Abstract
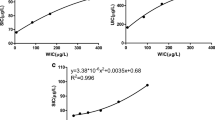
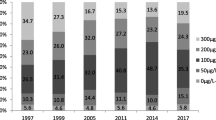
The aim of this study was to assess the population’s iodine nutrition and thyroid diseases in different water iodine areas and to offer suggestions to the governments of different countries to adjust the present policy in different water iodine areas. A cross-sectional survey was conducted in different water iodine areas in China. Urinary iodine, water iodine, salt iodine and thyroid function were determined. The thyroid volumes and nodules were measured by ultrasound. Upon categorization by water iodine level for the 10.0 ~ 39.9 μg/L, 40.0 ~ 100.0 μg/L and 100.1 ~ 150.0 μg/L areas, in adults, the prevalence of subclinical hypothyroidism was 9.28%, 5.35% and 11.07%, and the median urinary iodine (MUI) was 153.7 μg/L, 189.8 μg/L and 317.0 μg/L; in children of the three areas, the prevalence of goitre was 3.83%, 4.47% and 16.02%, and the MUI was 164.1 μg/L, 221.0 μg/L and 323.3 μg/L; in pregnant women of those areas, the MUI was 148.6 μg/L, 176.9 μg/L and 324.9 μg/L. Logistic regression results indicated that low iodine intake was a risk factor for developing hypothyroxinaemia in pregnant women. The iodine status of pregnant women is insufficient in areas with a median water iodine level of 10.0 ~ 39.9 μg/L. Low iodine intake increases the risk of developing hypothyroxinaemia in pregnant women. The iodine status of adults and children is excessive, and the iodine status of pregnant women is above the requirements in areas with a median water iodine concentration of 100.1 ~ 150.0 μg/L. Iodized salt, especially for pregnant women, should be supplied in areas with a median water iodine concentration of 10.0 ~ 39.9 μg/L to improve the iodine status of pregnant women. Supplying non-iodized salt is not enough to protect local residents from the harm from excess iodine in areas with a median water iodine concentration above 100.0 μg/L.



Similar content being viewed by others
Data Availability
The datasets generated during the current study are not publicly available due to privacy considerations but are available from the corresponding author on reasonable request.
References
Zimmermann MB (2009) Iodine deficiency. Endocr Rev 30:376–408. https://doi.org/10.1210/er.2009-0011
Zimmermann MB, Boelaert K (2015) Iodine deficiency and thyroid disorders. Lancet Diabetes Endocrinol 3:286–295. https://doi.org/10.1016/S2213-8587(14)70225-6
Koukkou EG, Roupas ND, Markou KB (2017) Effect of excess iodine intake on thyroid on human health. Minerva Med 108:136–146. https://doi.org/10.23736/S0026-4806.17.04923-0
Sang Z, Chen W, Shen J, Tan L, Zhao N, Liu H, Wen S, Wei W, Zhang G, Zhang W (2013) Long-term exposure to excessive iodine from water is associated with thyroid dysfunction in children. J Nutr 143:2038–2043. https://doi.org/10.3945/jn.113.179135
Teng W, Shan Z, Teng X, Guan H, Li Y, Teng D, Jin Y, Yu X, Fan C, Chong W, Yang F, Dai H, Yu Y, Li J, Chen Y, Zhao D, Shi X, Hu F, Mao J, Gu X, Yang R, Tong Y, Wang W, Gao T, Li C (2006) Effect of iodine intake on thyroid diseases in China. N Engl J Med 354:2783–2793. https://doi.org/10.1056/NEJMoa054022
Zimmermann MB, Andersson M (2021) GLOBAL ENDOCRINOLOGY: Global perspectives in endocrinology: coverage of iodized salt programs and iodine status in 2020. Eur J Endocrinol 185:R13–R21. https://doi.org/10.1530/EJE-21-0171
Zava TT, Zava DT (2011) Assessment of Japanese iodine intake based on seaweed consumption in Japan: a literature-based analysis. Thyroid Res 4:14. https://doi.org/10.1186/1756-6614-4-14
Kang MJ, Hwang IT, Chung HR (2018) Excessive iodine intake and subclinical hypothyroidism in children and adolescents aged 6–19 years: results of the Sixth Korean National Health and Nutrition Examination Survey, 2013–2015. Thyroid 28:773–779. https://doi.org/10.1089/thy.2017.0507
Shen H, Liu S, Sun D, Zhang S, Su X, Shen Y, Han H (2011) Geographical distribution of drinking-water with high iodine level and association between high iodine level in drinking-water and goitre: a Chinese national investigation. Br J Nutr 106:243–247. https://doi.org/10.1017/S0007114511000055
Farebrother J, Zimmermann MB, Abdallah F, Assey V, Fingerhut R, Gichohi-Wainaina WN, Hussein I, Makokha A, Sagno K, Untoro J, Watts M, Andersson M (2018) Effect of excess iodine intake from iodized salt and/or groundwater iodine on thyroid function in nonpregnant and pregnant women, infants, and children: a multicenter study in East Africa. Thyroid 28:1198–1210. https://doi.org/10.1089/thy.2018.0234
National Health Commission of the People’s Republic of China (2019) Report of national iodine content in drinking water survey. Available at: http://www.nhc.gov.cn/jkj/s5874/201905/bb1da1f5e47040e8820b9378e6db4bd3.shtml. Accessed 2021/07/12
Jia Q, Zhang X, Shen H, Guo X, Bian J, Wang P, Zheng H, Li S, Chen Z, Ma J (2016) Definition and demarcation of water-borne iodine-excess areas and iodine-excess endemial areas (GB/T 19380–2016), National Health and Family Planning Commission Standardization Administration, Beijing. (In Chinese)
Shen H, Liu P, Jia Q, Li W, Jiang W, Ma J, Zheng H, Wang P, Du Y, Fan L (2020) Definition and demarcation of iodine deficient areas and iodine adequate areas (WS/T 669–2020), National Health Commission of the People’s Republic of China. (In Chinese)
World Health Organization, UNICEF, ICCIDD (2007) Assessment of iodine deficiency disorders and monitoring their elimination: a guide for programme managers. WHO, Geneva
Jin Y, E X, Chen Y, Zhang L, Chen C, Chen S, Xing D, Wang Z, Wei J, Yang Y (2006) Standard exanination methods for drinking water-Nonmetal parameters(GB/T5750.5–2006), Beijing, China: People’s Medical Publishing House. (In Chinese)
Yan Y, Zhang Y, Liu L, Liu J, Li W, Hua J, Chen Z (2006) Method for determination of iodine in urine by As 3+-Ce 4+ catalytic spectrophotometry (WS/T 107–2006). China Criteria Publishing House, Beijing (In Chinese)
Chinese Society of Endocrinology, Chinese Society of Perinatology (2019) Guideline on Diagnosis and Management of Thyroid Diseases during Pregnancy and Postpartum (2nd edition). Chin J Perinat Med 22:505–539 (In Chinese)
Weetman AP (2004) Autoimmune Thyroid Disease. Autoimmunity 37:337–340
Liu S, Chen Z, Jia Q, Su X, Zhang S (2007) Diagnostic criterion of endemic goiter (WS 276–2007). People’s Medical Publishing House, Beijing (In Chinese)
Tan L, Sang Z, Shen J, Liu H, Chen W, Zhao N, Wei W, Zhang G, Zhang W (2015) Prevalence of thyroid dysfunction with adequate and excessive iodine intake in Hebei Province, People’s Republic of China. Public Health Nutr 18:1692–1697. https://doi.org/10.1017/S1368980014002237
Teng X, Shan Z, Chen Y, Lai Y, Yu J, Shan L, Bai X, Li Y, Li N, Li Z, Wang S, Xing Q, Xue H, Zhu L, Hou X, Fan C, Teng W (2011) More than adequate iodine intake may increase subclinical hypothyroidism and autoimmune thyroiditis: a cross-sectional study based on two Chinese communities with different iodine intake levels. Eur J Endocrinol 164:943–950. https://doi.org/10.1530/EJE-10-1041
Camargo RY, Tomimori EK, Neves SC, Rubio IGS, Galrão AL, Knobel M, Medeiros-Neto G (2008) Thyroid and the environment: exposure to excessive nutritional iodine increases the prevalence of thyroid disorders in Sao Paulo, Brazil. Eur J Endocrinol 159(293):299. https://doi.org/10.1530/EJE-08-0192
Duntas LH (2015) The role of iodine and selenium in autoimmune thyroiditis. Horm Metab Res 47:721–726. https://doi.org/10.1055/s-0035-1559631
Luo Y, Kawashima A, Ishido Y, Yoshihara A, Oda K, Hiroi N, Ito T, Ishii N, Suzuki K (2014) Iodine excess as an environmental risk factor for autoimmune thyroid disease. Int J Mol Sci 15:12895–12912. https://doi.org/10.3390/ijms150712895
Du Y, Gao Y, Meng F, Liu S, Fan Z, Wu J, Sun D (2014) Iodine deficiency and excess coexist in china and induce thyroid dysfunction and disease: a cross-sectional study. PLoS ONE 9:e111937. https://doi.org/10.1371/journal.pone.0111937
Chen W, Li X, Wu Y, Bian J, Shen J, Jiang W, Tan L, Wang X, Wang W, Pearce EN, Zimmermann MB, Carriquiry AL, Zhang W (2017) Associations between iodine intake, thyroid volume, and goiter rate in school-aged Chinese children from areas with high iodine drinking water concentrations. Am J Clin Nutr 105:228–233. https://doi.org/10.3945/ajcn.116.139725
Cui SL, Liu P, Su XH, Liu ShJ (2017) Surveys in areas of high risk of iodine deficiency and iodine excess in China, 2012–2014: current status and examination of the relationship between urinary iodine concentration and goiter prevalence in children aged 8–10 years. Biomed Environ Sci 30:88–96. https://doi.org/10.3967/bes2017.012
Lv S, Zhao J, Xu D, Chong Z, Jia L, Du Y, Ma J, Rutherford S (2012) An epidemiological survey of children’s iodine nutrition and goitre status in regions with mildly excessive iodine in drinking water in Hebei Province, China. Public Health Nutr 15:1168–1173. https://doi.org/10.1017/S1368980012000146
Murcia M, Espada M, Julvez J, Llop S, Lopez-Espinosa MJ, Vioque J, Basterrechea M, Riaño I, González L, Alvarez-Pedrerol M, Tardón A, Ibarluzea J, Rebagliato M (2018) Iodine intake from supplements and diet during pregnancy and child cognitive and motor development: the INMA Mother and Child Cohort Study. J Epidemiol Community Health 72:216–222. https://doi.org/10.1136/jech-2017-209830
Wang Y, Han J, Chen X, Zeng X, Wang Y, Dong J, Chen J (2018) Maternal iodine supplementation improves motor coordination in offspring by modulating the mGluR1 signaling pathway in mild iodine deficiency-induced hypothyroxinemia rats. J Nutr Biochem 58:80–89. https://doi.org/10.1016/j.jnutbio.2018.04.012
Wei W, Wang Y, Dong J, Wang Y, Min H, Song B, Shan Z, Teng W, Xi Q, Chen J (2013) Hypothyroxinemia induced by mild iodine deficiency deregulats thyroid proteins during gestation and lactation in dams. Int J Environ Res Public Health 10:3233–3245. https://doi.org/10.3390/ijerph10083233
Gowachirapant S, Melse-Boonstra A, Winichagoon P, Zimmermann MB (2014) Overweight increases risk of first trimester hypothyroxinaemia in iodine-deficient pregnant women. Matern Child Nutr 10:61–71. https://doi.org/10.1111/mcn.12040
Min H, Dong J, Wang Y, Wang Y, Teng W, Xi Q, Chen J (2016) Maternal hypothyroxinemia-induced neurodevelopmental impairments in the progeny. Mol Neurobiol 53:1613–1624. https://doi.org/10.1007/s12035-015-9101-x
Pop VJ, Kuijpens JL, van Baar AL, Verkerk G, van Son MM, de Vijlder JJ, Vulsma T, Wiersinga WM, Drexhage HA, Vader HL (1999) Low maternal free thyroxine concentrations during early pregnancy are associated with impaired psychomotor development in infancy. Clin Endocrinol (Oxf) 50:149–155. https://doi.org/10.1046/j.1365-2265.1999.00639.x
Su X, Zhao Y, Cao Z, Yang Y, Duan T, Hua J (2019) Association between isolated hypothyroxinaemia in early pregnancy and perinatal outcomes. Endocr Connect 8:435–441. https://doi.org/10.1530/EC-19-0088
Acknowledgements
We thank all the organizations that participated in this survey: the provincial Centers for Disease Control (CDC) and the Centers for Endemic Disease Control in Shanxi, Anhui, Shandong, Hebei, Henan and Jiangsu and the residents who participated in this survey.
Funding
This study was supported by grants from the National Natural Science Foundation of China (81830098).
Author information
Authors and Affiliations
Contributions
Shen H. and Liu P. contributed to the study’s conception and design. Material preparation and data collection were performed by Meng F., Fan L., Jia Q., Li W., Jiang W., Ma J., Zheng H., Wang P. and Sun D. Data analysis and the first draft of the manuscript was written by Du Y. Previous versions of the manuscript were commented by Liu P. and Shen H.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
Research approval was obtained from the Ethics Committee of Harbin Medical University. The study was performed in accordance with the Declaration of Helsinki. All participants consent to participate in this study.
Research Involving Human Participants and/or Animals
This study involved human participants.
Informed Consent
Written informed consent was obtained from the adult participants or the guardians on behalf of the participating children prior to the survey.
Consent for Publication
All authors consent for publication.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Du, Y., Liu, P., Meng, F. et al. What Iodine Intervention Measures Should Be Taken in Different Water Iodine Areas? Evidence from a Cross-sectional Chinese Survey. Biol Trace Elem Res 200, 4654–4663 (2022). https://doi.org/10.1007/s12011-021-03050-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-021-03050-0