Abstract
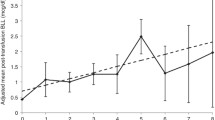
Very low birth weight (VLBW) infants usually receive packed red blood cell unit (pRBC) transfusions. Heavy metal transfer via pRBCs is not widely discussed before. This study aimed to determine pre-/post-transfusion erythrocyte lead and mercury levels in infants and to correlate these levels to heavy metal concentrations in pRBCs. VLBW infants (n = 80), needing pRBC transfusion for the first time, were enrolled. Erythrocyte heavy metal levels were determined in pre-/post-transfusion blood samples and also in pRBC units. Mean lead and mercury levels in the pRBCs were found to be 16.3 ± 10.8 and 3.75 ± 3.23 μg/L, respectively. Of the infants, 69.7% received lead above reference dose. Erythrocyte lead levels increased significantly after transfusions (10.6 ± 10.3 vs. 13 ± 8.5, p < 0.05) with significant correlated to amount of lead within pRBCs (r = 0.28). Mean pre-/post-transfusion erythrocyte mercury levels were 3.28 ± 3.08 and 3.5 ± 2.83 μg/L, respectively (p > 0.05). There was a significant correlation between mean difference of mercury levels after transfusion and amount of mercury delivered by pRBCs (r = 0.28). Infants can be subject to high levels of lead and mercury through pRBC transfusions.



Similar content being viewed by others
Abbreviations
- ATSDR:
-
Agency for Toxic Substances and Disease Registry
- CDC:
-
Centers for Disease Control and Prevention
- CI:
-
Confidence interval
- CL:
-
Confidence level
- CPDA-1:
-
Citrate-phosphate-dextrose-adenine
- ELBW:
-
Extremely low birth weight
- EPA:
-
Environmental Protection Agency
- IQ:
-
Intelligence quotient
- JECFA:
-
the Joint Food and Agriculture Organization/World Health Organization Expert Committee
- LOD:
-
Limit of detection
- NHANES:
-
National Health and Nutrition Examination Survey
- NICU:
-
Neonatal intensive care unit
- OSHA:
-
the US Occupational Safety and Health Administration
- pRBC:
-
packed red blood cell unit
- RfD:
-
Reference dose
- VLBW:
-
Very low birth weight
- WHO:
-
World Health Organization
References
Fabres J, Wehrli G, Marques MB, Phillips V, Dimmitt RA, Westfall AO, Schelonka RL (2006) Estimating blood needs for very-low-birth-weight infants. Transfusion 46(11):1915–1920
Sources of Lead. New York State. April 2010. Available from: https://www.health.ny.gov/environmental/lead/sources.htm. Last accessed: 26th June, 2018
Mercury in the Environment and Water Supply. Sources of Mercury. Available from: https://people.uwec.edu/piercech/hg/mercury_water/sources.htm. Last accessed: 26th June, 2018
Davidson PW, Palumbo D, Myers GJ, Cox C, Shamlaye CF, Sloane-Reeves J, Cernichiari E, Wilding GE, Clarkson TW (2000) Neurodevelopmental outcomes of Seychellois children from the pilot cohort at 108 months following prenatal exposure to methylmercury from a maternal fish diet. Environ Res 84(1):1–11
Hu H, Téllez-Rojo MM, Bellinger D, Smith D, Ettinger AS, Lamadrid-Figueroa H, Schwartz J, Schnaas L, Mercado-García A, Hernández-Avila M (2006) Fetal lead exposure at each stage of pregnancy as a predictor of infant mental development. Environ Health Perspect 114(11):1730–1735
Dorea JG, Donangelo CM (2006) Early (in uterus and infant) exposure to mercury and lead. Clin Nutr 25(11):369–376
Lanphear BP, Hornung R, Khoury J, Yolton K, Baghurst P, Bellinger DC, Canfield RL, Dietrich KN, Bornschein R, Greene T, Rothenberg SJ, Needleman HL, Schnaas L, Wasserman G, Graziano J, Roberts R (2005) Low-level environmental lead exposure and children's intellectual function: an international pooled analysis. Environ Health Perspect 113(7):894–899
Canfield RL, Henderson CR, Cory-Slechta DA, Cox C, Juski TA et al (2003) Intellectual impairment in children with blood lead concentrations below 10 μg per deciliter. New Engl J Med 348(16):1517–1526
Centers for Disease Control and Prevention (2002) Response to advisory committee on childhood lead poisoning prevention recommendations in “low level lead exposure harms children: a renewed call of primary prevention”. US Department of Health and Human Services, Atlanta Available from: URL: https://www.cdc.gov/nceh/lead/acclpp/cdc_response_lead_exposure_recs.pdf
Grandjean P, Weihe P, White RF, Debes F, Araki S, Yokoyama K, Murata K, SØRENSEN N, Dahl R, JØRGENSEN PJ (1997) Cognitive deficit in 7-year-old children with prenatal exposure to methylmercury. Neurotoxicol Teratol 19(6):417–428
Jedrychowski W, Jankowski J, Flak E, Skarupa A, Mroz E, Sochacka-Tatara E et al (2006) Effects of prenatal exposure to mercury on cognitive and psychomotor function in one-year-old infants: epidemiologic cohort study in Poland. Ann Epidemiol 16(6):439–447
Clifton JC 2nd (2007) Mercury exposure and public health. Pediatr Clin N Am 54(2):237–269
Elabiad MT, Hook RE (2013) Lead content of blood transfusions for extremely low-birth-weight infants. Am J Perinatol 30(9):765–770
Sundararajan S, Blatz AM, Dearborn DG, Varnes AW, Bearer CF, El Metwally D (2015) Toxic metal contamination of banked blood designated for neonatal transfusion. J Clin Toxicol 5(5):1–5
Joint Food and Agriculture Organization/World Health Organization Expert Committee on Food Additives (JECFA). 73rd meeting; Geneva; June 8–17, 2010. Available from: URL: www.who.int/ foodsafety/publications/chem/ summary73.pdf. Last accessed December, 2017
ASTDR. Toxicological profile for mercury: Update Atlanta, GA: ASTDR. Available from: URL: www.atsdr.cdc.gov/toxprofiles/tp46.pdf. Last accessed December, 2017
World Health Organization. Joint FAO/WHO expert committee on food additives: 61st Meeting, Rome, 10–19 June. Available from: URL: ftp://ftp.fao.org/es/esn/jecfa/jecfa61sc.pdf
US Environmental Protection Agency. Methylmercury (MeHg) (CASRN 22967–92-6). Available from: URL: www.epa.gov/iris/subst/0073. Last accessed December, 2017
Bain A, Blackburn S (2004) Issues in transfusing preterm infants in the NICU. J Perinat Neonatal Nurs 18(2):170–182
Elabiad MT, Christensen M (2014) Changes in premature infant mercury and lead blood levels after blood transfusions. Am J Perinatol 31(10):863–868
Ozment CP, Turi JL (2009) Iron overload following red blood cell transfusion and its impact on disease severity. Biochim Biophys Acta 1790(7):694–701
Widness JA, Seward VJ, Kromer IJ, Burmeister LF, Bell EF, Strauss RG (1996) Changing patterns of red blood cell transfusion in very low birth weight infants. J Pediatr 129(5):680–687
Strauss RG (1997) Practical issues in neonatal transfusion practice. Am J Clin Pathol 107(4 Suppl 1):S57–S63
Moretti R, Pansiot J, Bettati D, Strazielle N, Ghersi-Egea JF et al (2015) Blood-brain barrier dysfunction in disorders of the developing brain. Front Neurosci 9(1):40
Kirpalani H, Whyte RK, Andersen C, Asztalos EV, Heddle N, Blajchman MA, Peliowski A, Rios A, LaCorte M, Connelly R, Barrington K, Roberts RS (2006) The premature infants in need of transfusion (PINT) study: a randomized, controlled trial of a restrictive (low) versus liberal (high) transfusion threshold for extremely low birth weight infants. J Pediatr 149(3):301–307
Chen HL, Tseng HI, Lu CC, Yang SN, Fan HC, Yang RC (2009) Effect of blood transfusions on the outcome of very low body weight preterm infants under two different transfusion criteria. Pediatr Neonatol 50(3):110–116
Bell EF (2008) When to transfuse preterm babies. Arch Dis Child Fetal Neonatal Ed 93(6):F469–F473
Bearer CF, O'Riordan MA, Powers R (2000) Lead exposure from blood transfusion to premature infants. J Pediatr 137(4):549–554
Kirel B, Akşit MA, Bulut H (2005) Blood lead levels of maternal-cord pairs, children and adults who live in a central urban area in Turkey. Turk J Pediatr 47(2):125–131
The National Institute for Occupational Safety and Health (NIOSH). Adult blood lead epidemiology and Surveillance (ABLES). Available from: URL: http://www.cdc.gov/niosh/topics/ables/description.html. Last accessed December, 2017
Zubairi H, Visintainer P, Fleming J, Richardson M, Singh R (2015) Lead exposure in preterm infants receiving red blood cell transfusions. Pediatr Res 77(6):814–818
Centers for Disease Control and Prevention (2004) Blood mercury levels in young children and childbearing-aged women—United States, 1999—2002. MMWR 53:1018–1020
Kher K, Mistry K (2014) Assessment of glomerular and tubular function. Curr Pediatr Rev 10(2):142–150
Stajich GV, Lopez GP, Harry SW, Sexson WR (2000) Iatrogenic exposure to mercury after hepatitis B vaccination in preterm infants. J Pediatr 136(5):679–681
Harville EW, Hertz-Picciotto I, Schramm M, Watt-Morse M, Chantala K, Osterloh J, Parsons PJ, Rogan W (2005) Factors influencing the difference between maternal and cord blood lead. Occup Environ Med 62(4):263–269
Ettinger AS, Hu H, Hernandez-Avila M (2007) Dietary calcium supplementation to lower blood lead levels in pregnancy and lactation. J Nutr Biochem 18(3):172–178
Wu J, Ying T, Shen Z, Wang H (2014) Effect of low-level prenatal mercury exposure on neonate neurobehavioral development in China. Pediatr Neurol 51(1):93–99
Bulleova S, Rothenberg SJ, Manalo MA (2001) Lead levels in blood bank blood. Arch Environ Health 56(4):312–313
Bearer CF, Linsalata N, Yomtovian R, Walsh M, Singer L (2003) Blood transfusions: a hidden source of lead exposure. Lancet 362(9380):332
Hillyer C, Goldman M, Dzik S (2002) Journal club. Transfus Med Rev 16(4):325–333
Delage G, Gingras S, Rhainds M (2015) A population-based study on blood lead levels in blood donors. Transfusion 55:633–2640
Acknowledgements
We would like to thank Düzen Laboratories for their support in the measurement of erythrocyte mercury levels. This study is supported by Turkish Pediatric Association.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by Hacettepe University Human Ethics Committee (HEK 11/18-7).
Conflict of Interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Takci, S., Asci, A., Erkekoglu, P. et al. Lead and Mercury Levels in Preterm Infants Before and After Blood Transfusions. Biol Trace Elem Res 188, 344–352 (2019). https://doi.org/10.1007/s12011-018-1436-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-018-1436-5