Abstract
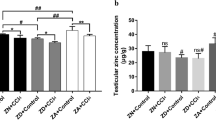
Marginal zinc deficiency is more common than severe zinc deficiency, and the effect of marginal zinc deficiency on male reproduction is unknown. This study investigated the effect of marginal zinc deficiency on spermatogenesis and its mechanism. Male ICR mice were fed normal zinc (30 mg/kg) and marginal zinc deficiency (10 mg/kg) diets for 35 days. Zinc-dependent proteins and enzymes were measured as biomarkers of zinc levels in the body. Metallothionein and Cu–Zn SOD levels in the control group were higher than those in the marginal zinc deficiency group. Hematoxylin and eosin staining showed that the marginal zinc deficiency diet caused histopathological changes in the testis and destruction of the sperm head under scanning electron microscopy. Sperm parameters and sex hormone levels were also affected by marginal zinc deficiency. In addition, marginal zinc deficiency led to alter expression level of several important spermatogenesis-related genes in the epididymis and testes. These results indicate that although zinc intake in marginal zinc deficiency is close to the recommended reference value, low zinc intake interferes with the expression of genes related to spermatogenesis and may lead to sperm abnormalities in mice.







Similar content being viewed by others
References
Vickram S et al (2021) Role of zinc (Zn) in human reproduction: a journey from initial spermatogenesis to childbirth. International Journal of Molecular Sciences 22(4):2188. https://doi.org/10.3390/ijms22042188
Prasad AS (2009) Zinc: role in immunity, oxidative stress and chronic inflammation. Curr Opin Clin Nutr Metab Care 12(6):646–652. https://doi.org/10.1097/MCO.0b013e3283312956
Kerns K, Zigo M, Sutovsky P (2018) Zinc: a necessary ion for mammalian sperm fertilization competency. International Journal of Molecular Sciences 19(12):4097. https://doi.org/10.3390/ijms19124097
Beigi Harchegani A et al (2020) Effects of zinc deficiency on impaired spermatogenesis and male infertility: the role of oxidative stress, inflammation and apoptosis. Hum Fertil (Camb) 23(1):5–16. https://doi.org/10.1080/14647273.2018.1494390
Jinno N, Nagata M, Takahashi T (2014) Marginal zinc deficiency negatively affects recovery from muscle injury in mice. Biol Trace Elem Res 158(1):65–72. https://doi.org/10.1007/s12011-014-9901-2
Rahali D et al. (2020) Spermatogenesis and steroidogenesis disruption in a model of metabolic syndrome rats. Arch Physiol Biochem, 1–11. https://doi.org/10.1080/13813455.2020.1812665
Razavi S et al (2019) Effect of zinc on spermatogenesis and sperm chromatin condensation in bleomycin, etoposide, cisplatin treated rats. Cell Journal 20(4):521–526. https://doi.org/10.22074/cellj.2019.5522
Oliva R (2006) Protamines and male infertility. Hum Reprod Update 12(4):417–435. https://doi.org/10.1093/humupd/dml009
Oghbaei H et al (2020) Effects of bacteria on male fertility: spermatogenesis and sperm function. Life Sci 256:117891. https://doi.org/10.1016/j.lfs.2020.117891
Baltaci AK, Mogulkoc R, Baltaci SB (2019) The role of zinc in the endocrine system. Pak J Pharm Sci 32(1):231–239
Liu DY et al (2009) Relationship between seminal plasma zinc concentration and spermatozoa-zona pellucida binding and the ZP-induced acrosome reaction in subfertile men. Asian J Androl 11(4):499–507. https://doi.org/10.1038/aja.2009.23
Xie J et al (2020) Low dose lead exposure at the onset of puberty disrupts spermatogenesis-related gene expression and causes abnormal spermatogenesis in mouse. Toxicology and Applied Pharmacology 393:114942. https://doi.org/10.1016/j.taap.2020.114942
Morgan A et al (2019) Next-generation sequencing identified SPATC1L as a possible candidate gene for both early-onset and age-related hearing loss. Eur J Hum Genet 27(1):70–79. https://doi.org/10.1038/s41431-018-0229-9
Kim J et al (2018) SPATC1L maintains the integrity of the sperm head-tail junction. EMBO Rep 19(9):e45991. https://doi.org/10.15252/embr.201845991
Yuan S et al (2015) Spata6 is required for normal assembly of the sperm connecting piece and tight head-tail conjunction. Proc Natl Acad Sci U S A 112(5):E430–E439. https://doi.org/10.1073/pnas.1424648112
Li W et al (2016) Dissecting the structural basis of MEIG1 interaction with PACRG. Sci Rep 6:18278. https://doi.org/10.1038/srep18278
Shen YR et al (2020) The SEPT12 complex is required for the establishment of a functional sperm head-tail junction. Mol Hum Reprod 26(6):402–412. https://doi.org/10.1093/molehr/gaaa031
Selvaraj V et al (2010) Mice lacking FABP9/PERF15 develop sperm head abnormalities but are fertile. Dev Biol 348(2):177–189. https://doi.org/10.1016/j.ydbio.2010.09.019
Gao Q et al (2014) Association of TNP2 gene polymorphisms of the bta-miR-154 target site with the semen quality traits of Chinese Holstein bulls. Plos One 9(1):e84355. https://doi.org/10.1371/journal.pone.0084355
Teves ME et al (2013) Germ cell-specific disruption of the Meig1 gene causes impaired spermiogenesis in mice. Andrology 1(1):37–46. https://doi.org/10.1111/j.2047-2927.2012.00001.x
Iwaya H et al (2011) Marginal zinc deficiency exacerbates experimental colitis induced by dextran sulfate sodium in rats. J Nutr 141(6):1077–1082. https://doi.org/10.3945/jn.111.138180
Croxford TP, McCormick NH, Kelleher SL (2011) Moderate zinc deficiency reduces testicular Zip6 and Zip10 abundance and impairs spermatogenesis in mice. J Nutr 141(3):359–365. https://doi.org/10.3945/jn.110.131318
Adamo AM et al (2019) Early developmental marginal zinc deficiency affects neurogenesis decreasing neuronal number and altering neuronal specification in the adult rat brain. Frontiers in Cellular Neuroscience 13:62. https://doi.org/10.3389/fncel.2019.00062
Gaulke CA et al (2018) Marginal zinc deficiency and environmentally relevant concentrations of arsenic elicit combined effects on the gut microbiome. Msphere 3(6):e00521-e618. https://doi.org/10.1128/mSphere.00521-18
Yokokawa H et al (2020) Serum zinc concentrations and characteristics of zinc deficiency/marginal deficiency among Japanese subjects. J Gen and Fam Med 21(6):248–255. https://doi.org/10.1002/jgf2.377
Huang YL et al (2016) Nutritional marginal zinc deficiency disrupts placental 11 beta-hydroxysteroid dehydrogenase type 2 modulation. Food Funct 7(1):84–92. https://doi.org/10.1039/c5fo01203a
Nuttall JR et al (2015) Gestational marginal zinc deficiency impaired fetal neural progenitor cell proliferation by disrupting the ERK1/2 signaling pathway. J Nutr Biochem 26(11):1116–1123. https://doi.org/10.1016/j.jnutbio.2015.05.007
McCormick NH et al (2015) Redistribution of tissue zinc pools during lactation and dyshomeostasis during marginal zinc deficiency in mice. J Trace Elem Med Biol 29:170–175. https://doi.org/10.1016/j.jtemb.2014.06.002
Paik HY et al (1999) Serum extracellular superoxide dismutase activity as an indicator of zinc status in humans. Biol Trace Elem Res 69(1):45–57. https://doi.org/10.1007/Bf02783914
DiSilvestro RA, Dardenne M, Joseph E (2020) Comparison of thymulin activity with other measures of marginal zinc deficiency. Biol Trace Elem Res 199(2):585–587. https://doi.org/10.1007/s12011-020-02159-y
Yazgan B et al (2020) Effects of zinc supplementation on metallothionein levels in ischemic renal tissue. Biotechnic & Histochemistry. 95(4):285–296. https://doi.org/10.1080/10520295.2019.1691264
Dimitrova AA et al (2008) Zinc content in the diet affects the activity of Cu/ZnSOD, lipid peroxidation and lipid profile of spontaneously hypertensive rats. Acta Biol Hung 59(3):305–314. https://doi.org/10.1556/ABiol.59.2008.3.4
Sun JY et al (2006) Effect of zinc on biochemical parameters and changes in related gene expression assessed by cDNA microarrays in pituitary of growing rats. Nutrition 22(2):187–196. https://doi.org/10.1016/j.nut.2005.07.007
Justus J, Weigand E (2014) The effect of a moderate zinc deficiency and dietary fat source on the activity and expression of the Delta(3)Delta (2)-enoyl-CoA isomerase in the liver of growing rats. Biol Trace Elem Res 158(3):365–375. https://doi.org/10.1007/s12011-014-9940-8
Mahfouz RZ et al (2010) Sperm viability, apoptosis, and intracellular reactive oxygen species levels in human spermatozoa before and after induction of oxidative stress. Fertil Steril 93(3):814–821. https://doi.org/10.1016/j.fertnstert.2008.10.068
Lambard S et al (2004) Analysis and significance of mRNA in human ejaculated sperm from normozoospermic donors: relationship to sperm motility and capacitation. Mol Hum Reprod 10(7):535–541. https://doi.org/10.1093/molehr/gah064
Bucar S et al (2015) DNA fragmentation in human sperm after magnetic-activated cell sorting. J Assist Reprod Genet 32(1):147–154. https://doi.org/10.1007/s10815-014-0370-5
Chu QQ et al (2016) A potential role for zinc transporter 7 in testosterone synthesis in mouse Leydig tumor cells. Int J Mol Med 37(6):1619–1626. https://doi.org/10.3892/ijmm.2016.2576
Saleem TH et al (2021) Biochemical assessments of seminal plasma zinc, testis-expressed sequence 101 and free amino acids and their correlations with reproductive hormones in male infertility. Biol Trace Elem Res 199(5):1729–1742. https://doi.org/10.1007/s12011-020-02310-9
Kothari RP, Chaudhari AR (2016) Zinc levels in seminal fluid in infertile males and its relation with serum free testosterone. J Clin Diagn Res 10(5):Cc5–Cc8. https://doi.org/10.7860/Jcdr/2016/14393.7723
Hamdi SA, Nassif OI, Ardawi MSM (1997) Effect of marginal or severe dietary zinc deficiency on testicular development and functions of the rat. Arch Androl 38(3):243–253. https://doi.org/10.3109/01485019708994883
Salzberg Y et al (2010) Meig1 deficiency causes a severe defect in mouse spermatogenesis. Dev Biol 338(2):158–167. https://doi.org/10.1016/j.ydbio.2009.11.028
Zhang Z et al (2009) MEIG1 is essential for spermiogenesis in mice. Proc Natl Acad Sci U S A 106(40):17055–17060. https://doi.org/10.1073/pnas.0906414106
Yamada Y et al (2017) Identification of EGFLAM, SPATC1L and RNASE13 as novel susceptibility loci for aortic aneurysm in Japanese individuals by exome-wide association studies. Int J Mol Med 39(5):1091–1100. https://doi.org/10.3892/ijmm.2017.2927
Yamada Y et al (2017) Identification of TNFSF13, SPATC1L, SLC22A25 and SALL4 as novel susceptibility loci for atrial fibrillation by an exomewide association study. Mol Med Rep 16(5):5823–5832. https://doi.org/10.3892/mmr.2017.7334
Oh C et al (2003) Characterization, expression pattern and chromosomal localization of the spermatogenesis associated 6 gene (Spata6). Mol Hum Reprod 9(6):321–330. https://doi.org/10.1093/molehr/gag047
Savadi-Shiraz E et al (2015) Quantification of sperm specific mRNA transcripts (PRM1, PRM2, and TNP2) in teratozoospermia and normozoospermia: new correlations between mRNA content and morphology of sperm. Mol Reprod Dev 82(1):26–35. https://doi.org/10.1002/mrd.22440
Yu ZR, Raabe T, Hecht NB (2005) MicroRNA Mirn122a reduces expression of the posttranscriptionally regulated germ cell transition protein 2 (Tnp2) messenger RNA (mRNA) by mRNA cleavage. Biol Reprod 73(3):427–433. https://doi.org/10.1095/biolreprod.105.040998
Adham IM et al (2001) Teratozoospermia in mice lacking the transition protein 2 (Tnp2). Mol Hum Reprod 7(6):513–520. https://doi.org/10.1093/molehr/7.6.513
Geng D et al (2019) Association of single nucleotide polymorphism c.673C>A/p.Gln225Lys in SEPT12 gene with spermatogenesis failure in male idiopathic infertility in Northeast China. J Int Med Res. 47(2):992–998. https://doi.org/10.1177/0300060518811770
Lai TH et al (2016) SEPT12-NDC1 complexes are required for mammalian spermiogenesis. Int J Mol Sci 17(11):1911. https://doi.org/10.3390/ijms17111911
Lin CH et al (2019) Regulation of septin phosphorylation: SEPT12 phosphorylation in sperm septin assembly. Cytoskeleton (Hoboken) 76(1):137–142. https://doi.org/10.1002/cm.21491
Yeh CH et al (2015) SEPT12/SPAG4/LAMINB1 complexes are required for maintaining the integrity of the nuclear envelope in postmeiotic male germ cells. PLoS ONE 10(3):e0120722. https://doi.org/10.1371/journal.pone.0120722
Karanth S et al (2008) The evolutionary relationship between the duplicated copies of the zebrafish fabp11 gene and the tetrapod FABP4, FABP5, FABP8 and FABP9 genes. FEBS J 275(12):3031–3040. https://doi.org/10.1111/j.1742-4658.2008.06455.x
Dacheux JL, Dacheux F (2014) New insights into epididymal function in relation to sperm maturation. Reproduction 147(2):R27–R42. https://doi.org/10.1530/Rep-13-0420
Aziz N et al (2007) The relationship between human sperm apoptosis, morphology and the sperm deformity index. Hum Reprod 22(5):1413–1419. https://doi.org/10.1093/humrep/dem016
Allen-Redpath K et al (2013) Marginal dietary zinc deficiency in vivo induces vascular smooth muscle cell apoptosis in large arteries. Cardiovasc Res 99(3):525–534. https://doi.org/10.1093/cvr/cvt114
Acknowledgements
Thanks to all members of Professor Wang CH’s lab at the School of Health Sciences, Wuhan University for their generous help. We would like to thank Ms. Hui Liang from the School of Basic Medicine, Wuhan University for her professional support in the use of the scanning electron microscope. At the same time, thanks to the animal facilities of Wuhan University Animal Experiment Center for the maintenance of the mouse population.
Funding
This study was supported by grants from Angel Nutritech Nutrition Fund (Grant NO. AF2019004).
Author information
Authors and Affiliations
Contributions
Chunhong Wang and Cheng Peng designed this study. Ziqiong Wang, Duanya Liu, Haitao Ma, and Lei Wang raised the animals. Cheng Peng and Zhaoyu Zhang carried out index detection and wrote the first draft. Chunhong Wang, Qian Cheng, and Youjiao Liu edited the final paper. All authors approved the final version.
Corresponding author
Ethics declarations
Ethics Approval
This study was approved by the Committee of the Ethics of Animal Experiments of the Wuhan University School of Medicine (No.: WP2020-08053).
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Data Repositories
All data presented in the main manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Peng, C., Cheng, Q., Liu, Y. et al. Marginal Zinc Deficiency in Mice Increased the Number of Abnormal Sperm and Altered the Expression Level of Spermatogenesis-Related Genes. Biol Trace Elem Res 200, 3738–3749 (2022). https://doi.org/10.1007/s12011-021-02979-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-021-02979-6