Abstract
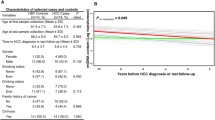
Arsenic (As) can cause liver damage and liver cancer and is capable of seriously affecting human health. Therefore, it is important to identify biomarkers of arsenic-induced liver damage. Mitochondria are key targets of hepatotoxicity caused by arsenic. The mitochondrial DNA copy number (mtDNAcn) is the number of mitochondrial DNA (mtDNA) copies in the genome. mtDNA is vulnerable to exogenous chemical attacks, thus causing mtDNAcn to change after exposure to environmental pollutants. Therefore, mtDNAcn can serve as a potential marker to identify and assess the risk of diseases caused by exposure to environmental pollutants. In this study, we selected 272 arsenicosis patients (155 cases without liver damage and 117 cases with liver damage) and 218 participants not exposed to arsenic (155 cases without liver damage and 63 cases with liver damage) as subjects to investigate the correlation between peripheral blood mtDNAcn and arsenic-induced liver damage, as well as the ability of peripheral blood mtDNAcn to identify and assess the risk of arsenic-induced liver damage. Peripheral blood mtDNAcn in patients with arsenic-induced liver damage is significantly decreased and negatively correlated with serum ALT, AST, and GGT levels. The decrease of peripheral blood mtDNAcn was associated with an increased risk of arsenic-induced liver damage. The receiver operating characteristic (ROC) curve analysis indicated that peripheral blood mtDNAcn could specifically identify patients with liver damage in the arsenicosis group. The decision tree C5.0 model was established to identify arsenicosis in all patients with liver damage. Peripheral blood mtDNAcn was included in the model and played the most important role in the identification of arsenic-induced liver damage. This study provided a basis for the identification and evaluation of arsenic-induced liver damage by peripheral blood mtDNAcn, indicating that peripheral blood mtDNAcn is expected to be a potential biomarker of arsenic-induced liver damage, and provides clues for exploring the mechanism of arsenic-induced liver damage from mitochondria damage.



Similar content being viewed by others
Data Availability
The data that support the findings of this study, titled “Association and risk of peripheral blood mitochondrial DNA copy number with arsenic-induced liver damage,” are available from the corresponding author upon reasonable request.
References
Carlin D, Naujokas M, Bradham K, Cowden J, Heacock M, Henry H, Lee J, Thomas D, Thompson C, Tokar E, Waalkes M, Birnbaum L, Suk W (2016) Arsenic and environmental health: state of the science and future research opportunities. Environ Health Perspect 124(7):890–899. https://doi.org/10.1289/ehp.1510209
Bundschuh J, Niazi N, Alam M, Berg M, Herath I, Tomaszewska B, Maity J, Ok Y (2022) Global arsenic dilemma and sustainability. J Hazard Mater 436:129197. https://doi.org/10.1016/j.jhazmat.2022.129197
Podgorski J, Berg M (2020) Global threat of arsenic in groundwater. Science (New York, NY) 368(6493):845–850. https://doi.org/10.1126/science.aba1510
Chen Q, Costa M (2021) Arsenic: a global environmental challenge. Annu Rev Pharmacol Toxicol 61:47–63. https://doi.org/10.1146/annurev-pharmtox-030220-013418
Wadgaonkar P, Chen F (2021) Connections between endoplasmic reticulum stress-associated unfolded protein response, mitochondria, and autophagy in arsenic-induced carcinogenesis. Semin Cancer Biol 76:258–266. https://doi.org/10.1016/j.semcancer.2021.04.004
Zhang W, Miao A, Wang N, Li C, Sha J, Jia J, Alessi D, Yan B, Ok Y (2022) Arsenic bioaccumulation and biotransformation in aquatic organisms. Environ Int 163:107221. https://doi.org/10.1016/j.envint.2022.107221
Liu J, Zheng B, Aposhian H, Zhou Y, Chen M, Zhang A, Waalkes M (2002) Chronic arsenic poisoning from burning high-arsenic-containing coal in Guizhou, China. Environ Health Perspect 110(2):119–122. https://doi.org/10.1289/ehp.02110119
Wang D, Luo P, Zou Z, Wang Q, Yao M, Yu C, Wei S, Sun B, Zhu K, Zeng Q, Li J, Liang B, Zhang A (2019) Alterations of arsenic levels in arsenicosis residents and awareness of its risk factors: a population-based 20-year follow-up study in a unique coal-borne arsenicosis County in Guizhou, China. Environ Int 129:18–27. https://doi.org/10.1016/j.envint.2019.05.005
Yao M, Zeng Q, Luo P, Sun B, Liang B, Wei S, Xu Y, Wang Q, Liu Q, Zhang A (2021) Assessing the risk of coal-burning arsenic-induced liver damage: a population-based study on hair arsenic and cumulative arsenic. Environ Sci Pollut Res Int 28(36):50489–50499. https://doi.org/10.1007/s11356-021-14273-y
Zeng Q, Zou Z, Wang Q, Sun B, Liu Y, Liang B, Liu Q, Zhang A (2019) Association and risk of five miRNAs with arsenic-induced multiorgan damage. Sci Total Environ 680:1–9. https://doi.org/10.1016/j.scitotenv.2019.05.042
Liou C, Chen S, Lin T, Tsai M, Chang C (2021) APOE4 oxidative stress biomarkers and mitochondrial DNA copy number associated with allele and cholinesterase inhibitor therapy in patients with Alzheimer’s disease. Antioxidants (Basel, Switzerland) 10(12). https://doi.org/10.3390/antiox10121971
Martens L, Luo J, Wermer M, Willems van Dijk K, Hägg S, Grassmann F, Noordam R, van Heemst D (2022) The association between mitochondrial DNA abundance and stroke: a combination of multivariable-adjusted survival and Mendelian randomization analyses. Atherosclerosis 354:1–7. https://doi.org/10.1016/j.atherosclerosis.2022.06.1012
Kronenberg F, Eckardt K (2022) Mitochondrial DNA and kidney function. Clin J Am Soc Nephrol: CJASN. https://doi.org/10.2215/cjn.05820522
Liu J, Wang Y, Shi Q, Wang X, Zou P, Zheng M, Luan Q (2022) Mitochondrial DNA efflux maintained in gingival fibroblasts of patients with periodontitis through ROS/mPTP pathway. Oxid Med Cell Longev 2022:1000213. https://doi.org/10.1155/2022/1000213
Bordoni L, Petracci I, Pelikant-Malecka I, Radulska A, Piangerelli M, Samulak J, Lewicki L, Kalinowski L, Gabbianelli R, Olek R (2021) Mitochondrial DNA copy number and trimethylamine levels in the blood: new insights on cardiovascular disease biomarkers. FASEB J 35(7):e21694. https://doi.org/10.1096/fj.202100056R
He W, Li C, Huang Z, Geng S, Rao V, Kelly T, Hamm L, Grams M, Arking D, Appel L, Rebholz C (2022) Association of mitochondrial DNA copy number with risk of progression of kidney disease. Clin J Am Soc Nephrol: CJASN 17(7):966–975. https://doi.org/10.2215/cjn.15551121
Li R, Chen G, Liu X, Pan M, Kang N, Hou X, Liao W, Dong X, Yuchi Y, Mao Z, Huo W, Wang X, Guo Y, Li S, Hou J, Wang C (2022) Aging biomarkers: potential mediators of association between long-term ozone exposure and risk of atherosclerosis. J Intern Med. https://doi.org/10.1111/joim.13500
Cantoni O, Zito E, Guidarelli A, Fiorani M, Ghezzi P (2022) Mitochondrial ROS, ER stress, and Nrf2 crosstalk in the regulation of mitochondrial apoptosis induced by arsenite. Antioxidants (Basel, Switzerland) 11(5). https://doi.org/10.3390/antiox11051034
Du X, Luo L, Huang Q, Zhang J (2022) Cortex metabolome and proteome analysis reveals chronic arsenic exposure via drinking water induces developmental neurotoxicity through hnRNP L mediated mitochondrial dysfunction in male rats. Sci Total Environ 820:153325. https://doi.org/10.1016/j.scitotenv.2022.153325
Wei S, Qiu T, Yao X, Wang N, Jiang L, Jia X, Tao Y, Wang Z, Pei P, Zhang J, Zhu Y, Yang G, Liu X, Liu S, Sun X (2020) Arsenic induces pancreatic dysfunction and ferroptosis via mitochondrial ROS-autophagy-lysosomal pathway. J Hazard Mater 384:121390. https://doi.org/10.1016/j.jhazmat.2019.121390
Choudhury S, Ghosh S, Mukherjee S, Gupta P, Bhattacharya S, Adhikary A, Chattopadhyay S (2016) Pomegranate protects against arsenic-induced p53-dependent ROS-mediated inflammation and apoptosis in liver cells. J Nutr Biochem 38:25–40. https://doi.org/10.1016/j.jnutbio.2016.09.001
Scheffler I (2001) A century of mitochondrial research: achievements and perspectives. Mitochondrion 1(1):3–31. https://doi.org/10.1016/s1567-7249(00)00002-7
Jia X, Qiu T, Yao X, Jiang L, Wang N, Wei S, Tao Y, Pei P, Wang Z, Zhang J, Zhu Y, Yang G, Liu X, Liu S, Sun X (2020) Arsenic induces hepatic insulin resistance via mtROS-NLRP3 inflammasome pathway. J Hazard Mater 399:123034. https://doi.org/10.1016/j.jhazmat.2020.123034
Lee C, Yu H (2016) Role of mitochondria, ROS, and DNA damage in arsenic induced carcinogenesis. Front Biosci (Schol Ed) 8(2):312–320. https://doi.org/10.2741/s465
Hu Y, Xiao T, Zhang A (2021) Associations between and risks of trace elements related to skin and liver damage induced by arsenic from coal burning. Ecotoxicol Environ Saf 208:111719. https://doi.org/10.1016/j.ecoenv.2020.111719
Wu I, Lin C, Liu C, Hsu C, Chen C, Hsiung C (2017) Interrelations between mitochondrial DNA copy number and inflammation in older adults. J Gerontol A Biol Sci Med Sci 72(7):937–944. https://doi.org/10.1093/gerona/glx033
Li D, An D, Zhou Y, Liu J, Waalkes M (2006) Current status and prevention strategy for coal-arsenic poisoning in Guizhou, China. J Health Popul Nutr 24(3):273–276
Zhang A, Feng H, Yang G, Pan X, Jiang X, Huang X, Dong X, Yang D, Xie Y, Peng L, Jun L, Hu C, Jian L, Wang X (2007) Unventilated indoor coal-fired stoves in Guizhou province, China: cellular and genetic damage in villagers exposed to arsenic in food and air. Environ Health Perspect 115(4):653–658. https://doi.org/10.1289/ehp.9272
Dong L, Liu Y, Wang D, Zhu K, Zou Z, Zhang A (2021) Imbalanced inflammatory response in subchronic arsenic-induced liver injury and the protective effects of Ginkgo biloba extract in rats: potential role of cytokines mediated cell-cell interactions. Environ Toxicol 36(10):2073–2092. https://doi.org/10.1002/tox.23324
Xue J, Xiao T, Wei S, Sun J, Zou Z, Shi M, Sun Q, Dai X, Wu L, Li J, Xia H, Tang H, Zhang A, Liu Q (2021) miR-21-regulated M2 polarization of macrophage is involved in arsenicosis-induced hepatic fibrosis through the activation of hepatic stellate cells. J Cell Physiol 236(8):6025–6041. https://doi.org/10.1002/jcp.30288
Flora KD, Keeffe EB (1990) Significance of mildly elevated liver tests on screening biochemistry profiles. J Insur Med (New York, NY) 22
Tanwar S, Rhodes F, Srivastava A, Trembling PM, Rosenberg WM (2020) Inflammation and fibrosis in chronic liver diseases including non-alcoholic fatty liver disease and hepatitis C. World J Gastroenterol 26(2):109–133. https://doi.org/10.3748/wjg.v26.i2.109
Maurice J, Manousou P (2018) Non-alcoholic fatty liver disease. Clin Med (Lond) 18(3):245–250. https://doi.org/10.7861/clinmedicine.18-3-245
Danan G, Teschke R (2016) RUCAM in drug and herb induced liver injury: the update. Int J Mol Sci 17(1):14. https://doi.org/10.3390/ijms17010014
Teschke R, Xuan T (2022) Heavy metals, halogenated hydrocarbons, phthalates, glyphosate, cordycepin, alcohol, drugs, and herbs, assessed for liver injury and mechanistic steps. Front Biosci (Landmark edition) 27(11):314. https://doi.org/10.31083/j.fbl2711314
Eldeeb M, Thomas R, Ragheb M, Fallahi A, Fon E (2022) Mitochondrial quality control in health and in Parkinson’s disease. Physiol Rev. https://doi.org/10.1152/physrev.00041.2021
Xu Y, Zeng Q, Sun B, Wei S, Wang Q, Zhang A (2022) Assessing the role of Nrf2/GPX4-mediated oxidative stress in arsenic-induced liver damage and the potential application value of Rosa roxburghii Tratt [Rosaceae]. Oxid Med Cell Longev 2022:9865606. https://doi.org/10.1155/2022/9865606
He Q, Sun X, Zhang M, Chu L, Zhao Y, Wu Y, Zhang J, Han X, Guan S, Ding C (2022) Protective effect of baicalin against arsenic trioxide-induced acute hepatic injury in mice through JAK2/STAT3 signaling pathway. Int J Immunopathol Pharmacol 36:20587384211073396. https://doi.org/10.1177/20587384211073397
Zhang M, Xue Y, Zheng B, Li L, Chu X, Zhao Y, Wu Y, Zhang J, Han X, Wu Z, Chu L (2021) Liquiritigenin protects against arsenic trioxide-induced liver injury by inhibiting oxidative stress and enhancing mTOR-mediated autophagy. Biomed Pharmacother = Biomed Pharmacother 143:112167. https://doi.org/10.1016/j.biopha.2021.112167
Santra A, Bishnu D, Santra S, Ghatak S, Mukherjee P, Dhali G, Chowdhury A (2022) Arsenic-induced injury of mouse hepatocytes through lysosome and mitochondria: an in vitro study. Int J Hepatol 2022:1546297. https://doi.org/10.1155/2022/1546297
Teschke R (2022) Aluminum, arsenic, beryllium, cadmium, chromium, cobalt, copper, iron, lead, mercury, molybdenum, nickel, platinum, thallium, titanium, vanadium, and zinc: molecular aspects in experimental liver injury. Int J Mol Sci 23 (20). https://doi.org/10.3390/ijms232012213
Ahmad S, Kitchin K, Cullen W (2000) Arsenic species that cause release of iron from ferritin and generation of activated oxygen. Arch Biochem Biophys 382(2):195–202. https://doi.org/10.1006/abbi.2000.2023
Dixon S, Lemberg K, Lamprecht M, Skouta R, Zaitsev E, Gleason C, Patel D, Bauer A, Cantley A, Yang W, Morrison B, Stockwell B (2012) Ferroptosis: an iron-dependent form of nonapoptotic cell death. Cell 149(5):1060–1072. https://doi.org/10.1016/j.cell.2012.03.042
Wei S, Qiu T, Wang N, Yao X, Jiang L, Jia X, Tao Y, Zhang J, Zhu Y, Yang G, Liu X, Liu S, Sun X (2020) Ferroptosis mediated by the interaction between Mfn2 and IREα promotes arsenic-induced nonalcoholic steatohepatitis. Environ Res 188:109824. https://doi.org/10.1016/j.envres.2020.109824
Liu Y, Liu Y (2022) Mitochondrial toxicity of organic arsenicals. Methods Mol Biol (Clifton, NJ) 2497:173–184. https://doi.org/10.1007/978-1-0716-2309-1_11
Han X, Yang Y, Zhang M, Chu X, Zheng B, Liu C, Xue Y, Guan S, Sun S, Jia Q (2022) Protective effects of 6-gingerol on cardiotoxicity induced by arsenic trioxide through AMPK/SIRT1/PGC-1α signaling pathway. Front Pharmacol 13:868393. https://doi.org/10.3389/fphar.2022.868393
Hu T, Lu J, Wu C, Duan T, Luo P (2022) Dictyophora polysaccharide attenuates As-mediated PINK1/Parkin pathway-induced mitophagy in L-02 cell through scavenging ROS. Molecules (Basel, Switzerland) 27 (9). https://doi.org/10.3390/molecules27092806
Bodaghi-Namileh V, Sepand M, Omidi A, Aghsami M, Seyednejad S, Kasirzadeh S, Sabzevari O (2018) Acetyl-l-carnitine attenuates arsenic-induced liver injury by abrogation of mitochondrial dysfunction, inflammation, and apoptosis in rats. Environ Toxicol Pharmacol 58:11–20. https://doi.org/10.1016/j.etap.2017.12.005
Miltonprabu S, Sumedha N (2014) Arsenic-induced hepatic mitochondrial toxicity in rats and its amelioration by diallyl trisulfide. Toxicol Mech Methods 24(2):124–135. https://doi.org/10.3109/15376516.2013.869778
Cordier W, Yousaf M, Nell M, Steenkamp V (2021) Underlying mechanisms of cytotoxicity in HepG2 hepatocarcinoma cells exposed to arsenic, cadmium and mercury individually and in combination. Toxicol In Vitro 72:105101. https://doi.org/10.1016/j.tiv.2021.105101
Cheng S, Zhang H, Wang P, Zou K, Duan X, Wang S, Yang Y, Shi L, Wang W (2021) Benchmark dose analysis for PAHs hydroxyl metabolites in urine based on mitochondrial damage of peripheral blood leucocytes in coke oven workers in China. Environ Toxicol Pharmacol 86:103675. https://doi.org/10.1016/j.etap.2021.103675
Ghosh M, Janssen L, Martens D, Öner D, Vlaanderen J, Pronk A, Kuijpers E, Vermeulen R, Nawrot T, Godderis L, Hoet P (2020) Increased telomere length and mtDNA copy number induced by multi-walled carbon nanotube exposure in the workplace. J Hazard Mater 394:122569. https://doi.org/10.1016/j.jhazmat.2020.122569
Wang X, Hart J, Liu Q, Wu S, Nan H, Laden F (2020) Association of particulate matter air pollution with leukocyte mitochondrial DNA copy number. Environ Int 141:105761. https://doi.org/10.1016/j.envint.2020.105761
Song L, Liu B, Wang L, Wu M, Zhang L, Liu Y, Bi J, Yang S, Zhang B, Xia W, Xu S, Chen R, Cao Z, Wang Y (2020) Exposure to arsenic during pregnancy and newborn mitochondrial DNA copy number: a birth cohort study in Wuhan. China. Chemosphere 243:125335. https://doi.org/10.1016/j.chemosphere.2019.125335
Prakash C, Kumar V (2016) Arsenic-induced mitochondrial oxidative damage is mediated by decreased PGC-1α expression and its downstream targets in rat brain. Chem Biol Interact 256:228–235. https://doi.org/10.1016/j.cbi.2016.07.017
Partridge M, Huang S, Hernandez-Rosa E, Davidson M, Hei T (2007) Arsenic induced mitochondrial DNA damage and altered mitochondrial oxidative function: implications for genotoxic mechanisms in mammalian cells. Can Res 67(11):5239–5247. https://doi.org/10.1158/0008-5472.Can-07-0074
Lou Q, Zhang M, Zhang K, Liu X, Zhang Z, Zhang X, Yang Y, Gao Y (2022) Arsenic exposure elevated ROS promotes energy metabolic reprogramming with enhanced AKT-dependent HK2 expression. Sci Total Environ 836:155691. https://doi.org/10.1016/j.scitotenv.2022.155691
Sanyal T, Bhattacharjee P, Bhattacharjee S, Bhattacharjee P (2018) Hypomethylation of mitochondrial D-loop and ND6 with increased mitochondrial DNA copy number in the arsenic-exposed population. Toxicology 408:54–61. https://doi.org/10.1016/j.tox.2018.06.012
Sanyal T, Paul M, Bhattacharjee S, Bhattacharjee P (2020) Epigenetic alteration of mitochondrial biogenesis regulatory genes in arsenic exposed individuals (with and without skin lesions) and in skin cancer tissues: a case control study. Chemosphere 258:127305. https://doi.org/10.1016/j.chemosphere.2020.127305
Jiang Y, Li X, Zhou W, Jin M, Li S, Lao Y, Zhu H, Wang J (2022) Clinical significance of serum ferritin in patients with systemic sclerosis. J Clin Lab Anal e24597. https://doi.org/10.1002/jcla.24597
Gao H, Xue Y, Wu L, Huo J, Pang Y, Chen J, Gao Q (2022) Lycium ruthenicum protective effect of polyphenols on oxidative stress against acrylamide induced liver injury in rats. Molecules (Basel, Switzerland) 27 (13). https://doi.org/10.3390/molecules27134100
Quan Y, Xin Y, Tian G, Zhou J, Liu X (2020) Mitochondrial ROS-modulated mtDNA: a potential target for cardiac aging. Oxid Med Cell Longev 2020:9423593. https://doi.org/10.1155/2020/9423593
Prakash C, Kumar V (2016) Chronic arsenic exposure-induced oxidative stress is mediated by decreased mitochondrial biogenesis in rat liver. Biol Trace Elem Res 173(1):87–95. https://doi.org/10.1007/s12011-016-0622-6
Zhong G, Hu T, Tang L, Li T, Wu S, Duan X, Pan J, Zhang H, Tang Z, Feng X, Hu L (2021) Arsenic causes mitochondrial biogenesis obstacles by inhibiting the AMPK/PGC-1α signaling pathway and also induces apoptosis and dysregulated mitophagy in the duck liver. Ecotoxicol Environ Saf 230:113117. https://doi.org/10.1016/j.ecoenv.2021.113117
Datta A, Alam MJ, Khaleda L, Al-Forkan M (2021) Protective effects of Corchorus olitorius and Butea monosperma against arsenic induced aberrant methylation and mitochondrial DNA damage in wistar rat model. Toxicol Rep 8:30–37. https://doi.org/10.1016/j.toxrep.2020.12.017
Funding
This study was supported by the National Natural Science Foundation of China (no. 81430077, no. U1812403).
Author information
Authors and Affiliations
Contributions
Qi Wang: participated in investigations, performed the research, collected and analyzed the data, visualized the data, drafted the paper, and performed statistical analysis. Lu Ma: participated in investigations, reviewed and edited the paper. Baofei Sun: participated in investigations, provided quality supervision. Aihua Zhang: conceived and designed the research, organizing investigations, performed data curation, reviewed and edited the paper, obtained research funding, provided administrative, technical, and material support, and supported the study.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
This study was reviewed and approved by the Ethics Committee of Guizhou Medical University (no. 201403001), and all subjects signed written informed consent. The procedure was performed in accordance with all relevant guidelines and regulations.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, Q., Ma, L., Sun, B. et al. Reduced Peripheral Blood Mitochondrial DNA Copy Number as Identification Biomarker of Suspected Arsenic-Induced Liver Damage. Biol Trace Elem Res 201, 5083–5097 (2023). https://doi.org/10.1007/s12011-023-03584-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-023-03584-5