Abstract
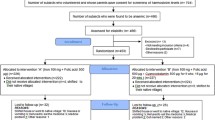
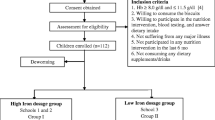
This study was carried out to assess the efficacy of sodium iron EDTA (NaFeEDTA) salt-enriched fish powder in addressing iron deficiency in adolescent anaemic girls. This was a 60-day randomised double-blinded, controlled intervention trial involving 123 girls age ranging from 10 to 19 years in three villages of West Jaintia Hills District of State of Meghalaya in India using soup made out of sodium iron EDTA (NaFeEDTA)-enriched fish powder (250 mg/100 g). The influence of the iron-enriched powder on blood haemoglobin levels and serum iron was determined. The research also analysed the food consumed by the study subjects during the study period and it was found that there were no significant differences between the iron-enriched and control groups. The results indicated that the girls predominantly consumed cereals with little fruits, vegetables and meat. On an average, 100 ml of soup prepared out of 10 g of fish powder per day was consumed that theoretically provided about 25 mg of iron each day. Following intervention, all the participants in the group that consumed soup made out of NaFeEDTA-enriched fish powder had significantly higher haemoglobin levels and serum iron and a lower prevalence of anaemia than the control group. The effects of NaFeEDTA salt-enriched fish powder were statistically significant and it can be inferred that NaFeEDTA-enriched fish powder was highly effective in controlling iron deficiency and reducing the prevalence of iron-deficiency anaemia among the adolescent girls.


Similar content being viewed by others
Data availability (Data Transparency)
All data generated in the study can be made available when required.
Code Availability (Software Application or Custom Code)
Not applicable.
References
de Benoist B, McLean E, Egli I, Cogswell M (2008) Worldwide prevalence of anemia 1993–2005: WHO global database on anemia. WHO, Geneva. https://doi.org/10.1017/S1368980008002401
World Health Organization, Regional Office for South-East Asia (2007) Adolescent health – India factsheet. In: Adolescent health at a glance in South – East Asia Region. New Delhi: WHO/SEARO. https://apps.who.int/iris/handle/10665/204750. Accessed 12 Jan 2021
Kumar A (1999) National nutritional anemia control programme in India. Indian J Public Health 43(3–5):16
Horton SRJ, Ross J (2003) The economics of iron deficiency. Food Policy 28:51–75. https://doi.org/10.1016/S0306-9192(02)00070-2
WHO, UNICEF, UNU (2001) Iron deficiency anemia: assessment, prevention and control, a guide for programme managers. Geneva, World Health Organization, http://www.who.int/nutrition/publications/micronutrients/anaemia_iron_deficiency/WHO_NHD_01.3/en/index.html. Accessed 23 Jan 2021
National Health Mission (2017) Technical handbook on anemia in adolescents https://www.nhm.gov.in/images/pdf/programmes/wifs/guidelines/technical_handbook_on_anaemia.pdf. Accessed 20 Jan 2021
Kotecha PV (2011) Nutritional anemia in young children with focus on Asia and India. Indian J of Community Med: Official publication of Indian Association of Preventive & Social Medicine 36:8–16. https://doi.org/10.4103/0970-0218.80786
Diseases and Injuries Collaborators (2019) Global burden of 369 diseases and injuries, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet. https://doi.org/10.1016/S0140-6736(20)30925-9
Institute for Health Metrics and Evaluation (2018) Findings from the Global Burden of Disease Study 2017. Seattle, WA.
Jelena R, Ksenija S (2018) Iron deficiency anemia in children. In: Jesmine Khan, (ed) Current topics in anemia, Intech Open. https://doi.org/10.5772/intechopen.69774
Tanu A, Manju R, Pragya S, Gopal KI (2014) Issues in prevention of iron deficiency anemia in India. Nutrition 30:764–770. https://doi.org/10.1016/j.nut.2013.11.022
Chandrakumari AS, Sinha P, Singaravelu S, Jaikumar S (2019) Prevalence of anemia among adolescent girls in a rural area of Tamil Nadu, India. Journal of Family Medicine and Primary Care 8:1414–1417. https://doi.org/10.4103/jfmpc.jfmpc_140_19
Madhusnata D, Ajanta H, Sandeep P, Rinini D, Shila C, Bani S, Tulika C, Urmisha D, Geeta T (2006) Anemia and hemoglobinopathies in tribal population of Eastern and North-eastern India. Hematology 11:371–373. https://doi.org/10.1080/10245330600840180
Elvina SM, Namita S (2018) Prevalence of anaemia and nutritional knowledge among tribal women of reproductive age group of Meghalaya, India. Int. J. Curr. Microbiol. App. Sci 7:1221–1229. https://doi.org/10.20546/ijcmas.2018.710.136
Gera T, Sachdev HS, Boy E (2012) Effect of iron-fortified foods on hematologic and biological outcomes: systematic review of randomized controlled trials. Am J Clin Nutr 96:309–324. https://doi.org/10.3945/ajcn.111.031500
Idjradinata P, Pollitt E (1993) Reversal of developmental delays in iron-deficient anemic infants treated with iron. Lancet 341:1–4. https://doi.org/10.1016/0140-6736(93)92477-b
Sachdev H, Gera T, Nestel P (2005) Effect of iron supplementation on mental and motor development in children: systematic review of randomized controlled trials. Public Health Nutr 8:117–132. https://doi.org/10.1079/phn2004677
Davidsson L, Almgren A, Hurrell RF (1998) Sodium iron EDTA [NaFe(III)EDTA] as a food fortificant does not influence absorption and urinary excretion of manganese in healthy adults. J Nutr 128:1139–1143. https://doi.org/10.1093/jn/128.7.1139
Davidsson L, Ziegler E, Zeder C, Walczyk T, Hurrell R (2005) Sodium iron EDTA [NaFe(III)EDTA] as a food fortificant: erythrocyte incorporation of iron and apparent absorption of zinc, copper, calcium, and magnesium from a complementary food based on wheat and soy in healthy infants. Am J Clin Nutr 81:104–109. https://doi.org/10.1093/ajcn/81.1.104
Munro IC (1994) Sodium iron EDTA, CanTox Inc., Mississauga, Canada. http://www.inchem.org/documents/jecfa/jecmono/v32je14.htm. Accessed 14 Jan 2021
EFSA panel on food additives and nutrient sources added to food (ANS), (2010) Scientific opinion on the use of ferric sodium EDTA as a source of iron added for nutritional purposes to foods for the general population (including food supplements) and to foods for particular nutritional uses. EFSA J 8:1414–1446. https://doi.org/10.2903/j.efsa.2010.1414
ICMR-NIN (2020) Recommended dietary allowances and estimated average requirements nutrient requirements for Indians - 2020 A Report of the Expert Group Indian Council of Medical Research-National Institute of Nutrition, Hyderabad https://foodfuturefoundation.org/media/i0ld30zx/recommended-dietary-allowances-RDA-for-indians-2020.pdf. Accessed 14 Jan 2021
FAO/WHO (2000) Evaluation of certain food additives and contaminants. Fifty-third report of the Joint FAO/WHO Expert Committee on Food Additives. Geneva, World Health Organization (WHO Technical Series No. 896). https://apps.who.int/iris/handle/10665/42378. Accessed 14 Jan 2021
Longvah T, Ananthan R, Bhaskarachary K, Venkaiah K (2017) Indian Food Composition Tables. Publisher, National Institute of Nutrition, Hyderabad
Cook JD (1985) Measurement of iron status. A report of the International Nutritional Anaemia Consultative Group (INACG). New York: Washington DC; Ch.II: pp 4
Poitevin E (2012) Determination of calcium, copper, iron, magnesium, manganese, potassium, phosphorus, sodium, and zinc in fortified food products by microwave digestion and inductively coupled plasma-optical emission spectrometry: single-laboratory validation and ring trial. J AOAC Int 95:177–185. https://doi.org/10.5740/jaoacint.CS2011_14
Recommended daily allowance (2020) Food Safety and Standards Authority of India, https://www.fssai.gov.in/upload/advisories/2020/01/5e159e0a809bbLetter_RDA_08_01_2020.pdf. Accessed 20 Jan 2021
Hashim N, Farooqi M, Naqvi S, Jaffery HF (2014) Anemia-moderate to severe during pregnancy. Professional Med J 21:247–252
Alleyne M, Horne MK, Miller JL (2008) Individualized treatment for iron-deficiency anemia in adults. Am J Med 121:943–948. https://doi.org/10.1016/j.amjmed.2008.07.012
Heimbach J, Rieth S, Mohamedshah F, Slesinski R, Samuel-Fernando P, Sheehan T, Dickmann R, Borzelleca J (2000) Safety assessment of iron EDTA [sodium iron (Fe (3+)) ethylenediaminetetraacetic acid]: summary of toxicological, fortification and exposure data. Food Chem Toxicol 38:99–111. https://doi.org/10.1016/s0278-6915(99)00125-8
Acknowledgements
The authors are indebted to ICDS, West Jaintia Hills District, Meghalaya, and Child Development Project Office, Thadlaskein Block, West Jaintia Hills District, Meghalaya, for the support rendered in conduct of the intervention trials. The support provided by the technical staff at Biochemistry and Nutrition Division of ICAR-CIFT is thankfully acknowledged. This work was undertaken as part of the ongoing ICARC-GIAR W3 collaboration in India between ICAR-CIFT, Cochin, and WorldFish, Malaysia.
Funding
The work was supported by funding from the Institute where the authors currently work.
Author information
Authors and Affiliations
Contributions
KKA was involved in the design and conduct of the study and prepared the manuscript. SM and PMM were involved in the design and conduct of the study. RCN critically reviewed the manuscript. All authors approved the final version of the manuscript to be submitted.
Corresponding author
Ethics declarations
Ethical Approval
The study was approved by the Institutional Research Review Committee and the Institute Project Evaluation and Monitoring Cell. It is also certified that the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki.
Consent to Participate
Informed consent was obtained from all individual participants included in the study and their legal guardians.
Consent to Publish
The authors affirm that the participants provided informed consent for publication of the study findings.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
•Fish powder, a rather unconventional source for iron enrichment, has been used as a vehicle to deliver iron to anaemic adolescent girls in our study.
•Sodium iron EDTA, a globally accepted source of iron, has been used as the fortificant to enrich fish powder with iron for the first time.
•Following intake of iron-enriched fish powder for 60 days, a significant decrease in prevalence of anaemia and increase in haemoglobin levels were observed among the participants of the study.
•About 53% of adolescent girls have been resolved of anaemia following the intervention with fish powder enriched with sodium iron EDTA.
Rights and permissions
About this article
Cite this article
Kunnath, A.K., Mathew, S., Mothadaka, M.P. et al. Iron-Enriched Fish Powder Improved Haemoglobin Levels in Adolescent Girls of West Jaintia Hills District of Meghalaya, India. Biol Trace Elem Res 200, 2017–2024 (2022). https://doi.org/10.1007/s12011-021-02820-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-021-02820-0