Abstract
This research was delineated to explore the efficacy of selenium nanoparticles delivered in liposomes (L-Se) in the mitigation of type-2 diabetes mellitus. Adult female Wistar rats were assigned into four groups: group I, the normal control group in which the rats received normal saline solution orally; group II, the diabetic control group in which the rats were injected intraperitoneally with a single dose of streptozotocin (STZ) for induction of diabetes; group III, the metformin (Met)-treated group in which the diabetic rats were treated orally with Met; and group IV, the L-Se-treated group in which the diabetic rats were treated orally with L-Se. All treatments were delivered for 21 days. Blood and pancreas tissue samples were obtained for biochemical analysis, immunohistochemical examinations, and histopathological investigation. The L-Se-treated group showed significant drop in serum glucose and pancreatic malondialdehyde (MDA), nitric oxide (NO), tumor necrosis factor-α (TNF-α), and prostaglandin F2α (PGF2α) levels associated with significant rise in serum insulin and pancreatic glutathione, superoxide dismutase (SOD), catalase (CAT), glutathione peroxidase (GPx), and glutathione reductase (GR) values, in addition to significant improvement in the immunohistochemical indices (insulin and glucagon). Aforementioned results are appreciated by the histopathological findings of pancreatic tissue. In conclusion, our data have brought about compelling evidence favoring the antidiabetic potency of elemental selenium nanoparticles delivered in liposomes through preservation of pancreatic β cell integrity with consequent increment of insulin secretion and in turn glucose depletion, repression of oxidative stress, potentiation of the antioxidant defense system, and inhibition of pancreatic inflammation.





Similar content being viewed by others
Abbreviations
- AGE:
-
Advanced glycosylation end product
- AMPK:
-
AMP-activated protein kinase
- ANOVA:
-
One-way analysis of variance
- ATF-3:
-
Activating transcription factor-3
- CAT:
-
Catalase
- COX-2:
-
Cyclooxygenase-2
- CREB:
-
cAMP responsive element binding protein
- DM:
-
Diabetes mellitus
- DPPC:
-
L-α-dipalmitoyl phosphatidyl choline
- DTNB:
-
5,5′ dithiobis (2-nitrobenzoic acid)
- ELISA:
-
Enzyme-linked immunosorbent assay
- GPx:
-
Glutathione peroxidase
- GR:
-
Glutathione reductase
- GSSG:
-
Oxidized glutathione
- IFN-γ:
-
Interferon-gamma
- IL-1β:
-
Interleukin-1 beta
- IL-6:
-
Interleukin-6
- IL-10:
-
Interleukin-10
- iNOS:
-
Inducible nitric oxide synthase
- IK-Bα:
-
Nuclear factor of kappa light polypeptide gene enhancer in B cell inhibitor alpha
- Ipf1:
-
Insulin promoter factor 1
- JNK1/2:
-
c-Jun N-terminal kinase 1/2
- LPS:
-
Lipopolysaccharides
- L-Se:
-
Selenium nanoparticles delivered in liposomes
- MAPK:
-
Mitogen-activated protein kinase
- MDA:
-
Malondialdehyde
- Met:
-
Metformin
- Na2SeO3 :
-
Sodium selenite
- NBT:
-
Nitroblue tetrazolium
- NF-κB:
-
Nuclear factor kappa B
- NO:
-
Nitric oxide
- PAP:
-
Peroxidase anti-peroxidase
- PGE2:
-
Prostaglandin E2
- PGF2α:
-
Prostaglandin F2α
- ROS:
-
Reactive oxygen species
- Se:
-
Selenium
- SOD:
-
Superoxide dismutase
- SPSS:
-
Statistical package for the social sciences program
- STZ:
-
Streptozotocin
- T2DM:
-
Type 2 diabetes mellitus
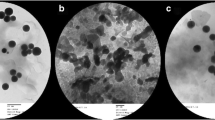
- TEM:
-
Transmission electron microscope
- TNF-α:
-
Tumor necrosis factor-α
References
Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE (2014) Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes E Res Clin Pract 103:137–149. doi:10.1016/j.diabres.2013.11.002
Usha J, Raut P, Agrawal S, Patra P, Maheshwari B, Apurb M, Dhirhe T (2011) Evaluation of serum selenium level in patients with uncomplicated diabetes mellitus. J Clin Diagn Res 5:70–73
Mercuri F, Quagliaro L, Ceriello A (2000) Oxidative stress evaluation in diabetes. Diabetes Technol Ther 2(4):589–600. doi:10.1089/15209150050502014
Park K, Rimm EB, Siscovick DS, Spiegelman D, Manson JE, Morris JS, Hu FB, Mozaffarian D (2012) Toenail selenium and incidence of type 2 diabetes in U.S. men and women. Diabetes Care 35(7):1544–1551. doi:10.2337/dc11-2136
Simmons RA (2012) Developmental origins of diabetes: the role of oxidative stress. Best Pract Res Clin Endocrinol Metab 26(5):701–708. doi:10.1016/j.beem.2012.03.012
Ziegler D, Sohr CG, Nourooz-Zadeh N (2004) Oxidative stress and antioxidant defense in relation to the severity of diabetic polyneuropathy and cardiovascular autonomic neuropathy. Diabetes Care 27(9):2178–2183. doi:10.2337/diacare.27.9.2178
Pandey KB, Rizvi SI (2009) Plant polyphenols as dietary antioxidants in human health and disease. Oxidative Med Cell Longev 2(5):270–278. doi:10.4161/oxim.2.5.9498
Jozanov-Stankov O, Demajo M, Djujić I, Mandić M (1998) Selenium intake as a modulator of responsiveness to oxidative stress. J Environ Pathol Toxicol Oncol 17(3–4):251–257
Wang H, Wei W, Zhang SY, Shen YX, Wang NP, Yue L, Xu SY (2005) Melatonin-selenium nanoparticles protects liver against immunological injury induced by bacillus Calmette-Guerin and lipopolysaccharide. Acta Pharmacol Sin 26(6):745–752. doi:10.1111/j.1745-7254.2005.00745.x
Srivastava P, Braganca JM, Kowshik M (2014) In vivo synthesis of selenium nanoparticles by Halococcus salifodinae BK18 and their anti-proliferative properties against HeLa cell line. Biotechnol Prog 30(6):1480–1487. doi:10.1002/btpr.1992
Hassanin KM, Abd El-Kawi SH, Hashem KS (2013) The prospective protective effect of selenium nanoparticles against chromium-induced oxidative and cellular damage in rat thyroid. Int J Nanomedicine 8:1713–1720. doi:10.2147/IJN.S42736
Abdelaleem RMA, Abdel Hameed HF, Askar ME, Hassan SHM, El-Batal AI (2016) Modulatory role of selenium nanoparticles and grape seed extract mixture on oxidative stress biomarkers in diabetic irradiated rats. Indian Journal of Pharmaceutical Education and Research 50(1):170–178. doi:10.5530/ijper.50.1.21
Al-Quraishy S, Dkhil MA, Abdel Moneim AE (2015) Anti-hyperglycemic activity of selenium nanoparticles in streptozotocin-induced diabetic rats. Int J Nanomedicine 10:6741–6756. doi:10.2147/IJN.S91377
Spangler RS (1990) Insulin administration via liposomes. Diabetes Care 13(9):911–922. doi:10.2337/diacare.13.9.911
Dwivedi C, Shah CP, Singh K, Kumar M, Bajaj PN (2011) An organic acid-induced synthesis and characterization of selenium nanoparticles. Journal of Nanotechnology 2011:1–6. doi:10.1155/2011/651971
Kim S, Jacobs RE, White SH (1985) Preparation of multilamellar vesicles of defined size-distribution by solvent-spherule evaporation. Biochim Biophys Acta 812(3):793–801. doi:10.1016/0005-2736(85)90274-3·
Wei M, Ong L, Smith MT, Ross FB, Schmid K, Hoey AJ, Burstow D, Brown L (2003) The streptozotocin-diabetic rat as a model of the chronic complications of human diabetes. Heart Lung Circ 12(1):44–50. doi:10.1046/j.1444-2892.2003.00160.x
Kosegawa I, Chen S, Awata T, Negishi K, Katayama S (1999) Troglitazone and metformin, but not glibenclamide, decrease blood pressure in Otsuka Long Evans Tokushima fatty rats. Clin Exp Hypertens 21(3):199–211. doi:10.3109/10641969909068661
Loeschner K, Hadrup N, Hansen M, Pereira SA, Gammelgaard B, Møller LH, Mortensen A, Lam HR, Larsen EH (2014) Absorption, distribution, metabolism and excretion of selenium following oral administration of elemental selenium nanoparticles or selenite in rats. Metallomics 6(2):330–337. doi:10.1039/c3mt00309d
Trinder P (1969) Determination of blood glucose using an oxidase-peroxidase system with a non-carcinogenic chromogen. J Clin Pathol 22(2):158–161. doi:10.1136/jcp.22.2.158
Temple R, Clark PMS, Hales CN (1992) Measurement of insulin secretion in type 2 diabetes: problems and pitfalls. Diabetic Med 9:503–512. doi:10.1111/j.1464-5491.1992.tb01830.x
Ohkawa H, Ohishi N, Yagi K (1979) Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 95(2):351–358. doi:10.1016/0003-2697(79)90738-3
Green LC, Wagner DA, Glogowski J, Skipper PL, Wishnok JS, Tannenbaum SR (1982) Analysis of nitrate, nitrite, and [15 N]nitrate in biological fluids. Anal Biochem 126(1):131–138. doi:10.1016/0003-2697(82)90118-X
Ellman GL (1959) Tissue sulfhydryl groups. Arch Biochem Biophys 82(1):70–77. doi:10.1016/0003-9861(59)90090-6
Nishikimi M, Appaji N, Yagi K (1972) The occurrence of superoxide anion in the reaction of reduced phenazine methosulfate and molecular oxygen. Biochem Biophys Res Commun 46(2):849–854. doi:10.1016/S0006-291X(72)80218-3
Aebi H (1984) Catalase in vitro. Methods Enzymol 105:121–126. doi:10.1016/S0076-6879(84)05016-3
Paglia DE, Valentine WN (1967) Studies on the quantitative and qualitative characterization of erythrocyte glutathione peroxidase. J Lab Clin Med 70(1):158–169
Factor VM, Kiss A, Woitach JT, Wirth PJ, Thorgeirsson SS (1998) Disruption of redox homeostasis in the transforming growth factor-alpha/c-myc transgenic mouse model of accelerated hepatocarcinogenesis. J Biol Chem 273(25):15846–15853. doi:10.1074/jbc.273.25.15846
Sternberger LA (1979) Immunocytochemistry, 2nd edn. Wiley medical publication, New York
Banchroft JD, Stevens A, Turner DR (1996) Theory and practice of histological techniques, 4th edn. Churchill Livingstone, Philadelphia
Defronza RA, Nir B, Donald CS (1991) Mechanism of metformin action in obese and lean non-insulin depended diabetic subjects. J Clin Endoc and Meta 73:1294–1301. doi:10.1210/jcem-73-6-1294#sthash.LVB4wfVq.dpuf
Ilahi I, Asghar A, Ali S, Khan M Khan N(2012) Beneficial effects of Pentanema vestitum Linn. whole plant on the glucose and other biochemical parameters of alloxan induced diabetic rabbits. ISRN Pharmacol 2012:478023. doi:10.5402/2012/478023
Fazilati M, AbdolYousefi NN, Kelishadi MR, Ghasemi A, Zamani S, Soleymani R, Rahimi A (2016) The effect of hypoglysemia of selenium nano particles on lipid profiles and thyroid factors in diabetic male rats by streptoysin in compared to glibenclamide drug. IJBPAS 5(1):335–341
Mueller AS, Pallauf J (2006) Compendium of the antidiabetic effects of supranutritional selenate doses. In vivo and in vitro investigations with type II diabetic db/db mice. J Nutr Biochem 17(8):548–560. doi:10.1016/j.jnutbio.2005.10.006
Eskander EF, Ahmed HH, Estefan SF (2000) Hypoglycemic and insulinotropic action of gastropods (Lambis-lambis-L) extracts on alloxan diabetic male rats. The Arab Journal of Laboratory Medicine 26(2):185–201
Hei YJ, Farahbakhshian S, Chen X, Battell ML, McNeill JH (1998) Stimulation of MAP kinase and S6 kinase by vanadium and selenium in rat adipocytes. Mol Cell Biochem 178(1–2):367–375. doi:10.1023/A:1006819906820
Gorray KC, Baskin D, Brodsky J, Fujimoto WY (1986) Responses of pancreatic b cells to alloxan and streptozotocin in the guinea pig. Pancreas 1(2):130–138
Matough FA, Budin SB, Hamid ZA, Alwahaibi N, Mohamed J (2012) The role of oxidative stress and antioxidants in diabetic complications. Sultan Qaboos Univ Med J 12(1):5–18
Neri S, Signorelli SS, Torrisi B, Pulvirenti D, Mauceri B, Abate G, Ignaccolo L, Bordonaro F, Cilio D, Calvagno S, Leotta C (2005) Effects of antioxidant supplementation on postprandial oxidative stress and endothelial dysfunction: a single-blind, 15-day clinical trial in patients with untreated type 2 diabetes, subjects with impaired glucose tolerance, and healthy controls. Clin Ther 27(11):1764–1773. doi:10.1016/j.clinthera.2005.11.006
Matsuoka T, Kajimoto Y, Watada H, Kaneto H, Kishimoto M, Umayahara Y, Fujitani Y, Kamada T, Kawamori R, Yamasaki Y (1997) Glycation-dependent, reactive oxygen species-mediated suppression of the insulin gene promoter activity in HIT cells. J Clin Invest 99(1):144–150. doi:10.1172/JCI119126
Kaneto H, Kajimoto Y, Miyagawa J, Matsuoka T, Fujitani Y, Umayahara Y, Hanafusa T, Matsuzawa Y, Yamasaki Y, Hori M (1999) Beneficial effects of antioxidants in diabetes: possible protection of pancreatic beta-cells against glucose toxicity. Diabetes 48(12):2398–2406. doi:10.2337/diabetes.48.12.2398
Majithiya JB, Balaraman R (2006) Metformin reduces blood pressure and restores endothelial function in aorta of streptozotocin-induced diabetic rats. Life Sci 78(22):2615–2624. doi:10.1016/j.lfs.2005.10.020
Kato Y, Koide N, Komatsu T, Tumurkhuu G, Dagvadorj J, Kato K, Yokochi T (2010) Metformin attenuates production of nitric oxide in response to lipopolysaccharide by inhibiting MyD88-independent pathway. Horm Metab Res 42(9):632–636. doi:10.1055/s-0030-1255033
Tong WM, Wang F (1998) Alterations in rat pancreatic islet beta cells induced by keshan disease pathogenic factors: protective action of selenium and vitamin E. Metab Clin Exp 47(4):415–419. doi:10.1016/S0026-0495(98)90052-X
Zeng J, Zhou J, Huang K (2009) Effect of selenium on pancreatic proinflammatory cytokines in streptozotocin-induced diabetic mice. J Nutr Biochem 20(7):530–536. doi:10.1016/j.jnutbio.2008.05.012
Birben E, Sahiner UM, Sackesen C, Erzurm S, Kalayci O (2012) Oxidative stress and antioxidant defense. WAO Journal 5:9–19. doi:10.1097/WOX.0b013e3182439613
Chakraborty A, Chowdhury S, Bhattacharyya M (2011) Effect of metformin on oxidative stress, nitrosative stress and inflammatory biomarkers in type 2 diabetes patients. Diabetes Res Clin Pract 93(1):56–62. doi:10.1016/j.diabres.2010.11.030
Faure P, Rossini E, Wiernsperger N (1999) An insulin sensitizer improves the free radical defense system potential and insulin sensitivity in high fructose-fed rats. Diabetes 48:353–357. doi:10.2337/diabetes.48.2.353
Wang YX, Zhan XA, Yuan D, Zhang XW, Wu RJ (2011) Effects of selenomethionine and sodium selenite supplementation on meat quality, selenium distribution and antioxidant status in broilers. Czech J Anim Sci 56(7):305–313
Beisswenger P, Rugiero-Lopez D (2003) Metformin inhibition of glycation processes. Diabetes Metab 29(6s):95–103. doi:10.1016/S1262-3636(03)72793-1
Tessier D, Maheux P, Khalil A, Fülöp T (1999) Effects of gliclazide versus metformin on the clinical profile and lipid peroxidation markers in type 2 diabetes. Metabolism 48(7):897–903. doi:10.1016/S0026-0495(99)90226-3
Ceriello A, Bortolotti N, Falleti E (1997) Total radical-trapping antioxidant parameter in NIDDM patients. Diabetes Care 20:194–197
Aguirre F, Martin J, Grinspon D (1998) Oxidative damage, plasma antioxidant capacity and glycemic control in elderly NIDDM patients. Free Radic Biol Med 24:580–585. doi:10.1016/S0891-5849(97)00293-1
Kohrle J, Brigelius-Flohe R, Bock A, Gartner R, Meyer O, Flohe L (2000) Selenium in biology: facts and medical perspectives. Biol Chem 381:849–864
Mohapatra P, Swain RK, Mishra SK, Behera T, Swain P, Mishra SS, Behura NC, Sabat SC, Sethy K, Dhama K, Jayasankar P (2014) Effects of dietary nano-selenium on tissue selenium deposition, antioxidant status and immune functions in layer chicks. Int J Pharmacol 10:160–167. doi:10.3923/ijp.2014.160.167
Liao CD, Hung WL, Jan KC, Yeh AI, Ho CT, Hwang LS (2010) Nano/sub-microsized lignan glycosides from sesame meal exhibit higher transport and absorption efficiency in Caco-2 cell monolayer. Food Chem 119:896–902. doi:10.1016/j.foodchem.2009.07.056
Pradhan AD, Manson JE, Rifai N, Buring JE, Ridker PM (2001) C-reactive protein, interleukin 6, and risk of developing type 2 diabetes mellitus. JAMA 286(3):327–334. doi:10.1001/jama.286.3.327
Esposito K, Nappo F, Marfella R, Giugliano G, Giugliano F, Ciotola M, Quagliaro L, Ceriello A, Giugliano D (2002) Inflammatory cytokine concentrations are acutely increased by hyperglycemia in humans: role of oxidative stress. Circulation 106(16):2067–2072. doi:10.1161/01.CIR.0000034509.14906.AE
Pickup JC, Chusney GD, Thomas SM, Burt D (2000) Plasma interleukin-6, tumour necrosis factor α and blood cytokine production in type 2 diabetes. Life Sci 67(3):291–300. doi:10.1016/S0024-3205(00)00622-6
Schottker B, Herder C, Rothenbacher D, Roden M, Kolb H, Müller H, Brenner H (2013) Proinflammatory cytokines, adiponectin, and increased risk of primary cardiovascular events in diabetic patients with or without renal dysfunction: results from the ESTHER study. Diabetes Care 36(6):1703–1711. doi:10.2337/dc12-1416
Andrews M, Soto N, Arredondo M (2012) Effect of metformin on the expression of tumor necrosis factor-α, Toll like receptors 2/4 and C reactive protein in obese type-2 diabetic patients. Rev Med Chil 140(11):1377–1382. doi:10.4067/S0034-98872012001100001
Isoda K, Young JL, Zirlik A, MacFarlane LA, Tsuboi N, Gerdes N, Schönbeck U, Libby P (2006) Metformin inhibits proinflammatory responses and nuclear factor-kappa B in human vascular wall cells. Arterioscler Thromb Vasc Biol 26(3):611–617. doi:10.1161/01.atv.0000201938.78044.75
Hyun B, Shin S, Lee A, Lee S, Song Y, Ha NJ, Cho KH, Kim K (2013) Metformin down-regulates TNF-α secretion via suppression of scavenger receptors in macrophages. Immune Netw 13(4):123–132. doi:10.4110/in.2013.13.4.123
Kim J, Kwak HJ, Cha JY, Jeong YS, Rhee SD, Kim KR, Cheon HG (2014) Metformin suppresses lipopolysaccharide (LPS)-induced inflammatory response in murine macrophages via activating transcription factor-3 (ATF-3) induction. J Biol Chem 289(33):23246–23255. doi:10.1074/jbc.M114.577908
Mohammed ET, Safwat GM (2013) Assessment of the ameliorative role of selenium nanoparticles on the oxidative stress of acetaminophen in some tissues of male albino rats. Beni-Suef University Journal of Basic and Applied Sciences 2(2):80–85. doi:10.1016/j.bjbas.2013.01.003
Wang J, Zhang Y, Yuan Y, Yue T (2014) Immunomodulatory of selenium nano-particles decorated by sulfated Ganoderma lucidum polysaccharides. Food Chem Toxicol 68:183–189. doi:10.1016/j.fct.2014.03.003
Ito M, Kondo Y, Nakatani A, Hayashi K, Naruse A (2001) Characterization of low dose streptozotocin-induced progressive diabetes in mice. Environ Toxicol Pharmacol 9(3):71–78
Hassan Z, Yam MF, Ahmad M, Yusof APM (2010) Antidiabetic properties and mechanism of action of Gynura procumbens water extract in streptozotocin-induced diabetic rats. Molecules 15:9008–9023. doi:10.3390/molecules15129008
Yu B, Pugazhenthi S, Khandelwal RL (1994) Effects of metformin on glucose and glucagon regulated gluconeogenesis in cultured normal and diabetic hepatocytes. Biochem Pharmacol 48(5):949–954
Campbell SC, Aldibbiat A, Marriott CE, Landy C, Ali T, Ferris WF, Butler CS, Shaw JA, Macfarlane WM (2008) Selenium stimulates pancreatic beta-cell gene expression and enhances islet function. FEBS Lett 582(15):2333–2337. doi:10.1016/j.febslet.2008.05.038
Roden M, Prskavec M, Fürnsinn C, Elmadfa I, König J, Schneider B, Wagner O, Waldhäusl W (1995) Metabolic effect of sodium selenite: insulin-like inhibition of glucagon-stimulated glycogenolysis in the isolated perfused rat liver. Hepatology 22(1):169–174. doi: 10.1002/hep.1840220127
Kanter M, Coskun O, Korkmaz A, Oter S (2004) Effects of Nigella sativa on oxidative stress and beta-cell damage in streptozotocin-induced diabetic rats. Anat Rec A Discov Mol Cell Evol Biol 279(1):685–691. doi:10.1002/ar.a.20056
Cuncio F, Pegoraro I, Dello-Russo P, Falleti F, Perrella G, Ceriello A (1995) SOD and GSH inhibit the high glucose induced oxidative damage and the PDGF increased secretion in cultured human endothelial cells. Thromb Haemost 74:963–973
Hull RL, Shen ZP, Watts MR, Kodama K, Carr DB, Utzschneider KM, Zraika S, Wang F, Kahn SE (2005) Long-term treatment with rosiglitazone and metformin reduces the extent of, but does not prevent, islet amyloid deposition in mice expressing the gene for human islet amyloid polypeptide. Diabetes 54(7):2235–2244. doi:10.2337/diabetes.54.7.2235
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All animals received care in compliance with the Egyptian rules for animal experiments which were approved by the Ethical Committee of Medical Research of the National Research Centre, Giza, Egypt.
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Ahmed, H.H., Abd El-Maksoud, M.D., Abdel Moneim, A.E. et al. Pre-Clinical Study for the Antidiabetic Potential of Selenium Nanoparticles. Biol Trace Elem Res 177, 267–280 (2017). https://doi.org/10.1007/s12011-016-0876-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-016-0876-z