Abstract
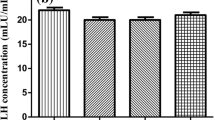
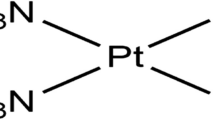
Selenium nanoparticles (SeNPs) and metformin (Met) elicit individually protective effects against testicular oxidative injury in diabetic rats. However, the combined effects of both compounds have not been investigated. We investigated the effects of SeNPs and Met individual/co-treatment on testicular oxidative injury in diabetic rats. Diabetes was induced by a single intraperitoneal administration of streptozotocin (STZ-40 mg/kg bwt). The rats were equally divided into 6 groups: Group one—non-diabetic; group two—diabetic untreated; and group six—non-diabetic received citrate buffer (2 mL/kg bwt), while group three, four, and five received SeNPs (0.1 mg/kg bwt), Met (50 mg/kg bwt), and SeNPs/Met combined respectively, for 42 days. Results revealed that SeNPs, as well as Met treatment significantly (p < 0.001), lowered blood glucose levels and improved relative organ weights in treated rats than those of the untreated group. Moreover, a synergistic effect was observed in the co-administration group. Additionally, combined treatment elicited better effect, in augmenting the pituitary and testicular hormone (LH, FSH, prolactin, and testosterone) levels, marker enzymes/protein associated with steroidogenesis (3-βHSD, 17-βHSD, and StAR protein), and sperm functional parameters than those of individual treatment groups, when compared with control. Furthermore, the combinatorial effects of SeNPs and Met surpassed their influence in attenuating testicular oxidative stress/inflammation and upregulation of Nrf2 protein expression in diabetic rats when compared with control. Overall, normal rats, co-treated with SeNPs and Met, did not reveal any deleterious effect. Therefore, SeNPs and Met combined treatment may better improve testes function in diabetic conditions than an individual regimen.








Similar content being viewed by others
References
Ebokaiwe AP, Ijomone OM, Osawe SO, Chukwu CJ, Ejike CECC, Zhang G, Wang F (2018) Alteration in sperm characteristics, endocrine balance and redox status in rats rendered diabetic by streptozotocin treatment: attenuating role of Loranthus micranthus. Redox Rep 23(1):194–205
Rato L, Alves G (2015) Testicular metabolic reprogramming in neonatal streptozotocin-induced type 2 diabetic rats impairs glycolytic flux and promotes glycogen synthesis. J Diabetes Res 9:73–142
Ma Q (2013) Role of Nrf2 in oxidative stress and toxicity. Annu Rev Pharmacol Toxicol 53:401–426
Muralidhara BS (2007) Early oxidative stress in testis and epididymal sperm in streptozotocin-induced diabetic mice: its progression and genotoxic consequences. Reprod Toxicol 23:578–587
Dkhil MD et al (2016) Selenium nanoparticles attenuate oxidative stress and testicular damage in streptozotocin-induced diabetic rats. Molecules 21:15–17
Griffin S et al (2018) Resuspendable powders of lyophilized chalcogen particles with activity against microorganisms. Antioxidants 7:23
Ebokaiwe AP et al (2019) Nanosized selenium and Loranthus micranthus leaves ameliorate streptozotocin-induced hepato-renal dysfunction in rats via enhancement of antioxidant system, regulation of caspase 3 and Nrf2 protein expression. Pharmanutrition. 9:100150
Hwang D, Seo S, Kim Y, Kim C, Shim S, Jee S, Lee S, Jang M, Kim M, Yim S, Lee SK, Kang B, Jang I, Cho J (2007) Selenium acts as an insulin-like molecule for the down-regulation of diabetic symptoms via endoplasmic reticulum stress and insulin signalling proteins in diabetes-induced non-obese diabetic mice. J Biosci 32:723–735
Al-Quraishy S et al (2015) Anti-hyperglycemic activity of selenium nanoparticles in streptozotocin-induced diabetic rats. Int J Nanomedicine 10:6741–6756
Meneses MJ et al (2015) The antidiabetic drug metformin and male reproductive function: an overview. Int J Diabetol Vasc Dis Res 3(1e):1–2
Tartarin P, Moison D, Guibert E, Dupont J, Habert R, Rouiller-Fabre V, Frydman N, Pozzi S, Frydman R, Lecureuil C, Froment P (2012) Metformin exposure affects human and mouse fetal testicular cells. Hum Reprod 27(11):3304–3314
Griffin S et al (2018) No time to waste organic waste: Nanosizing converts remains of food processing into refined materials. J Environ Manag 210:114–121
Misra HP, Fridovich I (1972) The role of superoxide anion in the autooxidation of epinephrine and a simple assay for superoxide dismutase. J Biol Chem 247:3170–3175
Clairborne A (1995) Catalase activity. In: Greewald AR (ed) Handbook of methods for oxygen radical research. CRC Press, Boca Raton, pp 237–242
Jollow DJ, Mitchell JR, Zampaglione N, Gillette JR (1974) Bromobenzene induced liver necrosis: protective role of glutathione and evidence for 3,4 bromobenzene oxide as the hepatotoxic metabolite. Pharmacology 11:151–169
Rotruck JT, Pope AL, Ganther HE, Swanson AB, Hafeman DG, Hoekstra WG (1973) Selenium: biochemical role as a component of glutathione peroxidase. Science 179:588–590
Habig WH, Pabst MJ, Jakoby WB (1974) Glutathione S-transferase. The first enzymatic step in mercapturic acid formation. J Biol Chem 249:7130–7139
Garcia YJ, Rodríguez-Malaver AJ, Peñaloza N (2005) Lipid peroxidation measurement by thiobarbituric acid assay in rat cerebellar slices. J Neurosci Methods 144(1):127–135
Eiserich JP, Hristova MCE (1998) Cross, formation of nitric oxide-derived inflammatory oxidants by myeloperoxidase in neu-trophils. Nature 391:393–397
Bergmeyer HU (1974) β-Hydroxysteroid dehydrogenase. In: Bergmeyer HU (ed) Methods of enzymatic analysis, vol 1. Academic, New York, pp 447–489
World Health Organization (2010) WHO laboratory manual for the examination and processing of human semen, 5th edn. World Health Organization, Geneva
Kim B (2017) Western blot techniques. Methods Mol Biol 1606:133–139
Adedara IA et al (2019) Dietary protocatechuic acid abrogates male reproductive dysfunction in streptozotocin induced diabetic rats via suppression of oxidative damage, inflammation and caspase-3 activity. Eur J Pharmacol 19:14–29
Schoeller EL, Albanna G, Frolova AI, Moley KH (2012) Insulin rescues impaired spermatogenesis via the hypothalamic–pituitary–gonadal axis in Akita diabetic mice and restores male fertility. Diabetes 61:1869–1878
Muthuvel R et al (2006) Antioxidant effect of ascorbic acid on PCB (Aroclor 1254) induced oxidative stress in hypothalamus of albino rats. Clin Chim Acta 365:297–303
Ramaswamy S, Weinbauer GF (2015) Endocrine control of spermatogenesis: role of FSH and LH/ testosterone. Spermatogenesis 4:996–1025
Cheng WH, Walker J (2005) FSH and testosterone signaling in Sertoli cells. Reproduction. 130:15–28
Nanjappa MK et al (2012) The industrial chemical bisphenol A (BPA) interferes with proliferative activity and development of steroidogenic capacity in rat Leydig cells. Biol Reprod 86:1–12
Oehninger S et al (2014) Sperm functional tests. Fertil Steril 102:1528–1533
Aitken RJ (2006) Sperm function tests and fertility. Int J Androl 29:69–75
Sharpe RM (1994) Regulation of spermatogenesis. In: Knobil E, Neill JD (eds) The physiology of reproduction. Raven Press, Ltd., New York, pp 1363–1434
Apichakan S et al (2019) Expression of testicular phosphorylated proteins in types 1 and 2 diabetes mellitus in mice: an experimental study. Int J Reprod BioMed 17:567–576
Acknowledgments
We thank Professor Cornelia M. Keck (Institute of Pharmaceutics and Biopharmaceutics, Philipps University of Marburg, 35037, Marburg, Germany), for giving us the opportunity to work in her laboratory for the nanoparticle production of selenium.
Funding
This research was supported by the TWAS-DFG 2017 cooperation visit grant awarded to Azubuike P. Ebokaiwe, and AE-FUNAI Institutional Based research grant Awarded to Azubuike P. Ebokaiwe with grant code FUNAI/FST/14/B2/022.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Male adult Wister rats (180 g ± 5 g) were nurtured at the Animal House, Alex Ekwueme Federal University, Ndufu-Alike Ikwo, Nigeria, and used for this study. Handling of animals was conducted with humane care according to the criteria outlined in the Guide for the Care and Use of Laboratory Animals as prepared by the US National Academy of Science (NAS) and published by the US National Institute of Health. Experiments were performed following the US NAS guidelines and with the approval of the relevant Institutional Committee.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ebokaiwe, A.P., Obeten, K.E., Okori, S.O. et al. Co-administration of Selenium Nanoparticles and Metformin Abrogate Testicular Oxidative Injury by Suppressing Redox Imbalance, Augmenting Sperm Quality and Nrf2 Protein Expression in Streptozotocin-Induced Diabetic Rats. Biol Trace Elem Res 198, 544–556 (2020). https://doi.org/10.1007/s12011-020-02082-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-020-02082-2