Abstract
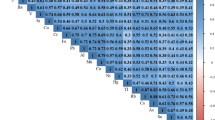
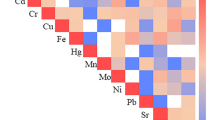
Hispanics/Latinos have higher rates of type 2 diabetes (T2D), and the origins of these disparities are poorly understood. Environmental endocrine-disrupting chemicals (EDCs), including some metals and metalloids, are implicated as diabetes risk factors. Data indicate that Hispanics/Latinos may be disproportionately exposed to EDCs, yet they remain understudied with respect to environmental exposures and diabetes. The objective of this study is to determine how metal exposures contribute to T2D progression by evaluating the associations between 8 urinary metals and measures of glycemic status in 414 normoglycemic or prediabetic adults living in Starr County, Texas, a Hispanic/Latino community with high rates of diabetes and diabetes-associated mortality. We used multivariable linear regression to quantify the differences in homeostatic model assessments for pancreatic β-cell function, insulin resistance, and insulin sensitivity (HOMA-β, HOMA-IR, HOMA-S, respectively), plasma insulin, plasma glucose, and hemoglobin A1c (HbA1c) associated with increasing urinary metal concentrations. Quantile-based g-computation was utilized to assess mixture effects. After multivariable adjustment, urinary arsenic and molybdenum were associated with lower HOMA-β, HOMA-IR, and plasma insulin levels and higher HOMA-S. Additionally, higher urinary copper levels were associated with a reduced HOMA-β. Lastly, a higher concentration of the 8 metal mixtures was associated with lower HOMA-β, HOMA-IR, and plasma insulin levels as well as higher HOMA-S. Our data indicate that arsenic, molybdenum, copper, and this metal mixture are associated with alterations in measures of glucose homeostasis among non-diabetics in Starr County. This study is one of the first to comprehensively evaluate associations of urinary metals with glycemic measures in a high-risk Mexican American population.
Similar content being viewed by others
References
Centers for Disease Control and Prevention (2020) National Diabetes Statistics Report, 2020. https://www.cdc.gov/diabetes/library/features/diabetes-stat-report.html
American Diabetes Association (2018) Economic Costs of Diabetes in the US in 2017. Diabetes Care 41(5):917–28. https://doi.org/10.2337/dci18-0007
Aguayo-Mazzucato C, Diaque P, Hernandez S, Rosas S, Kostic A, Caballero AE (2019) Understanding the growing epidemic of type 2 diabetes in the Hispanic population living in the United States. Diabetes Metab Res Rev 35(2):e3097. https://doi.org/10.1002/dmrr.3097
Hanis CL, Ferrell RE, Barton SA, Aguilar L, Garza-Ibarra A, Tulloch BR et al (1983) Diabetes among Mexican Americans in Starr County. Texas Am J Epidemiol 118(5):659–672. https://doi.org/10.1093/oxfordjournals.aje.a113677
Heindel JJ, Blumberg B, Cave M, Machtinger R, Mantovani A, Mendez MA et al (2017) Metabolism disrupting chemicals and metabolic disorders. Reprod Toxicol 68:3–33. https://doi.org/10.1016/j.reprotox.2016.10.001
Neel BA, Sargis RM (2011) The paradox of progress: environmental disruption of metabolism and the diabetes epidemic. Diabetes 60(7):1838–1848. https://doi.org/10.2337/db11-0153
Ruiz D, Becerra M, Jagai JS, Ard K, Sargis RM (2018) Disparities in environmental exposures to endocrine-disrupting chemicals and diabetes risk in vulnerable populations. Diabetes Care 41(1):193–205. https://doi.org/10.2337/dc16-2765
Menke A, Guallar E, Cowie CC (2016) Metals in urine and diabetes in US adults. Diabetes 65(1):164–71. https://doi.org/10.2337/db15-0316
Kazi TG, Afridi HI, Kazi N, Jamali MK, Arain MB, Jalbani N et al (2008) Copper, chromium, manganese, iron, nickel, and zinc levels in biological samples of diabetes mellitus patients. Biol Trace Elem Res 122(1):1–18. https://doi.org/10.1007/s12011-007-8062-y
Cruz KJC, de Oliveira ARS, Morais JBS, Severo JS, Mendes PMV, de Sousa Melo SR et al (2018) Zinc and insulin resistance: biochemical and molecular aspects. Biol Trace Elem Res 186(2):407–412. https://doi.org/10.1007/s12011-018-1308-z
Endocrine Society (2018) Endocrine-disrupting chemicals. An Endocrine Society Position Statement. https://www.endocrine.org/advocacy/position-statements/endocrine-disrupting-chemicals
Mimoto MS, Nadal A, Sargis RM (2017) Polluted pathways: mechanisms of metabolic disruption by endocrine disrupting chemicals. Curr Environ Health Rep 4(2):208–222. https://doi.org/10.1007/s40572-017-0137-0
Li XT, Yu PF, Gao Y, Guo WH, Wang J, Liu X et al (2017) Association between plasma metal levels and diabetes risk: a case-control study in China. Biomed Environ Sci 30(7):482–491. https://doi.org/10.3967/bes2017.064
Guo FF, Hu ZY, Li BY, Qin LQ, Fu C, Yu H et al (2019) Evaluation of the association between urinary cadmium levels below threshold limits and the risk of diabetes mellitus: a dose-response meta-analysis. Environ Sci Pollut Res Int 26(19):19272–19281. https://doi.org/10.1007/s11356-019-04943-3
Li Y, Zhang Y, Wang W, Wu Y (2017) Association of urinary cadmium with risk of diabetes: a meta-analysis. Environ Sci Pollut Res Int 24(11):10083–10090. https://doi.org/10.1007/s11356-017-8610-8
Feng W, Cui X, Liu B, Liu C, Xiao Y, Lu W et al (2015) Association of urinary metal profiles with altered glucose levels and diabetes risk: a population-based study in China. PLoS ONE 10(4):e0123742. https://doi.org/10.1371/journal.pone.0123742
Ettinger AS, Bovet P, Plange-Rhule J, Forrester TE, Lambert EV, Lupoli N et al (2014) Distribution of metals exposure and associations with cardiometabolic risk factors in the “Modeling the Epidemiologic Transition Study.” Environ Health 13:90. https://doi.org/10.1186/1476-069X-13-90
Laclaustra M, Navas-Acien A, Stranges S, Ordovas JM, Guallar E (2009) Serum selenium concentrations and diabetes in US adults: National Health and Nutrition Examination Survey (NHANES) 2003–2004. Environ Health Perspect 117(9):1409–13. https://doi.org/10.1289/ehp.0900704
Bleys J, Navas-Acien A, Guallar E (2007) Serum selenium and diabetes in U.S. adults. Diabetes Care 30(4):829–34. https://doi.org/10.2337/dc06-1726
Hanis CL, Redline S, Cade BE, Bell GI, Cox NJ, Below JE et al (2016) Beyond type 2 diabetes, obesity and hypertension: an axis including sleep apnea, left ventricular hypertrophy, endothelial dysfunction, and aortic stiffness among Mexican Americans in Starr County. Texas Cardiovasc Diabetol 15:86. https://doi.org/10.1186/s12933-016-0405-6
Jun G, Aguilar D, Evans C, Burant CF, Hanis CL (2020) Metabolomic profiles associated with subtypes of prediabetes among Mexican Americans in Starr County, Texas. USA Diabetologia 63(2):287–295. https://doi.org/10.1007/s00125-019-05031-4
Center for Disease Control and Prevention (2021) Hispanic/Latino Americans and Type 2 Diabetes. https://www.cdc.gov/diabetes/library/features/hispanic-diabetes.html
Brown EL, Essigmann HT, Hoffman KL, Palm NW, Gunter SM, Sederstrom JM, et al. (2020) Impact of Diabetes on the Gut and Salivary IgA Microbiomes. Infect Immun 88(12):e00301–20. https://doi.org/10.1128/IAI.00301-20.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28(7):412–419. https://doi.org/10.1007/BF00280883
Agency for Toxic Substances and Disease Registry (ATSDR) (2007) Toxicological profile for Arsenic. Atlanta, GA: U.S. Department of Health and Human Services, Public Health Service. https://www.atsdr.cdc.gov/toxprofiles/tp2.pdf
Agency for Toxic Substances and Disease Registry (ATSDR) (2005) Toxicological profile for Tin and Tin Compounds. Atlanta, GA: U.S. Department of Health and Human Services, Public Health Service. https://www.atsdr.cdc.gov/toxprofiles/tp55.pdf
Agency for Toxic Substances and Disease Registry (ATSDR) (2004) Toxicological profile for Copper. Atlanta, GA: U.S. Department of Health and Human Services, Public Health Service. https://www.atsdr.cdc.gov/toxprofiles/tp132.pdf
Agency for Toxic Substances and Disease Registry (ATSDR) (2020) Toxicological profile for Molybdenum. Atlanta, GA: U.S. Department of Health and Human Services, Public Health Service. https://www.atsdr.cdc.gov/toxprofiles/tp212.pdf
Agency for Toxic Substances and Disease Registry (ATSDR) (2005) Toxicological profile for Nickel. Atlanta, GA: U.S. Department of Health and Human Services, Public Health Service
Agency for Toxic Substances and Disease Registry (ATSDR) (2003) Toxicological profile for Selenium. Atlanta, GA: U.S. Department of Health and Human Services, Public Health Service. https://www.atsdr.cdc.gov/ToxProfiles/tp92.pdf
Li S, Wang J, Zhang B, Liu Y, Lu T, Shi Y et al (2018) Urinary Lead Concentration Is an Independent Predictor of Cancer Mortality in the U.S General Population. Front Oncol 8:242. https://doi.org/10.3389/fonc.2018.00242
Brookhart MA, Sturmer T, Glynn RJ, Rassen J, Schneeweiss S (2010) Confounding control in healthcare database research: challenges and potential approaches. Med Care 48(6 Suppl):S114–S120. https://doi.org/10.1097/MLR.0b013e3181dbebe3
Krishnakumar PK, Qurban MA, Stiboller M, Nachman KE, Joydas TV, Manikandan KP et al (2016) Arsenic and arsenic species in shellfish and finfish from the western Arabian Gulf and consumer health risk assessment. Sci Total Environ 566–567:1235–1244. https://doi.org/10.1016/j.scitotenv.2016.05.180
Keil AP, Buckley JP, O’Brien KM, Ferguson KK, Zhao S, White AJ (2020) A Quantile-Based g-Computation Approach to Addressing the Effects of Exposure Mixtures. Environ Health Perspect 128(4):47004. https://doi.org/10.1289/EHP5838
Thomas DJ, Styblo M, Lin S (2001) The cellular metabolism and systemic toxicity of arsenic. Toxicol Appl Pharmacol 176(2):127–144. https://doi.org/10.1006/taap.2001.9258
National Research Council (US) (1999) Subcommittee on Arsenic in Drinking Water. Arsenic in Drinking Water. Washington (DC): National Academies Press (US). Available from: https://www.ncbi.nlm.nih.gov/books/NBK230893/. https://doi.org/10.17226/6444
Ryker S (2001) Mapping arsenic in groundwater -- A real need, but a hard problem. Geotimes Newsmagazine Earth Sci p. 34–6. http://www.agiweb.org/geotimes/nov01/feature_Asmap.html
Gilbert-Diamond D, Cottingham KL, Gruber JF, Punshon T, Sayarath V, Gandolfi AJ et al (2011) Rice consumption contributes to arsenic exposure in US women. Proc Natl Acad Sci U S A 108(51):20656–20660. https://doi.org/10.1073/pnas.1109127108
Del Razo LM, Garcia-Vargas GG, Valenzuela OL, Castellanos EH, Sanchez-Pena LC, Currier JM et al (2011) Exposure to arsenic in drinking water is associated with increased prevalence of diabetes: a cross-sectional study in the Zimapan and Lagunera regions in Mexico. Environ Health 10:73. https://doi.org/10.1186/1476-069X-10-73
Tseng CH, Tai TY, Chong CK, Tseng CP, Lai MS, Lin BJ et al (2000) Long-term arsenic exposure and incidence of non-insulin-dependent diabetes mellitus: a cohort study in arseniasis-hyperendemic villages in Taiwan. Environ Health Perspect 108(9):847–851. https://doi.org/10.1289/ehp.00108847
Sung TC, Huang JW, Guo HR (2015) Association between Arsenic Exposure and Diabetes: A Meta-Analysis. Biomed Res Int 2015:368087. https://doi.org/10.1155/2015/368087
Navas-Acien A, Silbergeld EK, Streeter RA, Clark JM, Burke TA, Guallar E (2006) Arsenic exposure and type 2 diabetes: a systematic review of the experimental and epidemiological evidence. Environ Health Perspect 114(5):641–648. https://doi.org/10.1289/ehp.8551
Dover EN, Patel NY, Styblo M (2018) Impact of in vitro heavy metal exposure on pancreatic beta-cell function. Toxicol Lett 299:137–144. https://doi.org/10.1016/j.toxlet.2018.09.015
Liu S, Guo X, Wu B, Yu H, Zhang X, Li M (2014) Arsenic induces diabetic effects through beta-cell dysfunction and increased gluconeogenesis in mice. Sci Rep 4:6894. https://doi.org/10.1038/srep06894
Kirkley AG, Carmean CM, Ruiz D, Ye H, Regnier SM, Poudel A et al (2018) Arsenic exposure induces glucose intolerance and alters global energy metabolism. Am J Physiol Regul Integr Comp Physiol 314(2):R294–R303. https://doi.org/10.1152/ajpregu.00522.2016
Sargis RM (2014) The hijacking of cellular signaling and the diabetes epidemic: mechanisms of environmental disruption of insulin action and glucose homeostasis. Diabetes Metab J 38(1):13–24. https://doi.org/10.4093/dmj.2014.38.1.13
Momcilovic B (1999) A case report of acute human molybdenum toxicity from a dietary molybdenum supplement–a new member of the “Lucor metallicum” family. Arh Hig Rada Toksikol 50(3):289–297
Scott R, Eugenia GS, Melanie AWB, Sara ED, Thomas EG, Keith HP (2020) Spatial and temporal patterns of heavy metal deposition resulting from a smelter in El Paso. Texas Journal of Geochemical Exploration 210:106414. https://doi.org/10.1016/j.gexplo.2019.106414
Bulka CM, Daviglus ML, Persky VW, Durazo-Arvizu RA, Aviles-Santa ML, Gallo LC et al (2017) Occupational Exposures and Metabolic Syndrome Among Hispanics/Latinos: Cross-Sectional Results From the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). J Occup Environ Med 59(11):1047–1055. https://doi.org/10.1097/JOM.0000000000001115
Wang X, Mukherjee B, Karvonen-Gutierrez CA, Herman WH, Batterman S, Harlow SD et al (2020) Urinary metal mixtures and longitudinal changes in glucose homeostasis: The Study of Women’s Health Across the Nation (SWAN). Environ Int 145:106109. https://doi.org/10.1016/j.envint.2020.106109
Xiao L, Zhou Y, Ma J, Sun W, Cao L, Wang B et al (2018) Oxidative DNA damage mediates the association between urinary metals and prevalence of type 2 diabetes mellitus in Chinese adults. Sci Total Environ 627:1327–1333. https://doi.org/10.1016/j.scitotenv.2018.01.317
Yang TY, Yen CC, Lee KI, Su CC, Yang CY, Wu CC et al (2016) Molybdenum induces pancreatic beta-cell dysfunction and apoptosis via interdependent of JNK and AMPK activation-regulated mitochondria-dependent and ER stress-triggered pathways. Toxicol Appl Pharmacol 294:54–64. https://doi.org/10.1016/j.taap.2016.01.013
Domingo-Relloso A, Grau-Perez M, Galan-Chilet I, Garrido-Martinez MJ, Tormos C, Navas-Acien A et al (2019) Urinary metals and metal mixtures and oxidative stress biomarkers in an adult population from Spain: The Hortega Study. Environ Int 123:171–180. https://doi.org/10.1016/j.envint.2018.11.055
Robertson RP, Harmon J, Tran PO, Tanaka Y, Takahashi H (2003) Glucose toxicity in beta-cells: type 2 diabetes, good radicals gone bad, and the glutathione connection. Diabetes 52(3):581–587. https://doi.org/10.2337/diabetes.52.3.581
Mendy A, Gasana J, Vieira ER (2012) Urinary heavy metals and associated medical conditions in the US adult population. Int J Environ Health Res 22(2):105–118. https://doi.org/10.1080/09603123.2011.605877
Meeker JD, Rossano MG, Protas B, Padmanahban V, Diamond MP, Puscheck E et al (2010) Environmental exposure to metals and male reproductive hormones: circulating testosterone is inversely associated with blood molybdenum. Fertil Steril 93(1):130–140. https://doi.org/10.1016/j.fertnstert.2008.09.044
Shiue I, Hristova K (2014) Higher urinary heavy metal, phthalate and arsenic concentrations accounted for 3–19% of the population attributable risk for high blood pressure: US NHANES, 2009–2012. Hypertens Res 37(12):1075–1081. https://doi.org/10.1038/hr.2014.121
Taylor AA, Tsuji JS, Garry MR, McArdle ME, Goodfellow WL Jr, Adams WJ et al (2020) Critical Review of Exposure and Effects: Implications for Setting Regulatory Health Criteria for Ingested Copper. Environ Manage 65(1):131–159. https://doi.org/10.1007/s00267-019-01234-y
Qiu Q, Zhang F, Zhu W, Wu J, Liang M (2017) Copper in Diabetes Mellitus: a Meta-Analysis and Systematic Review of Plasma and Serum Studies. Biol Trace Elem Res 177(1):53–63. https://doi.org/10.1007/s12011-016-0877-y
Sobczak AIS, Stefanowicz F, Pitt SJ, Ajjan RA, Stewart AJ (2019) Total plasma magnesium, zinc, copper and selenium concentrations in type-I and type-II diabetes. Biometals 32(1):123–138. https://doi.org/10.1007/s10534-018-00167-z
Bjorklund G, Dadar M, Pivina L, Dosa MD, Semenova Y, Aaseth J (2020) The Role of Zinc and Copper in Insulin Resistance and Diabetes Mellitus. Curr Med Chem 27(39):6643–6657. https://doi.org/10.2174/0929867326666190902122155
Lowe J, Taveira-da-Silva R, Hilario-Souza E (2017) Dissecting copper homeostasis in diabetes mellitus. IUBMB Life 69(4):255–262. https://doi.org/10.1002/iub.1614
Cooper GJ (2011) Therapeutic potential of copper chelation with triethylenetetramine in managing diabetes mellitus and Alzheimer’s disease. Drugs 71(10):1281–1320. https://doi.org/10.2165/11591370-000000000-00000
Tinkov AA, Filippini T, Ajsuvakova OP, Aaseth J, Gluhcheva YG, Ivanova JM et al (2017) The role of cadmium in obesity and diabetes. Sci Total Environ 601–602:741–755. https://doi.org/10.1016/j.scitotenv.2017.05.224
Edwards J, Ackerman C (2016) A Review of Diabetes Mellitus and Exposure to the Environmental Toxicant Cadmium with an Emphasis on Likely Mechanisms of Action. Curr Diabetes Rev 12(3):252–258. https://doi.org/10.2174/1573399811666150812142922
RafatiRahimzadeh M, RafatiRahimzadeh M, Kazemi S, Moghadamnia AA (2017) Cadmium toxicity and treatment: An update. Caspian J Intern Med 8(3):135–45. https://doi.org/10.22088/cjim.8.3.135
Wu M, Song J, Zhu C, Wang Y, Yin X, Huang G et al (2017) Association between cadmium exposure and diabetes mellitus risk: a prisma-compliant systematic review and meta-analysis. Oncotarget 8(68):113129–41
Kuo CC, Moon K, Thayer KA, Navas-Acien A (2013) Environmental chemicals and type 2 diabetes: an updated systematic review of the epidemiologic evidence. Curr Diab Rep 13(6):831–849. https://doi.org/10.1007/s11892-013-0432-6
Wang X, Karvonen-Gutierrez CA, Herman WH, Mukherjee B, Harlow SD, Park SK (2020) Urinary metals and incident diabetes in midlife women: Study of Women's Health Across the Nation (SWAN). BMJ Open Diab Res Care 8(1):e001233. https://doi.org/10.1136/bmjdrc-2020-001233
Pokorska-Niewiada K, Brodowska A, Szczuko M (2021) The Content of Minerals in the PCOS Group and the Correlation with the Parameters of Metabolism. Nutrients 13(7): 2214. https://doi.org/10.3390/nu13072214
Lunyera J, Smith SR (2017) Heavy metal nephropathy: considerations for exposure analysis. Kidney Int 92(3):548–550. https://doi.org/10.1016/j.kint.2017.04.043
Kang ES, Yun YS, Park SW, Kim HJ, Ahn CW, Song YD et al (2005) Limitation of the validity of the homeostasis model assessment as an index of insulin resistance in Korea. Metabolism 54(2):206–211. https://doi.org/10.1016/j.metabol.2004.08.014
Funding
This work was supported by the National Institutes of Health (R01 ES028879 and R21 ES030884 supporting RMS; P30 ES027792 supporting MA and RMS; UL1 TR002003 supporting MA and RMS via the UIC Center for Clinical and Translational Science; University of Illinois at Chicago’s Medical-Scientist Training Program T32 GM079086 supporting MS; and R01 DK116378 supporting DA and CLH). The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
RMS declares he has received honoraria from CVS/Health and the American Medical Forum, neither of which relate to the present study.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Weiss, M.C., Shih, YH., Bryan, M.S. et al. Relationships Between Urinary Metals and Diabetes Traits Among Mexican Americans in Starr County, Texas, USA. Biol Trace Elem Res 201, 529–538 (2023). https://doi.org/10.1007/s12011-022-03165-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-022-03165-y