Abstract
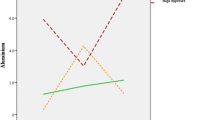
Cigarette smoking appears to have adverse effects of male reproductivity. The interplay between zinc and cadmium presumably plays a role in mediating toxic effects of smoking. This work was conducted to study serum and seminal plasma zinc and cadmium level in smokers compared to non-smokers. Seventy males were included: 35 smokers (group I) (smoking ˃20 cigarettes/day with mild smoking index <400) and 35 age-matched non-smokers (group II). Semen analysis was performed according to the WHO laboratory manual 2010. Atomic absorption spectrophotometer was used to detect zinc and cadmium amounts in both blood plasma and semen of any groups. Smoker group showed significantly lower sperm density, motility (P=0.001), and sperm viability (P=0.002) and higher abnormally formed sperms. Seminal zinc level was significantly lower in smokers (P=0.038).There was significant negative correlation between seminal zinc and smoking index and significant positive correlation between seminal zinc levels and sperm motility (P=0.008) and viability percentage (P=0.001). Seminal cadmium level was significantly higher in smoker (P=0.022). Significant positive correlation between seminal cadmium and both age and smoking index (P=0.003) and significant negative correlation between seminal cadmium and sperm density (P=0.005), motility (P=0.047), and viability (P=0.039). Seminal zinc level was negatively correlated to seminal cadmium level (P=0.020). Smoking has deleterious effects on semen quality hence fertility through several toxicants and chemicals. Reduced zinc levels and elevated cadmium levels were evident in smokers which have significant role in the adverse effects on the semen parameters.
Similar content being viewed by others
Data availability
Data supporting our study results are accessible from the relevant author whenever needed.
References
Eggert-Kruse W, Zwick E-M, Batschulat K, Rohr G, Armbruster FP, Petzoldt D, Strowitzki T (2002) Are zinc levels in seminal plasma associated with seminal leukocytes and other determinants of semen quality? Fertil Steril 77(2):260–269
Kumosani T, Elshal MF, Al-Jonaid A, Abduljabar H (2008) The influence of smoking on semen quality, seminal microelements and Ca2+-ATPase activity among infertile and fertile men. Clin Biochem 41(14-15):1199–1203
Jahantigh D, Colagar AH, Salimi S (2017) Genetic polymorphisms and haplotypes of the DJ-1 gene promoter associated with the susceptibility to male infertility. J Assist Reprod Genet 34(12):1673–1682
Josarayi GA, Mohammad-Hasani A, Aftabi Y, Moudi E, Colagar AH (2017) The AhRR-c. 565C> G transversion may increase total antioxidant capacity levels of the seminal plasma in infertile men. Environ Sci Pollut Res 24(21):17428–17435
Clemens S, Aarts MG, Thomine S, Verbruggen N (2013) Plant science: the key to preventing slow cadmium poisoning. Trends Plant Sci 18(2):92–99
Ranganathan P, Rao KA, Sudan JJ, Balasundaram S (2018) Cadmium effects on sperm morphology and semenogelin with relates to increased ROS in infertile smokers: an in vitro and in silico approach. Reprod Biol 18(2):189–197
Benoff S, Jacob A, Hurley IR (2000) Male infertility and environmental exposure to lead and cadmium. Hum Reprod Update 6(2):107–121
Pant N, Kumar G, Upadhyay A, Gupta Y, Chaturvedi P (2015) Correlation between lead and cadmium concentration and semen quality. Andrologia 47(8):887–891
WHO (2010) laboratory manual for the examination and processing of human semen- 5th edn
Liu R, Gao J, Zhang H, Wang R, Zhang Z, Liu X (2010) Seminal plasma zinc level may be associated with the effect of cigarette smoking on sperm parameters. J Int Med Res 38(3):923–928
Colagar AH, Jorsaraee G, Marzony ET (2007) Cigarette smoking and the risk of male infertility. Pakistan journal of biological sciences: PJBS 10(21):3870–3874
Yardimci S, Atan A, Delibasi T, Sunguroglu K, Güven M (1997) Long-term effects of cigarette-smoke exposure on plasma testosterone, luteinizing hormone and follicle-stimulating hormone levels in male rats. Br J Urol 79(1):66–69
Miyaji K, Kaneko S, Ishikawa H, Aoyagi T, Hayakawa K, Hata M, Oohashi M, Izawa A, Murai M (2001) Creatine kinase isoforms in the seminal plasma and the purified human sperm. Arch Androl 46(2):127–134
Morrow JD, Frei B, Longmire AW, Gaziano JM, Lynch SM, Shyr Y, Strauss WE, Oates JA, Roberts LJ (1995) Increase in circulating products of lipid peroxidation (F2-isoprostanes) in smokers—smoking as a cause of oxidative damage. N Engl J Med 332(18):1198–1203
Asare-Anane H, Bannison S, Ofori EK, Ateko R, Bawah A, Amanquah S, Oppong S, Gandau B, Ziem J (2016) Tobacco smoking is associated with decreased semen quality. Reprod Health 13(1):1–6
Kiziler AR, Aydemir B, Onaran I, Alici B, Ozkara H, Gulyasar T, Akyolcu MC (2007) High levels of cadmium and lead in seminal fluid and blood of smoking men are associated with high oxidative stress and damage in infertile subjects. Biol Trace Elem Res 120(1):82–91
Taha EA, Ez-Aldin AM, Sayed SK, Ghandour NM, Mostafa T (2012) Effect of smoking on sperm vitality, DNA integrity, seminal oxidative stress, zinc in fertile men. Urology 80(4):822–825
Subhani GM, Khan NI, Akmal M, Munir MI, Javed SH (2019) Correlation between semen zinc concentration and semen parameters of infertile men. Annals of Punjab Medical College 13(1):18–22
Telisman S, Cvitković P, Jurasović J, Pizent A, Gavella M, Rocić B (2000) Semen quality and reproductive endocrine function in relation to biomarkers of lead, cadmium, zinc, and copper in men. Environ Health Perspect 108(1):45–53
Mankad M, Sathawara N, Doshi H, Saiyed H, Kumar S (2006) Seminal plasma zinc concentration and α-glucosidase activity with respect to semen quality. Biol Trace Elem Res 110(2):97–106
Colagar AH, Marzony ET, Chaichi MJ (2009) Zinc levels in seminal plasma are associated with sperm quality in fertile and infertile men. Nutr Res 29(2):82–88
Hassan F, Xu X, Nuovo G, Killilea DW, Tyrrell J, Da Tan C, Tarran R, Diaz P, Jee J, Knoell D (2014) Accumulation of metals in GOLD4 COPD lungs is associated with decreased CFTR levels. Respir Res 15(1):1–9
Richter P, Faroon O, Pappas RS (2017) Cadmium and cadmium/zinc ratios and tobacco-related morbidities. Int J Environ Res Public Health 14(10):1154
Palaniappan U, Starkey LJ, O'Loughlin J, Gray-Donald K (2001) Fruit and vegetable consumption is lower and saturated fat intake is higher among Canadians reporting smoking. J Nutr 131(7):1952–1958
Yuyan L, Junqing W, Wei Y, Weijin Z, Ersheng G (2008) Are serum zinc and copper levels related to semen quality? Fertil Steril 89(4):1008–1011
Calderón B, Gómez-Martín JM, Cuadrado-Ayuso M, Cobeta P, Vega-Piñero B, Mateo R, Galindo J, Botella-Carretero JI (2020) Circulating zinc and copper levels are associated with sperm quality in obese men after metabolic surgery: a pilot study. Nutrients 12(11):3354
Saaranen M, Kantola M, Saarikoski S, Vanha-Perttula T (1989) Human seminal plasma cadmium: comparison with fertility and smoking habits/cadmium in menschlichem seminalplasma: Vergleich zwischen Fertilität und Rauchgewohnheiten. Andrologia 21(2):140–145
Oldereid N, Thomassen Y, Attramadal A, Olaisen B, Purvis K (1993) Concentrations of lead, cadmium and zinc in the tissues of reproductive organs of men. Reproduction 99(2):421–425
Saksena S, Dahlgren L, Lau I, Chang M (1977) Reproductive and endocrinological features of male rats after treatment with cadmium chloride. Biol Reprod 16(5):609–613
Oldereid N, Thomassen Y, Purvis K (1994) Seminal plasma lead, cadmium and zinc in relation to tobacco consumption. Int J Androl 17(1):24–28
Friberg L, Vahter M (1983) Assessment of exposure to lead and cadmium through biological monitoring: results of a UNEP/WHO global study. Environ Res 30(1):95–128
Senthil SL, Kumar TA, MarudhuPandi T, Dhaneesh K, Murugan JB, TBJWQ S, Exposure, Health (2012) Metal contagion in ecologically important estuary located in Bay of Bengal. Water Qual Expo Health 4(3):137–142
Kim H, Lee HJ, Hwang J-Y, Ha E-H, Park H, Ha M, Kim JH, Hong Y-C, Chang N (2010) Blood cadmium concentrations of male cigarette smokers are inversely associated with fruit consumption. J Nutr 140(6):1133–1138
Telisman S, Jurasovic J, Pizent A, Cvitkovic P (1998) Cadmium in the blood and seminal fluid of nonoccupationally exposed adult male subjects with regard to smoking habits. Occupational Health Industrial Medicine 1(38):48
Mendiola J, Moreno JM, Roca M, Vergara-Juárez N, Martínez-García MJ, García-Sánchez A, Elvira-Rendueles B, Moreno-Grau S, López-Espín JJ, Ten J (2011) Relationships between heavy metal concentrations in three different body fluids and male reproductive parameters: a pilot study. Environ Health Perspect 10(1):6
Taha EA, Sayed SK, Ghandour NM, Mahran AM, Saleh MA, Amin MM, Shamloul R (2013) Correlation between seminal lead and cadmium and seminal parameters in idiopathic oligoasthenozoospermic males. Central European journal of urology 66(1):84
Thompson J, Bannigan JJRt (2008) Cadmium: toxic effects on the reproductive system and embryo. Reprod Toxicol 25(3):304–15
Aoyagi T, Ishikawa H, Miyaji K, Hayakawa K, Hata M (2002) Cadmium-induced testicular damage in a rat model of subchronic intoxication. Reproductive medicine;biology 1(2):59–63
Amara S, Abdelmelek H, Garrel C, Guiraud P, Douki T, Ravanat J-L, Favier A, Sakly M, Rhouma KB (2008) Preventive effect of zinc against cadmium-induced oxidative stress in the rat testis. J Reprod Dev 54(2):129–134
Keck C, Bramkamp G, Behre HM, Müller C, Jockenhövel F, Nieschlag E (1995) Lack of correlation between cadmium in seminal plasma and fertility status of nonexposed individuals and two cadmium-exposed patients. Reprod Toxicol 9(1):35–40
Hovatta O, Venäläinen E-R, Kuusimäki L, Heikkilä J, Hirvi T, Reima I (1998) Aluminium, lead and cadmium concentrations in seminal plasma and spermatozoa, and semen quality in Finnish men. Hum Reprod 13(1):115–119
Omu AE, Dashti H, Mohamed AT, Mattappallil A (1995) Significance of trace elements in seminal plasma of infertile men. Nutr Res 11(5 Suppl):502–505
Chia S, Ong C, Lee S, Tsakok F (1992) Blood concentrations of lead, cadmium, mercury, zinc, and copper and human semen parameters. Arch Androl 29(2):177–183
Xu B, Chia S-E, Tsakok M, Ong C-N (1993) Trace elements in blood and seminal plasma and their relationship to sperm quality. Reprod Toxicol 7(6):613–618
Fallah A, Mohammad-Hasani A, Colagar AH (2018) Zinc is an essential element for male fertility: a review of Zn roles in men’s health, germination, sperm quality, and fertilization. J Reprod Infertil 19(2):96–81
Acknowledgements
We are tremendously grateful to all the healthy volunteers who participated in this study and all the research team.
Before obtaining samples, a written informed consent was received from all the subjects examined and this research was approved by the Local Ethics Committee of the Faculty of Medicine, Menoufia University; record number:19519DERM41, in alignment with the Helsinki Declaration (World Medical Assembly).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bazid, H.A.S., Attia, A.M., Yousef, A.M. et al. Evaluating the Serum and Seminal Plasma Levels of Zinc and Cadmium in Smokers and Their Relation to the Semen Parameters. Biol Trace Elem Res 200, 1002–1009 (2022). https://doi.org/10.1007/s12011-021-02720-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-021-02720-3