Abstract
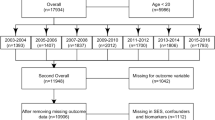
Internal migration and urbanization are occurring on a global scale. Although the risk of exposure to stress/lead/low selenium is assumed to be high among migrant pregnant women, population-based evidence is limited. This study aims to explore the association of internal-migration status with maternal exposure to lead, low selenium, and stress among pregnant women. A total of 1931 pregnant women were investigated in 2010. The internal-migration status was grouped based on their hukou (registered residence) and length-of-residency in Shanghai. Maternal blood lead and serum selenium concentrations were assessed. Life event stress and emotional stress were evaluated using “Event-Stress-Scale-for-Pregnant-Women” and “Symptom-Checklist-90-R-Scale” (SCL-90-R), respectively. Logistic regression and general linear models were used to evaluate associations between migration status and lead/stress/low selenium exposure. Compared with the local (with Shanghai hukou and length-of-residency ≥ 5 years), new migrants (without Shanghai hukou and length-of-residency < 2 years) had lower social-economic-status (SES), higher lead, life event and emotional stress, and lower selenium levels. After adjusting for SES, new migrants had higher risks of emotional stress (for interpersonal sensitivity of SCL-90-R, OR = 2.10, 95% CI 1.22–3.64) and low selenium [lg(selenium): beta = − 0.08, 95% CI − 0.11, − 0.05], but no significant risks for life event stress and high lead. Compared with the local, migrant pregnant women in big cities may have emotional stress and low selenium independent of SES, and high lead and life event stress dependent on SES.
Similar content being viewed by others
References
Neiderud CJ (2015) How urbanization affects the epidemiology of emerging infectious diseases. Infect Ecol Epidemiol 5:27060. https://doi.org/10.3402/iee.v5.27060
Tian Z, Cao G, Shi J, McCallum I, Cui L, Fan D, Li X (2012) Urban transformation of a metropolis and its environmental impacts: a case study in Shanghai. Environ Sci Pollut Res Int 19(5):1364–1374. https://doi.org/10.1007/s11356-011-0641-y
Qiu P, Caine E, Yang Y, Chen Q, Li J, Ma X (2011) Depression and associated factors in internal migrant workers in China. J Affect Disord 134(1–3):198–207. https://doi.org/10.1016/j.jad.2011.05.043
Dipietro JA (2012) Maternal stress in pregnancy: considerations for fetal development. J Adolesc Health 51(2 Suppl):S3–S8. https://doi.org/10.1016/j.jadohealth.2012.04.008
Tegethoff M, Greene N, Olsen J, Meyer AH, Meinlschmidt G (2010) Maternal psychosocial adversity during pregnancy is associated with length of gestation and offspring size at birth: evidence from a population-based cohort study. Psychosom Med 72(4):419–426. https://doi.org/10.1097/PSY.0b013e3181d2f0b0
Torres JM, Wallace SP (2013) Migration circumstances, psychological distress, and self-rated physical health for Latino immigrants in the United States. Am J Public Health 103(9):1619–1627. https://doi.org/10.2105/ajph.2012.301195
Zelkowitz P, Schinazi J, Katofsky L, Saucier J, Valenzuela M, Westreich R, Dayan J (2004) Factors associated with depression in pregnant immigrant women. Transcult Psychiatry 41(4):445–464. https://doi.org/10.1177/1363461504047929
Gao S, Jin Y, Unverzagt FW, Liang C, Hall KS, Cao J, Ma F, Murrell JR, Cheng Y, Li P, Bian J, Hendrie HC (2012) Selenium level and depressive symptoms in a rural elderly Chinese cohort. BMC Psychiatry 12:72. https://doi.org/10.1186/1471-244x-12-72
Benton D (2002) Selenium intake, mood and other aspects of psychological functioning. Nutr Neurosci 5(6):363–374. https://doi.org/10.1080/1028415021000055925
Makhoul IR, Sammour RN, Diamond E, Shohat I, Tamir A, Shamir R (2004) Selenium concentrations in maternal and umbilical cord blood at 24-42 weeks of gestation: basis for optimization of selenium supplementation to premature infants. Clin Nutr 23(3):373–381. https://doi.org/10.1016/j.clnu.2003.08.004
Wells EM, Jarrett JM, Lin YH, Caldwell KL, Hibbeln JR, Apelberg BJ, Herbstman J, Halden RU, Witter FR, Goldman LR (2011) Body burdens of mercury, lead, selenium and copper among Baltimore newborns. Environ Res 111(3):411–417. https://doi.org/10.1016/j.envres.2010.12.009
Smith AM, Picciano MF (1986) Evidence for increased selenium requirement for the rat during pregnancy and lactation. J Nutr 116(6):1068–1079. https://doi.org/10.1093/jn/116.6.1068
Pieczynska J, Grajeta H (2015) The role of selenium in human conception and pregnancy. J Trace Elem Med Biol 29:31–38. https://doi.org/10.1016/j.jtemb.2014.07.003
Kaplowitz SA, Perlstadt H, Dziura JD, Post LA (2016) Behavioral and environmental explanations of elevated blood lead levels in immigrant children and children of immigrants. J Immigr Minor Health 18(5):979–986. https://doi.org/10.1007/s10903-015-0243-8
Wu WT, Liou SH, Lin KJ, Liu TE, Liu SH, Chen CY, Sung FC, Wu TN (2009) Changing blood lead levels and DNA damage (comet assay) among immigrant women in Taiwan. Sci Total Environ 407(23):5931–5936. https://doi.org/10.1016/j.scitotenv.2009.07.025
Poropat AE, Laidlaw MAS, Lanphear B, Ball A, Mielke HW (2018) Blood lead and preeclampsia: a meta-analysis and review of implications. Environ Res 160:12–19. https://doi.org/10.1016/j.envres.2017.09.014
Taylor CM, Golding J, Emond AM (2015) Adverse effects of maternal lead levels on birth outcomes in the ALSPAC study: a prospective birth cohort study. BJOG 122(3):322–328. https://doi.org/10.1111/1471-0528.12756
Xie X, Ding G, Cui C, Chen L, Gao Y, Zhou Y, Shi R, Tian Y (2013) The effects of low-level prenatal lead exposure on birth outcomes. Environ Pollut 175:30–34. https://doi.org/10.1016/j.envpol.2012.12.013
Yan CH, Xu J, Shen XM (2013) Childhood lead poisoning in China: challenges and opportunities. Environ Health Perspect 121(10):A294
Cleveland LM, Minter ML, Cobb KA, Scott AA, German VF (2008) Lead hazards for pregnant women and children: part 1: immigrants and the poor shoulder most of the burden of lead exposure in this country. Part 1 of a two-part article details how exposure happens, whom it affects, and the harm it can do. Am J Nurs 108(10):40–49; quiz 50. https://doi.org/10.1097/01.naj.0000337736.76730.66
Wu WT, Wu CC, Lin YJ, Shen CY, Liu TY, Yang CY, Liou SH, Wu TN (2013) Changing blood lead levels and oxidative stress with duration of residence among Taiwan immigrants. J Immigr Minor Health 15(6):1048–1056. https://doi.org/10.1007/s10903-013-9820-x
Program. UND China National Human Development Report 2013—Sustainable and liveable cities: toward ecological civilization. (2013. http://www.undp.org/content/dam/china/docs/Publications/UNDP-CH_2013%20NHDR_EN.pdf. Accessed April 27, 2016)
Tegethoff M, Greene N, Olsen J, Schaffner E, Meinlschmidt G (2011) Stress during pregnancy and offspring pediatric disease: a National Cohort Study. Environ Health Perspect 119(11):1647–1652. https://doi.org/10.1289/ehp.1003253
WY. W Symptom Checklist 90. In: Zhang, ZJ, Eds Behavior Scale Rating Manual, 1st ed Chinese Medical Multimedia Press, Beijing, 2005:64–67 [in Chinese]
LR D SCL-90-R: administration, scoring and procedures manual, 3rd ed. National Computer Systems Inc, Minneapolis
Skroder HM, Hamadani JD, Tofail F, Persson LA, Vahter ME, Kippler MJ (2015) Selenium status in pregnancy influences children’s cognitive function at 1.5 years of age. Clin Nutr 34(5):923–930. https://doi.org/10.1016/j.clnu.2014.09.020
Committee opinion No. 533: lead screening during pregnancy and lactation (2012). Obstetrics and gynecology 120 (2 Pt 1):416–420. doi:https://doi.org/10.1097/AOG.0b013e31826804e8
Suarez L, Cardarelli K, Hendricks K (2003) Maternal stress, social support, and risk of neural tube defects among Mexican Americans. Epidemiology 14(5):612–616. https://doi.org/10.1097/01.ede.0000073270.39780.e9
Jensen HH, Mortensen EL, Lotz M (2013) SCL-90-R symptom profiles and outcome of short-term psychodynamic group therapy. ISRN Psychiatry 2013:540134–540137. https://doi.org/10.1155/2013/540134
Li S, Xiao T, Zheng B (2012) Medical geology of arsenic, selenium and thallium in China. Sci Total Environ 421-422:31–40. https://doi.org/10.1016/j.scitotenv.2011.02.040
Mistry HD, Wilson V, Ramsay MM, Symonds ME, Broughton Pipkin F (2008) Reduced selenium concentrations and glutathione peroxidase activity in preeclamptic pregnancies. Hypertension 52(5):881–888. https://doi.org/10.1161/hypertensionaha.108.116103
Schulpis KH, Karakonstantakis T, Gavrili S, Chronopoulou G, Karikas GA, Vlachos G, Papassotiriou I (2004) Maternal-neonatal serum selenium and copper levels in Greeks and Albanians. Eur J Clin Nutr 58(9):1314–1318. https://doi.org/10.1038/sj.ejcn.1601967
Nwagha UI, Ogbodo SO, Nwogu-Ikojo EE, Ibegbu DM, Ejezie FE, Nwagha TU, Dim CC (2011) Copper and selenium status of healthy pregnant women in Enugu, southeastern Nigeria. Niger J Clin Pract 14(4):408–412. https://doi.org/10.4103/1119-3077.91745
Rayman MP, Wijnen H, Vader H, Kooistra L, Pop V (2011) Maternal selenium status during early gestation and risk for preterm birth. CMAJ 183(5):549–555. https://doi.org/10.1503/cmaj.101095
Kantola M, Purkunen R, Kroger P, Tooming A, Juravskaja J, Pasanen M, Seppanen K, Saarikoski S, Vartiainen T (2004) Selenium in pregnancy: is selenium an active defective ion against environmental chemical stress? Environ Res 96(1):51–61. https://doi.org/10.1016/j.envres.2004.03.003
Laclaustra M, Navas-Acien A, Stranges S, Ordovas JM, Guallar E (2009) Serum selenium concentrations and hypertension in the US population. Circ Cardiovasc Qual Outcomes 2(4):369–376. https://doi.org/10.1161/circoutcomes.108.831552
Bodnar LM, Wisner KL (2005) Nutrition and depression: implications for improving mental health among childbearing-aged women. Biol Psychiatry 58(9):679–685. https://doi.org/10.1016/j.biopsych.2005.05.009
Sher L (2002) Effects of selenium status on mood and behaviour: role of thyroid hormones. Aust N Z J Psychiatry 36(4):559–560. https://doi.org/10.1046/j.1440-1614.2002.t01-2-01066.x
Naicker N, Norris SA, Mathee A, von Schirnding YE, Richter L (2010) Prenatal and adolescent blood lead levels in South Africa: child, maternal and household risk factors in the Birth to Twenty cohort. Environ Res 110(4):355–362. https://doi.org/10.1016/j.envres.2010.02.006
Nriagu J, Senthamarai-Kannan R, Jamil H, Fakhori M, Korponic S (2011) Lead poisoning among Arab American and African American children in the Detroit metropolitan area, Michigan. Bull Environ Contam Toxicol 87(3):238–244. https://doi.org/10.1007/s00128-011-0346-4
Bellinger DC (2013) Prenatal exposures to environmental chemicals and children’s neurodevelopment: an update. Saf Health Work 4(1):1–11. https://doi.org/10.5491/shaw.2013.4.1.1
Cory-Slechta DA, Virgolini MB, Thiruchelvam M, Weston DD, Bauter MR (2004) Maternal stress modulates the effects of developmental lead exposure. Environ Health Perspect 112(6):717–730
Virgolini MB, Rossi-George A, Lisek R, Weston DD, Thiruchelvam M, Cory-Slechta DA (2008) CNS effects of developmental Pb exposure are enhanced by combined maternal and offspring stress. Neurotoxicology 29(5):812–827. https://doi.org/10.1016/j.neuro.2008.03.003
Qian LJ, Shen BB, YMSe a (2012) Mental health levels of 206 cases of normal pregnant women and relevant influencing factors in a 3A hospital in Anqing. Anhui Med Pharm J 16:400–402
Funding
This study was supported by National Natural Science Foundation of China [NCFS, 81673189, 30901205, 81373016]; Shanghai Health and Family Planning Commission [201640363]; National Key Research and Development Program of China [2016FYC1000203]; and Shanghai Jiao Tong University School of Medicine Gaofeng Clinical Medicine Grant Support [20172016]. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NCFS or STCSM.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Jiang, S., Yang, B., Xu, J. et al. Associations of Internal-Migration Status with Maternal Exposure to Stress, Lead, and Selenium Deficiency Among Pregnant Women in Shanghai, China. Biol Trace Elem Res 190, 309–317 (2019). https://doi.org/10.1007/s12011-018-1570-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-018-1570-0