gillebert, T. C., et al. (2009). Recommendations for the evaluation of left ventricular diastolic function by echocardiography. European Journal of Echocardiography, 10(2), 165–193. doi:10.1093/ejechocard/jep007.
Maurer, M. S., Spevack, D., Burkhoff, D., & Kronzon, I. (2004). Diastolic dysfunction: Can it be diagnosed by Doppler echocardiography? Journal of the American College of Cardiology, 44, 1543–1549. doi:10.1016/j.jacc.2004.07.034.
Paulus, W. J., Tschöpe, C., Sanderson, J. E., et al. (2007). How to diagnose diastolic heart failure: A consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. European Heart Journal, 28(20), 2539–2550. doi:10.1093/eurheartj/ehm037.
Yvorchuk, K. J., Davies, R. A., & Chan, K. L. (1994). Measurement of left ventricular ejection fraction by acoustic quantification and comparison with radionuclide angiography. American Journal of Cardiology, 74, 1052–1056. doi:10.1016/0002-9149(94)90858-3.
Teichholz, L. E., Cohen, M. V., Sonnenblick, E. H., & Gorlin, R. (1974). Study of left ventricular geometry and function by B-scan ultrasonography in patients with and without asynergy. New England Journal of Medicine, 291, 1220–1226. http://www.nejm.org/doi/full/10.1056/NEJM197412052912304. Accessed March 23, 2014.
Cerqueira, M. D., Weissman, N. J., Dilsizian, V., Jacobs, A. K., Kaul, S., Laskey, W. K., … & Verani, M. S.. (2002) Standardized Myocardial Segmentation and Nomenclature for Tomographic Imaging of the Heart: A Statement for Healthcare Professionals From the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association American Heart. Circulation, 105, 539–542.
Meluzín, J., Spinarová, L., Bakala, J., et al. (2001). Pulsed Doppler tissue imaging of the velocity of tricuspid annular systolic motion; A new, rapid, and non-invasive method of evaluating right ventricular systolic function. European Heart Journal, 22, 340–348. doi:10.1053/euhj.2000.2296.
Tei, C., Dujardin, K., Hodge, D., et al. (1996). Doppler echocardiographic index for assessment of global right ventricular function. Journal of the American Society of Echocardiography, 9. http://www2.us.elsevierhealth.com/scripts/om.dll/serve?article=a73680.
Kaul, S., Tei, C., Hopkins, J. M., & Shah, P. M. (1984). Assessment of right ventricular function using two-dimensional echocardiography. American Heart Journal, 107, 526–531. http://www.ncbi.nlm.nih.gov/pubmed/6695697.
Ghio, S., Recusani, F., Klersy, C., et al. (2000). Prognostic usefulness of the tricuspid annular plane systolic excursion in patients with congestive heart failure secondary to idiopathic or ischemic dilated cardiomyopathy. American Journal of Cardiology, 85, 837–842. doi:10.1016/S0002-9149(99)00877-2.
Slamon, D. J., Leyland-Jones, B., Shak, S., et al. (2001). Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. New England Journal Medicine, 344(11), 783–792.
Romond, E. H., Perez, E. A., Bryant, J., et al. (2005). Adjuvant Herceptin-Original NSABP & NCCTG data (Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. New England Journal of Medicine, 353, 1673–1684. doi:10.1056/NEJMoa052122.
Tan-Chiu, E., Yothers, G., Romond, E., et al. (2005). Assessment of cardiac dysfunction in a randomized trial comparing doxorubicin and cyclophosphamide followed by paclitaxel, with or without trastuzumab as adjuvant therapy in node-positive, human epidermal growth factor receptor 2-overexpressing breast can. Journal of Clinical Oncology, 23(31), 7811–7819. doi:10.1200/JCO.2005.02.4091.
Piccart-Gebhart, M. J., Procter, M., Leyland-Jones, B., et al. (2005). Trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer. New England Journal of Medicine, 353, 1659–1672. doi:10.1056/NEJMoa052306.
Goldberg, M. (1986). Cyclophosphamide cardiotoxicity: An analysis of dosing as a risk factor. Blood, 68(5), 1114–1118.
Pai, V., & Nahata, M. (2000). Cardiotoxicity of chemotherapeutic agents: Incidence, treatment and prevention. Drug Safety, 22(4), 263–302.
Braverman, A. C., Antin, J. H., Plappert, M. T., Cook, E. F., & Lee, R. T. (1991). Cyclophosphamide cardiotoxicity in bone marrow transplantation: A prospective evaluation of new dosing regimens. Journal of Clinical Oncology, 9(7), 1215–1223.
Ryberg, M., Nielsen, D., Skovsgaard, T., Hansen, J., Jensen, B. V., & Dombernowsky, P. (1998). Epirubicin cardiotoxicity: An analysis of 469 patients with metastatic breast cancer. Journal of Clinical Oncology, 16(11), 3502–3508.
Swain, S. M., Whaley, F. S., & Ewer, M. S. (2003). Congestive heart failure in patients treated with doxorubicin: A retrospective analysis of three trials. Cancer, 97(11), 2869–2879. doi:10.1002/cncr.11407.
Rowinsky, E. K., McGuire, W. P., Guarnieri, T., Fisherman, J. S., Christian, M. C., & Donehower, R. C. (1991). Cardiac disturbances during the administration of taxol. Journal of Clinical Oncology, 9(9), 1704–1712.
Chan, S., Friedrichs, K., Noel, D., et al. (1999). Prospective randomized trial of docetaxel versus doxorubicin in patients with metastatic breast cancer. Journal of Clinical Oncology, 17(8), 2341–2354.
Robben, N. C., Pippas, A. W., & Moore, J. O. (1993). The syndrome of 5-fluorouracil cardiotoxicity: An elusive cardiopathy. Cancer, 71(2), 493–509. doi:10.1002/1097-0142(19930115)71:2<493:AID-CNCR2820710235>3.0.CO;2-C.
Stewart, T., Pavlakis, N., & Ward, M. (2010). Cardiotoxicity with 5-fluorouracil and capecitabine: More than just vasospastic angina. Internal Medicine Journal, 40(4), 303–307. doi:10.1111/j.1445-5994.2009.02144.x.
Bria, E., Cuppone, F., Fornier, M., et al. (2008). Cardiotoxicity and incidence of brain metastases after adjuvant trastuzumab for early breast cancer: The dark side of the moon? A meta-analysis of the randomized trials. Breast Cancer Research and Treatment, 109(2), 231–239.
Dandel, M., & Hetzer, R. (2009). Echocardiographic strain and strain rate imaging—clinical applications. International Journal of Cardiology, 132(1), 11–24. doi:10.1016/j.ijcard.2008.06.091.
Kang, Y., Xu, X., Cheng, L., Li, L., Sun, M., Chen, H., et al. (2014). Two-dimensional speckle tracking echocardiography combined with high-sensitive cardiac troponin T in early detection and prediction of cardiotoxicity during epirubicine-based chemotherapy. European Journal of Heart Failure, 16(3), 300–308.
Ho, E., Brown, A., Barrett, P., et al. (2010). Subclinical anthracycline- and trastuzumab-induced cardiotoxicity in the long-term follow-up of asymptomatic breast cancer survivors: A speckle tracking echocardiographic study. Heart, 96, 701–707. doi:10.1136/hrt.2009.173997.
Tanindi, A., Demirci, U., Tacoy, G., et al. (2011). Assessment of right ventricular functions during cancer chemotherapy. European Journal of Echocardiography, 12, 834–840. doi:10.1093/ejechocard/jer142.
Belham, M., Kruger, A., & Pritchard, C. (2006). The Tei index identifies a differential effect on left and right ventricular function with low-dose anthracycline chemotherapy. Journal of the American Society of Echocardiography, 19, 206–210. doi:10.1016/j.echo.2005.08.018.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lange, S.A., Jung, J., Jaeck, A. et al. Subclinical Myocardial Impairment Occurred in Septal and Anterior LV Wall Segments After Anthracycline-Embedded Chemotherapy and did not Worsen During Adjuvant Trastuzumab Treatment in Breast Cancer Patients. Cardiovasc Toxicol 16, 193–206 (2016). https://doi.org/10.1007/s12012-015-9328-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12012-015-9328-9