Abstract
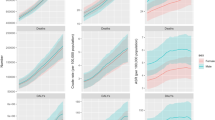
Long-term exposure to lead is associated with an increased risk of diabetic kidney disease (DKD). However, limited data exist on global trends in DKD burden attributable to lead exposure, especially across diverse regions categorized by socioeconomic level. We aimed to assess the spatiotemporal changes in DKD burden attributable to lead exposure from 1990 to 2019 across 204 countries and regions with varying socio-demographic index (SDI) metrics. This retrospective analysis utilized data from the Global Burden of Disease Study 2019 (GBD2019) database. We estimated the burden of DKD attributable to lead exposure using the age-standardized mortality rate (ASMR) and age-standardized disability-adjusted life year rate (ASDR), accounting for sex, age, nationality, and SDI. The annual percentage change (APC) and average annual percentage change (AAPC) were calculated using the Joinpoint model to evaluate trends in the ASMR and ASDR attributable to lead exposure from 1990 to 2019. Gaussian process regression was used to model the relationship between the SDI and ASMR/ASDR. Globally, the burden of DKD attributable to lead exposure has significantly increased since 1990, especially among elderly men and in regions such as Asia, Central Latin America, North Africa, the Middle East, and low-SDI regions. In 2019, the ASMR and ASDR of DKD attributable to lead exposure were 0.68 (95% CI: 0.40, 0.98) per 100,000 people and 15.02 (95% CI: 8.68, 22.26) per 100,000 people, respectively. From 1990 to 2019, the global ASMR and ASDR attributable to lead-associated DKD changed by 15.45% and -1.78%, respectively. The global AAPCs of the ASMR and ASDR were 0.55 (95% CI: 0.45, 0.65) and -0.01 (95% CI: -0.12, 0.1), respectively. Significant declining trends were observed in the high-income Asia Pacific region, eastern sub-Saharan Africa, North Africa, the Middle East, and other regions with high SDIs. Over this 30-year study period, the global burden of DKD attributable to lead exposure has increased, particularly in regions with low SDI. Lead exposure remains a significant concern in the global burden of diabetic kidney disease.





Similar content being viewed by others
Data Availability
No datasets were generated or analysed during the current study.
References
Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW et al (2018) IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract 138:271–281. https://doi.org/10.1016/j.diabres.2018.02.023
Akhtar M, Taha NM, Nauman A, Mujeeb IB, Al-Nabet A (2020) Diabetic Kidney Disease: Past and Present. Adv Anat Pathol 27(2):87–97. https://doi.org/10.1097/PAP.0000000000000257
Afkarian M, Zelnick LR, Hall YN, Heagerty PJ, Tuttle K, Weiss NS et al (2016) Clinical Manifestations of Kidney Disease Among US Adults With Diabetes, 1988-2014. JAMA. 316(6):602–610. https://doi.org/10.1001/jama.2016.10924
Alicic RZ, Rooney MT, Tuttle KR (2017) Diabetic Kidney Disease: Challenges, Progress, and Possibilities. Clin J Am Soc Nephrol 12(12):2032–2045. https://doi.org/10.2215/CJN.11491116
Giorda CB, Carna P, Salomone M, Picariello R, Costa G, Tartaglino B et al (2018) Ten-year comparative analysis of incidence, prognosis, and associated factors for dialysis and renal transplantation in type 1 and type 2 diabetes versus non-diabetes. Acta Diabetol 55(7):733–740. https://doi.org/10.1007/s00592-018-1142-y
Gregg EW, Williams DE, Geiss L (2014) Changes in diabetes-related complications in the United States. N Engl J Med 371(3):286–287. https://doi.org/10.1056/NEJMc1406009
Thomas B (2019) The Global Burden of Diabetic Kidney Disease: Time Trends and Gender Gaps. Curr Diab Rep 19(4):18. https://doi.org/10.1007/s11892-019-1133-6
Apostolou A, Garcia-Esquinas E, Fadrowski JJ, McLain P, Weaver VM, Navas-Acien A (2012) Secondhand tobacco smoke: a source of lead exposure in US children and adolescents. Am J Public Health 102(4):714–722. https://doi.org/10.2105/AJPH.2011.300161
Rehman K, Fatima F, Waheed I, Akash MSH (2018) Prevalence of exposure of heavy metals and their impact on health consequences. J Cell Biochem 119(1):157–184. https://doi.org/10.1002/jcb.26234
Satarug S, G CG, D AV, Phelps KR. (2020) Cadmium and lead exposure, nephrotoxicity, and mortality. Toxics. 8(4). https://doi.org/10.3390/toxics8040086
Tong S, Von Schirnding YE, Prapamontol T (2000) Environmental lead exposure: a public health problem with global dimensions. Servir. 49(1):35–43
Madden EF, Fowler BA (2000) Mechanisms of nephrotoxicity from metal combinations: a review. Drug Chem Toxicol 23(1):1–12. https://doi.org/10.1081/dct-100100098
Hagedoorn IJM, Gant CM, Huizen SV, Maatman R, Navis G, Bakker SJL et al (2020) Lifestyle-Related Exposure to Cadmium and Lead is Associated with Diabetic Kidney Disease. J Clin Med 9(8). https://doi.org/10.3390/jcm9082432
Diseases GBD, Injuries C (2020) Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 396(10258):1204–1222. https://doi.org/10.1016/S0140-6736(20)30925-9
Collaborators GBDCRF (2022) The global burden of cancer attributable to risk factors, 2010-19: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 400(10352):563–591. https://doi.org/10.1016/S0140-6736(22)01438-6
Sang S, Chu C, Zhang T, Chen H, Yang X (2022) The global burden of disease attributable to ambient fine particulate matter in 204 countries and territories, 1990-2019: A systematic analysis of the Global Burden of Disease Study 2019. Ecotoxicol Environ Saf 238:113588. https://doi.org/10.1016/j.ecoenv.2022.113588
Yang X, Chen H, Zhang T, Yin X, Man J, He Q et al (2021) Global, regional, and national burden of blindness and vision loss due to common eye diseases along with its attributable risk factors from 1990 to 2019: a systematic analysis from the global burden of disease study 2019. Aging (Albany NY) 13(15):19614–19642. https://doi.org/10.18632/aging.203374
Collaborators GBDCoD (2018) Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 392(10159):1736–1788. https://doi.org/10.1016/S0140-6736(18)32203-7
Mattiuzzi C, Lippi G (2020) Recent updates on worldwide gout epidemiology. Clin Rheumatol 39(4):1061–1063. https://doi.org/10.1007/s10067-019-04868-9
Liu C, Wang B, Liu S, Li S, Zhang K, Luo B et al (2021) Type 2 diabetes attributable to PM(2.5): A global burden study from 1990 to 2019. Environ Int 156:106725. https://doi.org/10.1016/j.envint.2021.106725
Tapper EB, Parikh ND (2018) Mortality due to cirrhosis and liver cancer in the United States, 1999-2016: observational study. BMJ. 362:k2817. https://doi.org/10.1136/bmj.k2817
Mehdipour P, Navidi I, Parsaeian M, Mohammadi Y, Moradi Lakeh M, Rezaei Darzi E et al (2014) Application of Gaussian Process Regression (GPR) in estimating under-five mortality levels and trends in Iran 1990 - 2013, study protocol. Arch Iran Med 17(3):189–192
Farmand F, Ehdaie A, Roberts CK, Sindhu RK (2005) Lead-induced dysregulation of superoxide dismutases, catalase, glutathione peroxidase, and guanylate cyclase. Environ Res 98(1):33–39. https://doi.org/10.1016/j.envres.2004.05.016
Gui C, Shan X, Liu C, He L, Zhao H, Luo B (2023) Disease burden of chronic kidney disease attributable to lead exposure: A global analysis of 30 years since 1990. Chemosphere. 341:140029. https://doi.org/10.1016/j.chemosphere.2023.140029
Ahmadian E, Eftekhari A, Atakishizada S, Valiyeva M, Ardalan M, Khalilov R et al (2022) Podocytopathy: The role of actin cytoskeleton. Biomed Pharmacother 156:113920. https://doi.org/10.1016/j.biopha.2022.113920
Wan H, Chen S, Cai Y, Chen Y, Wang Y, Zhang W et al (2021) Lead exposure and its association with cardiovascular disease and diabetic kidney disease in middle-aged and elderly diabetic patients. Int J Hyg Environ Health 231:113663. https://doi.org/10.1016/j.ijheh.2020.113663
Chen KH, Lin JL, Lin-Tan DT, Hsu HH, Hsu CW, Hsu KH et al (2012) Effect of chelation therapy on progressive diabetic nephropathy in patients with type 2 diabetes and high-normal body lead burdens. Am J Kidney Dis 60(4):530–538. https://doi.org/10.1053/j.ajkd.2012.04.028
Payton M, Hu H, Sparrow D, Weiss ST (1994) Low-level lead exposure and renal function in the Normative Aging Study. Am J Epidemiol 140(9):821–829. https://doi.org/10.1093/oxfordjournals.aje.a117330
Huang WH, Lin JL, Lin-Tan DT, Hsu CW, Chen KH, Yen TH (2013) Environmental lead exposure accelerates progressive diabetic nephropathy in type II diabetic patients. Biomed Res Int 2013:742545. https://doi.org/10.1155/2013/742545
Youssef D, Abboud E, Abou-Abbas L, Hassan H, Youssef J (2022) Prevalence and correlates of burnout among Lebanese health care workers during the COVID-19 pandemic: a national cross-sectional survey. J Pharm Policy Pract 15(1):102. https://doi.org/10.1186/s40545-022-00503-2
Jiang W, Wang J, Shen X, Lu W, Wang Y, Li W et al (2020) Establishment and Validation of a Risk Prediction Model for Early Diabetic Kidney Disease Based on a Systematic Review and Meta-Analysis of 20 Cohorts. Diabetes Care 43(4):925–933. https://doi.org/10.2337/dc19-1897
Kim Y, Lee BK (2012) Associations of blood lead, cadmium, and mercury with estimated glomerular filtration rate in the Korean general population: analysis of 2008-2010 Korean National Health and Nutrition Examination Survey data. Environ Res 118:124–129. https://doi.org/10.1016/j.envres.2012.06.003
Inker LA, Levey AS, Tighiouart H, Shafi T, Eckfeldt JH, Johnson C et al (2018) Performance of glomerular filtration rate estimating equations in a community-based sample of Blacks and Whites: the multiethnic study of atherosclerosis. Nephrol Dial Transplant 33(3):417–425. https://doi.org/10.1093/ndt/gfx042
Piani F, Melena I, Tommerdahl KL, Nokoff N, Nelson RG, Pavkov ME et al (2021) Sex-related differences in diabetic kidney disease: A review on the mechanisms and potential therapeutic implications. J Diabetes Complicat 35(4):107841. https://doi.org/10.1016/j.jdiacomp.2020.107841
Sattar N (2013) Revisiting the links between glycaemia, diabetes and cardiovascular disease. Diabetologia 56(4):686–695. https://doi.org/10.1007/s00125-012-2817-5
Mason LH, Harp JP, Han DY (2014) Pb neurotoxicity: neuropsychological effects of lead toxicity. Biomed Res Int 2014:840547. https://doi.org/10.1155/2014/840547
Dickerson AS, Hansen J, Specht AJ, Gredal O, Weisskopf MG (2019) Population-based study of amyotrophic lateral sclerosis and occupational lead exposure in Denmark. Occup Environ Med 76(4):208–214. https://doi.org/10.1136/oemed-2018-105469
Barry V, Steenland K (2019) Lead exposure and mortality among U.S. workers in a surveillance program: Results from 10 additional years of follow-up. Environ Res 177:108625. https://doi.org/10.1016/j.envres.2019.108625
Boskabady M, Marefati N, Farkhondeh T, Shakeri F, Farshbaf A, Boskabady MH (2018) The effect of environmental lead exposure on human health and the contribution of inflammatory mechanisms, a review. Environ Int 120:404–420. https://doi.org/10.1016/j.envint.2018.08.013
Lund I, Lund KE (2014) Lifetime smoking habits among Norwegian men and women born between 1890 and 1994: a cohort analysis using cross-sectional data. BMJ Open 4(10):e005539. https://doi.org/10.1136/bmjopen-2014-005539
Yanes LL, Sartori-Valinotti JC, Reckelhoff JF (2008) Sex steroids and renal disease: lessons from animal studies. Hypertension. 51(4):976–981. https://doi.org/10.1161/HYPERTENSIONAHA.107.105767
Tanaka R, Tsutsui H, Kobuchi S, Sugiura T, Yamagata M, Ohkita M et al (2012) Protective effect of 17beta-estradiol on ischemic acute kidney injury through the renal sympathetic nervous system. Eur J Pharmacol 683(1-3):270–275. https://doi.org/10.1016/j.ejphar.2012.02.044
Poolsup N, Suksomboon N, Aung N (2016) Effect of phosphodiesterase-5 inhibitors on glycemic control in person with type 2 diabetes mellitus: A systematic review and meta-analysis. J Clin Transl Endocrinol 6:50–55. https://doi.org/10.1016/j.jcte.2016.11.003
Naranjo VI, Hendricks M, Jones KS (2020) Lead Toxicity in Children: An Unremitting Public Health Problem. Pediatr Neurol 113:51–55. https://doi.org/10.1016/j.pediatrneurol.2020.08.005
Dignam T, Kaufmann RB, LeStourgeon L, Brown MJ (2019) Control of Lead Sources in the United States, 1970-2017: Public Health Progress and Current Challenges to Eliminating Lead Exposure. J Public Health Manag Pract 25:S13–S22. https://doi.org/10.1097/PHH.0000000000000889
Dapul H, Laraque D (2014) Lead poisoning in children. Adv Pediatr Infect Dis 61(1):313–333. https://doi.org/10.1016/j.yapd.2014.04.004
Jones RL, Homa DM, Meyer PA, Brody DJ, Caldwell KL, Pirkle JL et al (2009) Trends in Blood Lead Levels and Blood Lead Testing Among US Children Aged 1 to 5 Years, 1988-2004. Pediatrics. 123(3):e376–ee85. https://doi.org/10.1542/peds.2007-3608
Sadler RC, LaChance J, Hanna-Attisha M (2017) Social and Built Environmental Correlates of Predicted Blood Lead Levels in the Flint Water Crisis. Am J Public Health 107(5):763–769. https://doi.org/10.2105/AJPH.2017.303692
Wheeler W, Brown MJ (2013) Blood Lead Levels in Children Aged 1-5 Years - United States, 1999-2010. Mmwr-Morbid Mortal W 62(13):245–248
Meyer PA, Brown MJ, Falk H (2008) Global approach to reducing lead exposure and poisoning. Mutat Res 659(1-2):166–175. https://doi.org/10.1016/j.mrrev.2008.03.003
Zajac L, Kobrosly RW, Ericson B, Caravanos J, Landrigan PJ, Riederer AM (2020) Probabilistic estimates of prenatal lead exposure at 195 toxic hotspots in low- and middle-income countries. Environ Res 183:109251. https://doi.org/10.1016/j.envres.2020.109251
Kordas K, Ravenscroft J, Cao Y, McLean EV (2018) Lead Exposure in Low and Middle-Income Countries: Perspectives and Lessons on Patterns, Injustices, Economics, and Politics. Int J Environ Res Public Health 15(11). https://doi.org/10.3390/ijerph15112351
Zhang T, Yin X, Chen H, Li Y, Chen J, Yang X (2022) Global magnitude and temporal trends of idiopathic developmental intellectual disability attributable to lead exposure from 1990 to 2019: Results from Global Burden of Disease Study. Sci Total Environ 834:155366. https://doi.org/10.1016/j.scitotenv.2022.155366
Chowdhury R, Ramond A, O'Keeffe LM, Shahzad S, Kunutsor SK, Muka T et al (2018) Environmental toxic metal contaminants and risk of cardiovascular disease: systematic review and meta-analysis. BMJ. 362:k3310. https://doi.org/10.1136/bmj.k3310
Gambelunghe A, Sallsten G, Borne Y, Forsgard N, Hedblad B, Nilsson P et al (2016) Low-level exposure to lead, blood pressure, and hypertension in a population-based cohort. Environ Res 149:157–163. https://doi.org/10.1016/j.envres.2016.05.015
Jalili C, Kazemi M, Cheng H, Mohammadi H, Babaei A, Taheri E et al (2021) Associations between exposure to heavy metals and the risk of chronic kidney disease: a systematic review and meta-analysis. Crit Rev Toxicol 51(2):165–182. https://doi.org/10.1080/10408444.2021.1891196
Carrington C, Devleesschauwer B, Gibb HJ, Bolger PM (2019) Global burden of intellectual disability resulting from dietary exposure to lead, 2015. Environ Res 172:420–429. https://doi.org/10.1016/j.envres.2019.02.023
Ericson B, Dowling R, Dey S, Caravanos J, Mishra N, Fisher S et al (2018) A meta-analysis of blood lead levels in India and the attributable burden of disease. Environ Int 121(Pt 1):461–470. https://doi.org/10.1016/j.envint.2018.08.047
Acknowledgements
This research was funded by the Natural Science Foundation of Gansu Province (22JR5RA1069) and the Scientific Research Project of Health Industry in Gansu Province (GSWSKY2003-15).
Author information
Authors and Affiliations
Contributions
Conceptualization, L.M.; investigation, L.M.; writing—original draft preparation, Y.Z., C.X. and J.Y; writing—review and editing, Y.Z.,C.X.,J.Y.,J.Y.,S.Y.,N.L., S.Y., A.Y. and L.M.; supervision, A.Y. and L.M. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, Y., Xu, C., Yu, J. et al. Distributions and Trends of the Global Burden of DKD Attributable to Lead Exposure: A Systematic Analysis of GBD from 1990 to 2019. Biol Trace Elem Res (2024). https://doi.org/10.1007/s12011-024-04156-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12011-024-04156-x