Abstract
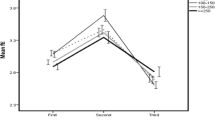
Iodine is essential for normal thyroid function, supporting healthy fetal and child development. The relevance between maternal iodine nutrition status and pregnancy outcomes remains controversial. The aim was to explore whether urinary iodine concentrations (UIC)/urinary creatinine (UCr) was associated with thyroid function and adverse pregnancy outcomes. This study was performed in the Department of Endocrinology and Metabolism of the First Affiliated Hospital of Nanjing Medical University. A total of 212 pregnant women were enrolled from May 2018 to November 2021, from the first visit until postpartum. Maternal serum samples were obtained in the second half of pregnancy, and then thyroid-stimulating hormone (TSH), free thyroxine (FT4), free triiodothyronine (FT3), UIC, and UCr were tested. The correlation of UIC/UCr, which represented maternal iodine nutrition status, with TSH, FT4, and FT3 was studied using linear regression. And we assessed associations between UIC/UCr and pregnancy outcomes. Notably, we explored consistency between UIC/UCr and the incidence of low birth weight (LBW) by application of logistic regression analysis. A total of 212 women were divided into 3 groups according to the upper and lower quartiles of UIC/UCr. There were 53 women in group 1 (UIC/UCr < 106.96 ug/g), 106 women in group 2 (UIC/UCr 106.96–259.08 ug/g), and 53 women in group 3 (UIC/UCr > 259.08 ug/g). The level of UIC/UCr had a negative correlation with FT4 (r = − 0.139, p = 0.043) but a positive correlation with TSH (r = 0.096, p = 0.162 > 0.05). There was a significant difference in the incidence of LBW among the 3 groups (p = 0.007). Logistic regression analysis found that the level of UIC/UCr was an independent factor for LBW (p = 0.048, OR = 0.991, 95%CI (0.982, 0.999)). The receiver operating characteristic (ROC) curve showed that the area under the curve (AUC) for UIC/UCr predicting the incidence of low birth weight was 0.687 (p = 0.013, 95%CI 0.575, 0.799). Lower UIC/UCr during pregnancy was associated with higher FT4 and lower TSH. And iodine deficiency during pregnancy is a risk factor for low birth weight. Our findings indicated that more attention should be paid to the appropriate iodine nutrition status in pregnant women, which can help prevent suffering from adverse pregnancy outcomes.




Similar content being viewed by others
Data Availability
The data of this study are available from the corresponding author upon request.
References
Alexander EK, Pearce EN, Brent GA, Brown RS, Chen H, Dosiou C, Grobman WA, Laurberg P, Lazarus JH, Mandel SJ et al (2017) 2017 Guidelines of the American Thyroid Association for the Diagnosis and Management of Thyroid Disease During Pregnancy and the Postpartum. Thyroid 27(3):315–389
Li C, Peng S, Zhang X, Xie X, Wang D, Mao J, Teng X, Shan Z, Teng W (2016) The urine iodine to creatinine as an optimal index of iodine during pregnancy in an iodine adequate area in China. J Clin Endocrinol Metab 101(3):1290–1298
Næss S, Markhus MW, Strand TA, Kjellevold M, Dahl L, Stokland AM, Nedrebø BG, Aakre I (2021) Iodine nutrition and iodine supplement initiation in association with thyroid function in mildly-to-moderately iodine-deficient pregnant and postpartum women. J Nutr 151(10):3187–3196
Levie D, Derakhshan A, Shu H, Broeren M, de Poortere RA, Peeters RP, Bornehag CG, Demeneix B, Korevaar T (2019) The association of maternal iodine status in early pregnancy with thyroid function in the Swedish Environmental Longitudinal, Mother and Child Asthma and Allergy Study. Thyroid 29(11):1660–1668
Abel MH, Korevaar T, Erlund I, Villanger GD, Caspersen IH, Arohonka P, Alexander J, Meltzer HM, Brantsæter AL (2018) Iodine intake is associated with thyroid function in mild to moderately iodine deficient pregnant women. Thyroid 28(10):1359–1371
Schiller T, Agmon A, Ostrovsky V, Shefer G, Knobler H, Zornitzki T (2020) Moderate iodine deficiency is common in pregnancy but does not alter maternal and neonatal thyroid function tests. Front Endocrinol (Lausanne) 11:523319
Charoenratana C, Leelapat P, Traisrisilp K, Tongsong T (2016) Maternal iodine insufficiency and adverse pregnancy outcomes. Matern Child Nutr 12(4):680–687
Snart C, Threapleton DE, Keeble C, Taylor E, Waiblinger D, Reid S, Alwan NA, Mason D, Azad R, Cade JE et al (2020) Maternal iodine status, intrauterine growth, birth outcomes and congenital anomalies in a UK birth cohort. BMC Med 18(1):132
Nazarpour S, Ramezani TF, Amiri M, Simbar M, Tohidi M, Bidhendi YR, Azizi F (2020) Maternal urinary iodine concentration and pregnancy outcomes: Tehran thyroid and pregnancy study. Biol Trace Elem Res 194(2):348–359
Abel MH, Caspersen IH, Sengpiel V, Jacobsson B, Meltzer HM, Magnus P, Alexander J, Brantsæter AL (2020) Insufficient maternal iodine intake is associated with subfecundity, reduced foetal growth, and adverse pregnancy outcomes in the Norwegian mother, father and child cohort study. BMC Med 18(1):211
Snart C, Keeble C, Taylor E, Cade JE, Stewart PM, Zimmermann M, Reid S, Threapleton DE, Poston L, Myers JE et al (2019) Maternal iodine status and associations with birth outcomes in three major cities in the United Kingdom. Nutrients 11(2)
León G, Murcia M, Rebagliato M, Álvarez-Pedrerol M, Castilla AM, Basterrechea M, Iñiguez C, Fernández-Somoano A, Blarduni E, Foradada CM et al (2015) Maternal thyroid dysfunction during gestation, preterm delivery, and birthweight. The Infancia y Medio Ambiente Cohort, Spain. Paediatr Perinat Epidemiol 29(2):113–122
Torlinska B, Bath SC, Janjua A, Boelaert K, Chan SY (2018) Iodine status during pregnancy in a region of mild-to-moderate iodine deficiency is not associated with adverse obstetric outcomes; results from the Avon Longitudinal Study of Parents and Children (ALSPAC). Nutrients 10(3)
Liu J, Yu X, Xia M, Cai H, Cheng G, Wu L, Li Q, Zhang Y, Sheng M, Liu Y et al (2017) Development of gestation-specific reference intervals for thyroid hormones in normal pregnant Northeast Chinese women: what is the rational division of gestation stages for establishing reference intervals for pregnancy women? Clin Biochem 50(6):309–317
Carlé A, Krejbjerg A, Laurberg P (2014) Epidemiology of nodular goitre. Influence of iodine intake. Best Pract Res Clin Endocrinol Metab 28(4):465–479
Shi X, Han C, Li C, Mao J, Wang W, Xie X, Li C, Xu B, Meng T, Du J et al (2015) Optimal and safe upper limits of iodine intake for early pregnancy in iodine-sufficient regions: a cross-sectional study of 7190 pregnant women in China. J Clin Endocrinol Metab 100(4):1630–1638
Andersson M, Braegger CP (2022) The role of iodine for thyroid function in lactating women and infants. Endocr Rev 43(3):469–506
Mulder TA, Korevaar T, Peeters RP, van Herwaarden AE, de Rijke YB, White T, Tiemeier H (2021) Urinary iodine concentrations in pregnant women and offspring brain morphology. Thyroid 31(6):964–972
Chen R, Li Q, Cui W, Wang X, Gao Q, Zhong C, Sun G, Chen X, Xiong G, Yang X et al (2018) Maternal iodine insufficiency and excess are associated with adverse effects on fetal growth: a prospective cohort study in Wuhan, China. J Nutr 148(11):1814–1820
Sun Y, Han Y, Qian M, Li Y, Ye Y, Lin L, Liu Y (2021) Defending effects of iodide transfer in placental barrier against maternal iodine deficiency. Thyroid 31(3):509–518
Habibi N, Grieger JA, Bianco-Miotto T (2020) A review of the potential interaction of selenium and iodine on placental and child health. Nutrients 12(9)
Velasco I, Sánchez-Gila M, Manzanares S, Taylor P, García-Fuentes E (2020) Iodine status, thyroid function, and birthweight: a complex relationship in high-risk pregnancies. J Clin Med 9(1)
Eastman CJ, Ma G, Li M (2019) Optimal assessment and quantification of iodine nutrition in pregnancy and lactation: laboratory and clinical methods, controversies and future directions. Nutrients 11(10)
Chen GD, Pang TT, Lu XF, Li PS, Zhou ZX, Ye SX, Yang J, Shen XY, Lin DX, Fan DZ et al (2020) Associations between maternal thyroid function and birth outcomes in Chinese mother-child dyads: a retrospective cohort study. Front Endocrinol (Lausanne) 11:611071
Zhang C, Yang X, Zhang Y, Guo F, Yang S, Peeters RP, Korevaar T, Fan J, Huang HF (2019) Association between maternal thyroid hormones and birth weight at early and late pregnancy. J Clin Endocrinol Metab 104(12):5853–5863
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Hongying Zha, Lin Yu, Yi Tang and Lu Sun. The first draft of the manuscript was written by Hongying Zha and Lin Yu, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Hongying Zha and Lin Yu are contributed equally to this work.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zha, H., Yu, L., Tang, Y. et al. Effect of Iodine Nutrition Status on Thyroid Function and Pregnancy Outcomes. Biol Trace Elem Res 201, 5143–5151 (2023). https://doi.org/10.1007/s12011-023-03600-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-023-03600-8