Abstract
The objective of the present study was to investigate the relationship between hair essential trace element and mineral content and ADHD in preschool (4–6 years old) and primary school children (6–10 years old) in relation to age and gender. Hair essential trace element and mineral content in 90 Russian children with ADHD and 90 age- and gender-matched neurotypical controls were assessed using inductively coupled plasma mass-spectrometry after microwave digestion. The obtained data demonstrate that hair Co, Cu, Mn, Si, and Zn contents in ADHD children was significantly reduced by 18%, 10%, 27%, 16%, and 19% as compared to the control values, respectively. The most significant decrease in children with ADHD was observed for hair Mg levels, being 29% lower than those in neurotypical children. After adjustment for age and gender, the observed difference in hair element content was more characteristic for preschool children and girls, respectively. Multiple linear regression analysis demonstrated that in a crude model (hair element levels as predictors), only hair Zn content was significantly inversely associated with ADHD (β = − 0.169; p = 0.025). Adjustment for anthropometric parameters (model 2) did not increase the predictive ability of the model, although it improved the association between hair Zn and ADHD in children (β = − 0.194; p = 0.014). Hypothetically, the observed alterations may at least partially contribute to neurobehavioral disturbances in children with ADHD. Moreover, the results of the present study raise the question about the potential benefits of Zn and Mg supplementation in children with ADHD. However, further detailed studies are required to investigate micronutrient deficiencies in ADHD.
Similar content being viewed by others
References
Epstein JN, Loren RE (2013) Changes in the definition of ADHD in DSM-5: subtle but important. Neuropsychiatry 3:455–458. https://doi.org/10.2217/npy.13.59
Hansen BH, Oerbeck B, Skirbekk B, Petrovski BÉ, Kristensen H (2018) Neurodevelopmental disorders: prevalence and comorbidity in children referred to mental health services. Nord J Psychiatry 72:285–291. https://doi.org/10.1080/08039488.2018.1444087
Sayal K, Prasad V, Daley D, Ford T, Coghill D (2018) ADHD in children and young people: prevalence, care pathways, and service provision. Lancet Psychiatry 5:175–186. https://doi.org/10.1016/S2215-0366(17)30167-0
Kotov AS, Borisova MN, Panteleeva MV, Matyuk YUV, Shatalin AV Attention deficit hyperactivity disorder. A clinical lecture. Rus J Child Neurol 2:54–58. https://doi.org/10.17650/2073-8803-2015-10-2-54-58
Russell AE, Ford T, Russell G (2015) Socioeconomic associations with ADHD: findings from a mediation analysis. PLoS One 10:e0128248. https://doi.org/10.1371/journal.pone.0128248
Faraone SV, Perlis RH, Doyle AE, Smoller JW, Goralnick J, Holmgren NA, Sklar P (2005) Molecular genetics of attention-deficit/hyperactivity disorder. Biol Psychiatry 57:1313–1323. https://doi.org/10.1016/j.biopsych.2004.11.024
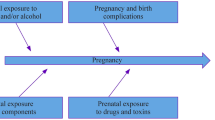
Sciberras E, Mulraney M, Silva D, Coghill D (2017) Prenatal risk factors and the etiology of ADHD—review of existing evidence. Curr Psychiatry Rep 19(1). https://doi.org/10.1007/s11920-017-0753-2
Halmøy A, Klungsøyr K, Skjærven R, Haavik J (2012) Pre- and perinatal risk factors in adults with attention-deficit/hyperactivity disorder. Biol Psychiatry 71:474–481. https://doi.org/10.1016/j.biopsych.2011.11.013
Sagiv SK, Epstein JN, Bellinger DC, Korrick SA (2013) Pre- and postnatal risk factors for ADHD in a nonclinical pediatric population. J Atten Disord 17:47–57. https://doi.org/10.1177/1087054711427563
Kern JK, Geier DA, Sykes LK, Geier MR, Deth RC (2015) Are ASD and ADHD a continuum? A comparison of pathophysiological similarities between the disorders. J Atten Disord 19:805–827. https://doi.org/10.1177/1087054712459886
Anjos T, Altmäe S, Emmett P et al (2013) Nutrition and neurodevelopment in children: focus on NUTRIMENTHE project. Eur J Nutr 52:1825–1842. https://doi.org/10.1007/s00394-013-0560-4
Woo H, Kim D, Hong YS, Kim YM, Seo JH, Choe B, Park JH, Kang J-W, Yoo J-H, Chueh HW, Lee JH, Kwak MJ, Kim J (2014) Dietary patterns in children with attention deficit/hyperactivity disorder (ADHD). Nutrients 6:1539–1553. https://doi.org/10.3390/nu6041539
Elbaz F, Zahra S, Hanafy H (2017) Magnesium, zinc and copper estimation in children with attention deficit hyperactivity disorder (ADHD). Egypt J Med Hum Genet 18:153–163. https://doi.org/10.1016/j.ejmhg.2016.04.009
Russo AJ (2010) Decreased serum Cu/Zn SOD associated with high copper in children with attention deficit hyperactivity disorder (ADHD). J Centr Nerv Syst Dis 2. https://doi.org/10.4137/JCNSD.S4553
Yang R, Zhang Y, Gao W, Lin N, Li R, Zhao Z (2019) Blood levels of trace elements in children with attention-deficit hyperactivity disorder: results from a case-control study. Biol Trace Elem Res 187:376–382. https://doi.org/10.1007/s12011-018-1408-9
Kul M, Kara M, Unal F, Tuzun Z, Akbiyik F (2014) Serum copper and ceruloplasmin levels in children and adolescents with attention deficit hyperactivity disorder. Klinik Psikofarmakol Bülteni 24:139–145. https://doi.org/10.5455/bcp.20130614050435
Donfrancesco R, Parisi P, Vanacore N, Martines F, Sargentini V, Cortese S (2013) Iron and ADHD: time to move beyond serum ferritin levels. J Atten Disord 17:347–357. https://doi.org/10.1177/1087054711430712
Konikowska K, Regulska-Ilow B, Rozanska D (2012) The influence of components of diet on the symptoms of ADHD in children. Rocz Panstw Zakl Hig 63:127–134
Verlaet AA, Noriega DB, Hermans N, Savelkoul HF (2014) Nutrition, immunological mechanisms and dietary immunomodulation in ADHD. Eur Child Adolesc Psychiatry 23:519–529. https://doi.org/10.1007/s00787-014-0522-2
Hariri M, Azadbakht L (2015) Magnesium, iron, and zinc supplementation for the treatment of attention deficit hyperactivity disorder: a systematic review on the recent literature. Int J Prev Med 6:83. https://doi.org/10.4103/2008-7802.164313
Kosanovic M, Jokanovic M (2011) Quantitative analysis of toxic and essential elements in human hair. Clinical validity of results. Environ Monit Assess 174:635–643. https://doi.org/10.1007/s10661-010-1484-6
Chojnacka K, Zielińska A, Górecka H, Dobrzański Z, Górecki H (2010) Reference values for hair minerals of Polish students. Environ Toxicol Pharmacol 29:314–319. https://doi.org/10.1016/j.etap.2010.03.010
Chojnacka K, Mikulewicz M (2012) Hair mineral analysis in the assessment of human exposure to metals. In: Reddy VR (ed) Handbook of hair in health and disease. Wageningen Academic Publishers, Wageningen, pp 278–292. https://doi.org/10.3920/978-90-8686-728-8_14
Viktorinova A, Ursinyova M, Trebaticka J, Uhnakova I, Durackova Z, Masanova V (2016) Changed plasma levels of zinc and copper to zinc ratio and their possible associations with parent-and teacher-rated symptoms in children with attention-deficit hyperactivity disorder. Biol Trace Elem Res 169:1–7. https://doi.org/10.1007/s12011-015-0395-3
Tippairote T, Temviriyanukul P, Benjapong W, Trachootham D (2017) Hair zinc and severity of symptoms are increased in children with attention deficit and hyperactivity disorder: a hair multi-element profile study. Biol Trace Elem Res 179:185–194. https://doi.org/10.1007/s12011-017-0978-2
Comai S, Bertazzo A, Vachon J, Daigle M, Toupin J, Côté G, Gobbi G (2019) Trace elements among a sample of prisoners with mental and personality disorders and aggression: correlation with impulsivity and ADHD indices. J Trace Elem Med Biol 51:123–129. https://doi.org/10.1016/j.jtemb.2018.10.008
Ghanizadeh A, Berk M (2013) Zinc for treating of children and adolescents with attention-deficit hyperactivity disorder: a systematic review of randomized controlled clinical trials. Eur J Clin Nutr 67:122–124. https://doi.org/10.1038/ejcn.2012.177
Zamora J, Velasquez A, Troncoso L, Barra P, Guajardo K, Castillo-Duran C (2011) Zinc in the therapy of the attention-deficit/hyperactivity disorder in children. A preliminar randomized controlled trial. Arch Latinoam Nutr 61:242–246
El-Bakry A, El Safty AM, Abdou AA, Amin OR, Ayoub DR, Afifi DY (2019) Effect of zinc supplementation in zinc-deficient children with attention-deficit hyperactivity disorder. Egypt J Psychiatr 40:86–94. https://doi.org/10.4103/ejpsy.ejpsy_10_19
Lepping P, Huber M (2010) Role of zinc in the pathogenesis of attention-deficit hyperactivity disorder. CNS Drugs 24:721–728. https://doi.org/10.2165/11537610-000000000-00000
Kozielec T, Starobrat-Hermelin B (1997) Assessment of magnesium levels in children with attention deficit hyperactivity disorder (ADHD). Magnes Res 10:143–148
Effatpanah M, Rezaei M, Effatpanah H, Effatpanah Z, Varkaneh HK, Mousavi SM, Fatahi S, Rinaldi G, Hashemi R (2019) Magnesium status and attention deficit hyperactivity disorder (ADHD): a meta-analysis. Psychiatry Res 274:228–234. https://doi.org/10.1016/j.psychres.2019.02.043
Huang YH, Zeng BY, Li DJ, Cheng YS, Chen TY, Liang HY, Yang WC, Lin PY, Chen YW, Tseng PT, Lin CH (2019) Significantly lower serum and hair magnesium levels in children with attention deficit hyperactivity disorder than controls: a systematic review and meta-analysis. Prog Neuro-Psychopharmacol Biol Psychiatry 90:134–141. https://doi.org/10.1016/j.pnpbp.2018.11.012
Kirkland A, Sarlo G, Holton K (2018) The role of magnesium in neurological disorders. Nutrients 10:730. https://doi.org/10.3390/nu10060730
El Baza F, AlShahawi HA, Zahra S, Abdel Hakim RA (2016) Magnesium supplementation in children with attention deficit hyperactivity disorder. Egypt J Med Hum Genet 17:63–70. https://doi.org/10.1016/j.ejmhg.2016.04.009
Mousain-Bosc M, Roche M, Rapin J, Bali JP (2004) Magnesium VitB6 intake reduces central nervous system hyperexcitability in children. J Am Coll Nutr 23:545S–548S. https://doi.org/10.1080/07315724.2004.10719400
Slutsky I, Abumaria N, Wu LJ, Huang C, Zhang L, Li B, Zhao X, Govindarajan A, Zhao MG, Zhuo M, Tonegawa S (2010) Enhancement of learning and memory by elevating brain magnesium. Neuron 65:165–177. https://doi.org/10.1016/j.neuron.2009.12.026
Ode A, Rylander L, Gustafsson P, Lundh T, Källén K, Olofsson P, Ivarsson SA, Rignell-Hydbom A (2015) Manganese and selenium concentrations in umbilical cord serum and attention deficit hyperactivity disorder in childhood. Environ Res 137:373–381. https://doi.org/10.1016/j.envres.2015.01.001
Cheong H, Kwon H, Kim E, Ha M, Hong Y, Kang D, Moon S (2008) Blood manganese level and attention deficit/hyperactivity disorder in early school age children. Epidemiology 19:S223–S224. https://doi.org/10.1097/01.ede.0000340168.26974.7b
Hong SB, Kim JW, Choi BS, Hong YC, Park EJ, Shin MS, Kim BN, Yoo HJ, Cho IH, Bhang SY, Cho SC (2014) Blood manganese levels in relation to comorbid behavioral and emotional problems in children with attention-deficit/hyperactivity disorder. Psychiatry Res 220:418–425. https://doi.org/10.1016/j.psychres.2014.05.049
Farias AC, Cunha A, Benko CR, McCracken JT, Costa MT, Farias LG, Cordeiro ML (2010) Manganese in children with attention-deficit/hyperactivity disorder: relationship with methylphenidate exposure. J Am Acad Child Adolesc Psychiatry 20:113–118
Shin DW, Kim EJ, Lim SW, Shin YC, Oh KS, Kim EJ (2015) Association of hair manganese level with symptoms in attention-deficit/hyperactivity disorder. Psychiatry Investig 12:66–72. https://doi.org/10.4306/pi.2015.12.1.66
Bhang SY, Cho SC, Kim JW, Hong YC, Shin MS, Yoo HJ, Cho IH, Kim Y, Kim BN (2013) Relationship between blood manganese levels and children’s attention, cognition, behavior, and academic performance—a nationwide cross-sectional study. Environ Res 126:9–16. https://doi.org/10.1016/j.envres.2013.05.006
Torrente M, Gascon M, Vrijheid M, Sunyer J, Forns J, Domingo J, Nadal M (2013) Levels of metals in hair in childhood: preliminary associations with neuropsychological behaviors. Toxics 2:1–16. https://doi.org/10.3390/toxics2010001
Bouchard M, Laforest F, Vandelac L, Bellinger D, Mergler D (2006) Hair manganese and hyperactive behaviors: pilot study of school-age children exposed through tap water. Environ Health Perspect 115:122–127. https://doi.org/10.1289/ehp.9504
Skalnaya MG, Skalny AV (2018) Essential trace elements in human health: a physician’s view. Publishing House of Tomsk State University, Tomsk
Zoni S, Lucchini RG (2013) Manganese exposure: cognitive, motor and behavioral effects on children: a review of recent findings. Curr Opin Pediatr 25:255–260. https://doi.org/10.1097/MOP.0b013e32835e906b
Mahmoud MM, El-Mazary AAM, Maher RM, Saber MM (2011) Zinc, ferritin, magnesium and copper in a group of Egyptian children with attention deficit hyperactivity disorder. Ital J Pediatr 37:60. https://doi.org/10.1186/1824-7288-37-60
Zhou F, Wu F, Zou S, Chen Y, Feng C, Fan G (2016) Dietary, nutrient patterns and blood essential elements in Chinese children with ADHD. Nutrients 8:352. https://doi.org/10.3390/nu8060352
Gaier ED, Eipper BA, Mains RE (2013) Copper signaling in the mammalian nervous system: synaptic effects. J Neurosci Res 91:2–19. https://doi.org/10.1002/jnr.23143
Tabatadze T, Kherkheulidze M, Kandelaki E, Kavlashvili N, Ivanashvili T (2018) Attention deficit hyperactivity disorder and hair heavy metal and essential trace element concentrations. Is there a link? Georgian Med News 284:88–92
Tudosie M, Truţă E, Daviţoiu AM, Mitu AM, Bojescu AA (2017) Optoelectronics method for determining the cobalt involved in symptoms of attention deficit hyperactivity disorder. 2017 9th International Conference on Electronics, Computers and Artificial Intelligence (ECAI) IEEE pp 1–4. https://doi.org/10.1109/ECAI.2017.8166474
Zhou T, Guo J, Zhang J, Xiao H, Qi X, Wu C, Chang X, Zhang Y, Lui Q, Zhou Z (2019) Sex-specific differences in cognitive abilities associated with childhood cadmium and manganese exposures in school-age children: a prospective cohort study. Biol Trace Elem Res. https://doi.org/10.1007/s12011-019-01703-9
Skalny AV, Simashkova NV, Klyushnik TP, Grabeklis AR, Bjørklund G, Skalnaya MG, Nikonorov AA, Tinkov AA (2017) Hair toxic and essential trace elements in children with autism spectrum disorder. Metab Brain Dis 32:195–202. https://doi.org/10.1007/s11011-016-9899-6
Saghazadeh A, Ahangari N, Hendi K, Saleh F, Rezaei N (2017) Status of essential elements in autism spectrum disorder: systematic review and meta-analysis. Rev Neurosci 28:783–809. https://doi.org/10.1515/revneuro-2017-0015
Catalani S, Rizzetti MC, Padovani A, Apostoli P (2012) Neurotoxicity of cobalt. Hum Exp Toxicol 31:421–437. https://doi.org/10.1177/0960327111414280
Jones SM, Novak AE, Elliott JP (2013) The role of HIF in cobalt-induced ischemic tolerance. Neuroscience 252:420–430. https://doi.org/10.1016/j.neuroscience.2013.07.060
Skalny AV, Zaitseva IP, Gluhcheva YG, Skalny AA, Achkasov EE, Skalnaya MG, Tinkov AA (2019) Cobalt in athletes: hypoxia and doping – new crossroads. J Appl Biomed:21–28. https://doi.org/10.32725/jab.2018.003
Black MM (2008) Effects of vitamin B12 and folate deficiency on brain development in children. Food Nutr Bull 29:S126–S131. https://doi.org/10.1177/15648265080292S117
Saha T, Chatterjee M, Sinha S, Rajamma U, Mukhopadhyay K (2017) Components of the folate metabolic pathway and ADHD core traits: an exploration in eastern Indian probands. J Hum Genet 62:687–695. https://doi.org/10.1038/jhg.2017.23
Nielsen FH (2014) Update on the possible nutritional importance of silicon. J Trace Elem Med Biol 28:379–382. https://doi.org/10.1016/j.jtemb.2014.06.024
Martin KR (2013) Silicon: the health benefits of a metalloid. In: Sigel A, Sigel H, Sigel R (eds) Interrelations between essential metal ions and human diseases. Springer, Dordrecht, pp 451–473
Komorowski JR, Tuzcu M, Sahin N, Juturu V, Orhan C, Ulas M, Sahin K (2012) Chromium picolinate modulates serotonergic properties and carbohydrate metabolism in a rat model of diabetes. Biol Trace Elem Res 149:50–56. https://doi.org/10.1007/s12011-012-9393-x
Sahin K, Tuzcu M, Orhan C, Gencoglu H, Ulas M, Atalay M, Sahin N, Hayirli A, Komorowski JR (2012) The effects of chromium picolinate and chromium histidinate administration on NF-κB and Nrf2/HO-1 pathway in the brain of diabetic rats. Biol Trace Elem Res 150:291–296. https://doi.org/10.1007/s12011-012-9475-9
Chen WY, Mao FC, Liu CH, Kuan YH, Lai NW, Wu CC, Chen CJ (2016) Chromium supplementation improved post-stroke brain infarction and hyperglycemia. Metab Brain Dis 31:289–297. https://doi.org/10.1007/s11011-015-9749-y
Chen HJ, Lee YJ, Yeh GC, Lin HC (2013) Association of attention-deficit/hyperactivity disorder with diabetes: a population-based study. Pediatr Res 73:492. https://doi.org/10.1038/pr.2013.5
Davidson JR, Abraham K, Connor KM, McLeod MN (2003) Effectiveness of chromium in atypical depression: a placebo-controlled trial. Biol Psychiatry 53:261–264. https://doi.org/10.1016/S0006-3223(02)01500-7
Wojciak RW, Mojs E, Stanislawska-Kubiak M, Samborski W (2013) The serum zinc, copper, iron, and chromium concentrations in epileptic children. Epilepsy Res 104:40–44. https://doi.org/10.1016/j.eplepsyres.2012.09.009
Brownley KA, Girdler SS, Stout AL, McLeod MN (2013) Chromium supplementation for menstrual cycle-related mood symptoms. J Diet Suppl 10:345–356. https://doi.org/10.3109/19390211.2013.830678
Quinn PO, Madhoo M (2014) A review of attention-deficit/hyperactivity disorder in women and girls: uncovering this hidden diagnosis. Prim Care Companion CNS Disord 16. https://doi.org/10.4088/PCC.13r01596
Nussbaum NL (2012) ADHD and female specific concerns: a review of the literature and clinical implications. J Atten Disord 16:87–100. https://doi.org/10.1177/1087054711416909
Hubbs-Tait L, Nation JR, Krebs NF, Bellinger DC (2005) Neurotoxicants, micronutrients, and social environments: individual and combined effects on children’s development. Psychol Sci Public Interest 6:57–121. https://doi.org/10.1111/j.1529-1006.2005.00024.x
Funding
The project was supported by RFBR No. 19-013-00528.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tinkov, A.A., Mazaletskaya, A.L., Ajsuvakova, O.P. et al. ICP-MS Assessment of Hair Essential Trace Elements and Minerals in Russian Preschool and Primary School Children with Attention-Deficit/Hyperactivity Disorder (ADHD). Biol Trace Elem Res 196, 400–409 (2020). https://doi.org/10.1007/s12011-019-01947-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-019-01947-5