Abstract
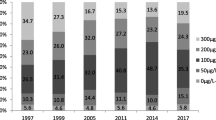
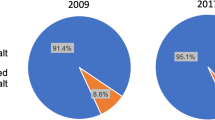
In Shanghai, a new iodized salt standard was implemented in 2012. To provide evidence to the government, we compared iodine status before (35 mg/kg) and after (30 mg/kg) adjustment in vulnerable populations living in Shanghai. The probability-proportional-to-size sampling technique was used to select at least 360 pregnant women for urine iodine test and at least 1200 students for thyroid measurement and the household salt test. Of these students, at least 360 performed urine iodine test. The median thyroid volume and the median household salt iodine concentration of children aged 8–10 years were 1.80 ml and 24.8 mg/kg in 2015, and 0.97 ml and 28.3 mg/kg in 2011. The median urine iodine concentration (UIC) of pregnant women was 126.52 and 139.77 μg/L in 2015 and 2011. All differences were statistically significant (P < 0.05). The median UIC of students was 171.40 and 181.63 μg/L in 2015 and 2011, the difference was not statistically significant. Multivariate linear regression analysis showed that thyroid volume in children was associated with sex, age, region, and household salt iodized concentration. The current iodized salt concentration meets the basic needs of the population’s iodine requirements except for pregnant women. Periodic monitoring is necessary particularly in vulnerable groups.
Similar content being viewed by others
References
Abd El Naser Yamamah G, Kamel AF, Abd-El Dayem S, Hussein AS, Salama H (2013) Thyroid volumes and iodine status in Egyptian South Sinai schoolchildren. Arch Med Sci 9(3):548–554. https://doi.org/10.5114/aoms.2012.30952
Zimmermann MB (2009) Iodine deficiency. Endocr Rev 30(4):376–408. https://doi.org/10.1210/er.2009-0011
Andersson M, Karumbunathan V, Zimmermann MB (2012) Global iodine status in 2011 and trends over the past decade. J Nutr 142(4):744–750. https://doi.org/10.3945/jn.111.149393
Auso E, Lavado-Autric R, Cuevas E, Del Rey FE, Morreale De Escobar G et al (2004) A moderate and transient deficiency of maternal thyroid function at the beginning of fetal neocorticogenesis alters neuronal migration. Endocrinology 145(9):4037–4047. https://doi.org/10.1210/en.2004-0274
Walker SP, Wachs TD, Gardner JM, Lozoff B, Wasserman GA et al (2007) Child development: risk factors for adverse outcomes in developing countries. Lancet 369(9556):145–157. https://doi.org/10.1016/S0140-6736(07)60076-2
Zimmermann MB, Andersson M (2012) Update on iodine status worldwide. Curr Opin Endocrinol Diabetes Obes 19(5):382–387. https://doi.org/10.1097/MED.0b013e328357271a
Nystrom HF, Brantsaeter AL, Erlund I, Gunnarsdottir I, Hulthen L et al (2016) Iodine status in the Nordic countries—past and present. Food Nutr Res 60(1):31969. https://doi.org/10.3402/fnr.v60.31969
Lazarus JH (2014) Iodine status in europe in 2014. Eur Thyroid J 3(1):3–6. https://doi.org/10.1159/000358873
Tran TD, Hetzel B, Fisher J (2016) Access to iodized salt in 11 low- and lower-middle-income countries: 2000 and 2010. Bull World Health Organ 94(2):122–129. https://doi.org/10.2471/BLT.15.160036
Laurberg P, Bulow Pedersen I, Knudsen N, Ovesen L, Andersen S (2001) Environmental iodine intake affects the type of nonmalignant thyroid disease. Thyroid 11(5):457–469. https://doi.org/10.1089/105072501300176417
Li C, Xingb M, Baoxiu Z et al (1998) Pioneer study of IDD in Shanghai. Chinese journal of endemiology 17:16–19
Fund/International WHOUNCs, Disorders CftCoID (2001) Assessment of iodine deficiency disorders and monitoring their elimination. Geneva
Yan Y, Zhang Y, Liu L, Liu J, L W (2006) Method for determination of iodine in urine by As3+-Ce4+catalytic spectrophotometry (WS/T 107–2006). People’s Medical Publishing House, Beijing (in Chinese)
WHO/UNICEF/ICCIDD (2007) Assessment of iodine deficiency disorders and monitoring their elimination: a guide for programme managers, 3rd edn. World Health Organization, Geneva (SZ)
Supervision SBoQT (2011) General test method in salt industry-determination of iodine GB 26878-2011. China Criteria Publishing House, Beijing (in Chinese)
Fuse Y, Saito N, Tsuchiya T, Shishiba Y, Irie M (2007) Smaller thyroid gland volume with high urinary iodine excretion in Japanese schoolchildren: normative reference values in an iodine-sufficient area and comparison with the WHO/ICCIDD reference. Thyroid 17(2):145–155. https://doi.org/10.1089/thy.2006.0209
Zou S, Wu F, Guo C, Song J, Huang C, Zhu Z, Yu H, Guo Y, Lu X, Ruan Y (2012) Iodine nutrition and the prevalence of thyroid disease after salt iodization: a cross-sectional survey in Shanghai, a coastal area in China. PLoS One 7(7):e40718. https://doi.org/10.1371/journal.pone.0040718
WHO (2011) Guidelines for drinking-water quality, 4th edn. World Health Organization, Gutenberg
Zimmermann MB, Jooste PL, Pandav CS (2008) Iodine-deficiency disorders. Lancet 372(9645):1251–1262. https://doi.org/10.1016/S0140-6736(08)61005-3
Gutekunst R, Smolarek H, Hasenpusch U, Stubbe P, Friedrich HJ, Wood WG, Scriba PC (1986) Goitre epidemiology: thyroid volume, iodine excretion, thyroglobulin and thyrotropin in Germany and Sweden. Acta Endocrinol 112(4):494–501
Melse-Boonstra A, Jaiswal N (2010) Iodine deficiency in pregnancy, infancy and childhood and its consequences for brain development. Best Pract Res Clin Endocrinol Metab 24(1):29–38. https://doi.org/10.1016/j.beem.2009.09.002
Zou Y, Lou X, Ding G, Mo Z, Zhu W, Mao G (2014) Iodine nutritional status after the implementation of the new iodized salt concentration standard in Zhejiang Province, China. BMC Public Health 14(1):836. https://doi.org/10.1186/1471-2458-14-836
Yang J, Zhu L, Li X, Zheng H, Wang Z, Liu Y, Hao Z (2016) Iodine status of vulnerable populations in Henan Province of China 2013–2014 after the implementation of the new iodized salt standard. Biol Trace Elem Res 173(1):7–13. https://doi.org/10.1007/s12011-016-0619-1
Luo Y, Kawashima A, Ishido Y, Yoshihara A, Oda K, Hiroi N, Ito T, Ishii N, Suzuki K (2014) Iodine excess as an environmental risk factor for autoimmune thyroid disease. Int J Mol Sci 15(7):12895–12912. https://doi.org/10.3390/ijms150712895
Delshad H, Touhidi M, Abdollahi Z, Hedayati M, Salehi F, Azizi F (2016) Inadequate iodine nutrition of pregnant women in an area of iodine sufficiency. J Endocrinol Investig 39(7):755–762. https://doi.org/10.1007/s40618-016-0438-4
O'Donnell KJ, Rakeman MA, Zhi-Hong D, Xue-Yi C, Mei ZY, DeLong N, Brenner G, Tai M, Dong W, DeLong GR (2002) Effects of iodine supplementation during pregnancy on child growth and development at school age. Dev Med Child Neurol 44(02):76–81. https://doi.org/10.1017/S0012162201001712
Bath SC, Rayman MP (2015) A review of the iodine status of UK pregnant women and its implications for the offspring. Environ Geochem Health 37(4):619–629. https://doi.org/10.1007/s10653-015-9682-3
Berbel P, Mestre JL, Santamaria A, Palazon I, Franco A et al (2009) Delayed neurobehavioral development in children born to pregnant women with mild hypothyroxinemia during the first month of gestation: the importance of early iodine supplementation. Thyroid 19(5):511–519. https://doi.org/10.1089/thy.2008.0341
Bath SC, Walter A, Taylor A, Wright J, Rayman MP (2014) Iodine deficiency in pregnant women living in the South East of the UK: the influence of diet and nutritional supplements on iodine status. Br J Nutr 111(09):1622–1631. https://doi.org/10.1017/S0007114513004030
Zimmermann MB, Aeberli I, Torresani T, Burgi H (2005) Increasing the iodine concentration in the Swiss iodized salt program markedly improved iodine status in pregnant women and children: a 5-y prospective national study. Am J Clin Nutr 82(2):388–392
Mayor S (2015) Giving all pregnant women iodine supplements could save costs of cognitive impairment, study finds. BMJ 351:h4337
Ferreira SM, Navarro AM, Magalhaes PK, Maciel LM (2014) Iodine insufficiency in pregnant women from the State of Sao Paulo. Arq Bras Endocrinol Metabol 58(3):282–287. https://doi.org/10.1590/0004-2730000002979
Knight BA, Shields BM, He X, Pearce EN, Braverman LE, Sturley R, Vaidya B (2017) Iodine deficiency amongst pregnant women in South-West England. Clin Endocrinol 86(3):451–455. https://doi.org/10.1111/cen.13268
Simpong DL, Adu P, Bashiru R, Morna MT, Yeboah FA, Akakpo K, Ephraim RKD (2016) Assessment of iodine status among pregnant women in a rural community in Ghana—a cross sectional study. Arch Public Health 74(1):8. https://doi.org/10.1186/s13690-016-0119-y
Andersen S, Karmisholt J, Pedersen KM, Laurberg P (2008) Reliability of studies of iodine intake and recommendations for number of samples in groups and in individuals. Br J Nutr 99(4):813–818. https://doi.org/10.1017/S0007114507842292
Acknowledgements
We thank all the children and pregnant women who participated in this study. We also thank the healthcare professionals at the Centers for Disease Control and Prevention of the 17 districts in Shanghai for their assistance.
Financial Support
The current study was supported by the National Nature Science Foundation of China (No. 81602851), Excellent Young Talents of Health System in Shanghai (No. 2017YQ043), the Fourth Three-Year Public Health Program (No. GWIV-27.1), and Key Disciplines (No. 15GWZK0801). None of the above funders played a role in the study design, data analysis or manuscript writing.
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiments: Shoujun Liu, Xiaohui Su, and Peng Liu; Performed the experiments: Shurong Zou, Jun Song, and Zhengyuan Wang; Analyzed the data: Zhengyuan Wang; Wrote the paper: Zhengyuan Wang. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Wang, Z., Liu, P., Su, X. et al. A Comparison of Iodine Status in Children and Pregnant Women After a Policy Change in the Iodized Salt Standard in Shanghai, China. Biol Trace Elem Res 185, 275–281 (2018). https://doi.org/10.1007/s12011-018-1257-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-018-1257-6