Abstract
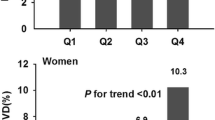
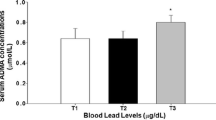
We aimed to explore whether an elevated blood lead level (BLL) is associated with visceral adipose dysfunction in patients with type 2 diabetes mellitus (T2DM). Four thousand one hundred and fourteen diabetic participants were enrolled from seven communities in Shanghai in 2018 in the cross-sectional METAL study. BLL was measured by graphite furnace atomic absorption spectrometry. Visceral adiposity index (VAI) and lipid accumulation product (LAP)were calculated by simple anthropometric and biochemical parameters. We found that medians (IQR) of BLL were 26.0 μg/L (18.0–37.0) for men and 25.0 μg/L (18.0–35.0) for women, respectively. In men, each doubling of BLL was associated with a 2.0% higher VAI (95% CI, 0.6 to 3.5%) and 1.8% higher LAP (95% CI, 0.2 to 3.3%) after full adjustment. Using the lowest BLL quartile as the referent group, significant positive trends were observed for BLL with VAI and LAP. In women, each doubling of BLL was associated with a 1.9% higher LAP (95% CI, 0.6 to 3.1%). Additionally, there was a marginally significant positive association between BLL and VAI, either using log2-transformed concentrations as continuous variables or categorized in quartiles. In conclusion, lead exposure is associated with visceral adipose dysfunction in patients with T2DM. Further prospective studies are warranted to confirm our findings.
Similar content being viewed by others
Data Availability
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Jaacks LM, Vandevijvere S, Pan A, McGowan CJ, Wallace C, Imamura F, Mozaffarian D, Swinburn B, Ezzati M (2019) The obesity transition: stages of the global epidemic. Lancet Diabetes Endocrinol 7:231–240
Sun H et al (2022) IDF Diabetes Atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract 183:109119
Pappachan JM, Fernandez CJ, Chacko EC (2019) Diabesity and antidiabetic drugs. Mol Aspects Med 66:3–12
Bhupathiraju SN, Hu FB (2016) Epidemiology of obesity and diabetes and their cardiovascular complications. Circ Res 118:1723–1735
Wan H, Wang Y, Xiang Q, Fang S, Chen Y, Chen C, Zhang W, Zhang H, Xia F, Wang N, Lu Y (2020) Associations between abdominal obesity indices and diabetic complications: Chinese visceral adiposity index and neck circumference. Cardiovasc Diabetol 19:118
Zhao L, Huang G, Xia F, Li Q, Han B, Chen Y, Chen C, Lin D, Wang N, Lu Y (2018) Neck circumference as an independent indicator of visceral obesity in a Chinese population. Lipids Health Dis 17:85
Brown JC, Harhay MO, Harhay MN (2018) Anthropometrically predicted visceral adipose tissue and blood-based biomarkers: a cross-sectional analysis. Eur J Nutr 57:191–198
Petta S, Amato M, Cabibi D, Camma C, Di Marco V, Giordano C, Galluzzo A, Craxi A (2010) Visceral adiposity index is associated with histological findings and high viral load in patients with chronic hepatitis C due to genotype 1. Hepatology (Baltimore, Md.) 52:1543–52
Amato MC, Giordano C, Galia M, Criscimanna A, Vitabile S, Midiri M, Galluzzo A (2010) Visceral Adiposity Index: a reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care 33:920–922
Piché ME, Tchernof A, Després JP (2020) Obesity phenotypes, diabetes, and cardiovascular diseases. Circ Res 126:1477–1500
Kahn HS (2005) The “lipid accumulation product” performs better than the body mass index for recognizing cardiovascular risk: a population-based comparison. BMC Cardiovasc Disord 5:26
Ribeiro CM, Beserra BTS, Silva NG, Lima CL, Rocha PRS, Coelho MS, Neves FAR, Amato AA (2020) Exposure to endocrine-disrupting chemicals and anthropometric measures of obesity: a systematic review and meta-analysis. BMJ Open 10:e033509
Mitra A, Chatterjee S, Kataki S, Rastogi RP, Gupta DK (2021) Bacterial tolerance strategies against lead toxicity and their relevance in bioremediation application. Environ Sci Pollut Res Int 28:14271–14284
Obeng-Gyasi E (2019) Sources of lead exposure in various countries. Rev Environ Health 34:25–34
Wang T, Zhang J, Xu Y (2020) Epigenetic basis of lead-induced neurological disorders. Int J Environ Res Public Health 17:4878
Leff T, Stemmer P, Tyrrell J, Jog R (2018) Diabetes and exposure to environmental lead (Pb). Toxics 6:54
Chen C, Li Q, Nie X, Han B, Chen Y, Xia F, Zhai H, Wang N, Lu Y (2017) Association of lead exposure with cardiovascular risk factors and diseases in Chinese adults. Environ Sci Pollut Res Int 24:22275–22283
Chen C, Wang N, Zhai H, Nie X, Sun H, Han B, Li Q, Chen Y, Cheng J, Xia F, Zhao L, Zheng Y, Shen Z, Lu Y (2016) Associations of blood lead levels with reproductive hormone levels in men and postmenopausal women: results from the SPECT-China Study. Sci Rep 6:37809
Wan H, Chen S, Cai Y, Chen Y, Wang Y, Zhang W, Chen C, Wang N, Guo Y, Lu Y (2021) Lead exposure and its association with cardiovascular disease and diabetic kidney disease in middle-aged and elderly diabetic patients. Int J Hyg Environ Health 231:113663
Hagedoorn IJM, Gant CM, Huizen SV, Maatman R, Navis G, Bakker SJL, Laverman GD (2020) Lifestyle-related exposure to cadmium and lead is associated with diabetic kidney disease. J Clin Med 9:2432
Lamas GA, Goertz C, Boineau R, Mark DB, Rozema T, Nahin RL, Lindblad L, Lewis EF, Drisko J, Lee KL (2013) Effect of disodium EDTA chelation regimen on cardiovascular events in patients with previous myocardial infarction: the TACT randomized trial. JAMA 309:1241–1250
İsa Ardahanlı RA, Çelik M, Akgün O, Akyüz O (2021) Effects of empagliflozin on carotid intima-media thickness and epicardial fat tissue volume in patients with type-2 diabetes mellitus. Lokman Hekim Health Sci 1:74–80
Wang N, Wang X, Li Q, Han B, Chen Y, Zhu C, Chen Y, Lin D, Wang B, Jensen MD, Lu Y (2017) The famine exposure in early life and metabolic syndrome in adulthood. Clin Nutr 36:253–259
Chen C, Xu H, Chen Y, Chen Y, Li Q, Hu J, Liang W, Cheng J, Xia F, Wang C, Han B, Zheng Y, Jiang B, Wang N, Lu Y (2017) Iodized salt intake and its association with urinary iodine, thyroid peroxidase antibodies, and thyroglobulin antibodies among urban Chinese. Thyroid 27:1566–1573
Chen C, Zhai H, Cheng J, Weng P, Chen Y, Li Q, Wang C, Xia F, Wang N, Lu Y (2019) Causal link between vitamin D and total testosterone in men: a Mendelian randomization analysis. J Clin Endocrinol Metab 104:3148–3156
Chen C, Chen Q, Nie B, Zhang H, Zhai H, Zhao L, Xia P, Lu Y, Wang N (2020) Trends in bone mineral density, osteoporosis, and osteopenia among U.S. adults with prediabetes, 2005–2014. Diabetes Care 43:1008–1015
Xu Y et al (2013) Prevalence and control of diabetes in Chinese adults. JAMA 310:948–959
Zhai H, Chen C, Wang N, Chen Y, Nie X, Han B, Li Q, Xia F, Lu Y (2017) Blood lead level is associated with non-alcoholic fatty liver disease in the Yangtze River Delta region of China in the context of rapid urbanization. Environ Health 16:93
Amato MC, Giordano C (2014) Visceral adiposity index: an indicator of adipose tissue dysfunction. Int J Endocrinol 2014:730827
Huang X, Jiang X, Wang L, Chen L, Wu Y, Gao P, Hua F (2019) Visceral adipose accumulation increased the risk of hyperuricemia among middle-aged and elderly adults: a population-based study. J Transl Med 17:341
Du T, Yu X, Zhang J, Sun X (2015) Lipid accumulation product and visceral adiposity index are effective markers for identifying the metabolically obese normal-weight phenotype. Acta Diabetol 52:855–863
Ferreira FG, Juvanhol LL, da Silva DCG, Longo GZ (2019) Visceral adiposity index is a better predictor of unhealthy metabolic phenotype than traditional adiposity measures: results from a population-based study. Public Health Nutr 22:1545–1554
Han Z, Guo X, Zhang B, Liao J, Nie L (2018) Blood lead levels of children in urban and suburban areas in China (1997–2015): Temporal and spatial variations and influencing factors. Sci Total Environ 625:1659–1666
Nguyen HD, Oh H, Jo WH, Hoang NHM, Kim MS (2022) Mixtures modeling identifies heavy metals and pyrethroid insecticide metabolites associated with obesity. Environ Sci Pollut Res Int 29:20379–20397
Wang N, Chen C, Nie X, Han B, Li Q, Chen Y, Zhu C, Chen Y, Xia F, Cang Z, Lu M, Meng Y, Zhai H, Lin D, Cui S, Jensen MD, Lu Y (2015) Blood lead level and its association with body mass index and obesity in China—results from SPECT-China study. Sci Rep 5:18299
Moon MK, Lee I, Lee A, Park H, Kim MJ, Kim S, Cho YH, Hong S, Yoo J, Cheon GJ, Choi K, Park YJ, Park J (2022) Lead, mercury, and cadmium exposures are associated with obesity but not with diabetes mellitus: Korean National Environmental Health Survey (KoNEHS) 2015–2017. Environ Res 204:111888
Scinicariello F, Buser MC, Mevissen M, Portier CJ (2013) Blood lead level association with lower body weight in NHANES 1999–2006. Toxicol Appl Pharmacol 273:516–523
Anonymous (2021) 8. Obesity management for the treatment of type 2 diabetes: standards of medical care in diabetes-2021. Diabetes Care 44:S100-s110
Wan H, Wang Y, Zhang H, Zhang K, Chen Y, Chen C, Zhang W, Xia F, Wang N, Lu Y (2022) Chronic lead exposure induces fatty liver disease associated with the variations of gut microbiota. Ecotoxicol Environ Saf 232:113257
Omidifar N, Nili-Ahmadabadi A, Nakhostin-Ansari A, Lankarani KB, Moghadami M, Mousavi SM, Hashemi SA, Gholami A, Shokripour M, Ebrahimi Z (2021) The modulatory potential of herbal antioxidants against oxidative stress and heavy metal pollution: plants against environmental oxidative stress. Environ Sci Pollut Res Int 28:61908–61918
D’Alessandro ME, Selenscig D, Illesca P, Chicco A, Lombardo YB (2015) Time course of adipose tissue dysfunction associated with antioxidant defense, inflammatory cytokines and oxidative stress in dyslipemic insulin resistant rats. Food Funct 6:1299–1309
Sun H, Wang N, Nie X, Zhao L, Li Q, Cang Z, Chen C, Lu M, Cheng J, Zhai H, Xia F, Ye L, Lu Y (2017) Lead exposure induces weight gain in adult rats, accompanied by dna hypermethylation. PLoS One 12:e0169958
Souza-Talarico JN, Suchecki D, Juster RP, Plusquellec P, Barbosa Junior F, Bunscheit V, Marcourakis T, de Matos TM, Lupien SJ (2017) Lead exposure is related to hypercortisolemic profiles and allostatic load in Brazilian older adults. Environ Res 154:261–268
Pasquali R (1998) Is the hypothalamic-pituitary-adrenal axis really hyperactivated in visceral obesity? J Endocrinol Invest 21:268–271
Li MM, Cao J, Xu J, Cai SZ, Shen XM, Yan CH (2014) The national trend of blood lead levels among Chinese children aged 0–18 years old, 1990–2012. Environ Int 71:109–117
Wiener RC, Bhandari R (2020) Association of electronic cigarette use with lead, cadmium, barium, and antimony body burden: NHANES 2015–2016. J Trace Elem Med Biol 62:126602
Shiek SS, Mani MS, Kabekkodu SP, Dsouza HS (2021) Health repercussions of environmental exposure to lead: methylation perspective. Toxicology 461:152927
Acknowledgements
The authors thank all research staff and participants in the METAL study.
Funding
This study was supported by the National Natural Science Foundation of China (82100846; 82170870; 82120108008), Shanghai Sailing Program (20YF1423500), Science and Technology Commission of Shanghai Municipality (19140902400), and Clinical Research Plan of SHDC (SHDC2020CR4006).
Author information
Authors and Affiliations
Contributions
Y.L., N.W., and H.Z. designed the study, contributed to the discussion, reviewed and edited the manuscript, and takes full responsibility for the work as a whole. C.C. designed the study, performed analysis, wrote the manuscript, and contributed to the discussion. C.C. and B.W. conducted the research, analyzed the data, and reviewed and edited the manuscript. H.Z., Y.W., S.Y., S.Z., Y.C., and F.X. conducted the research as well as contributed to the discussion.
Corresponding authors
Ethics declarations
Ethics Approval and Consent to Participate
Ethical approval was obtained from the Ethics Committee of Shanghai Ninth People’s Hospital, Shanghai Jiaotong University School of Medicine. All participants provided written informed consent at enrolment.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Ningjian Wang and Hualing Zhai are co-corresponding authors.
Yingli Lu (she should receive the proofs and will handle correspondence at all stages of refereeing and publication, also post-publication).
Rights and permissions
About this article
Cite this article
Chen, C., Wang, B., Zhang, H. et al. Blood Lead Level Is Associated with Visceral Adipose Dysfunction in Patients with Type 2 Diabetes. Biol Trace Elem Res 201, 2266–2273 (2023). https://doi.org/10.1007/s12011-022-03357-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-022-03357-6