Abstract
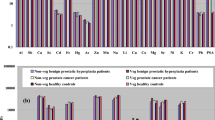
Although smoking is not associated with prostate cancer risk overall, smoking is associated with prostate cancer recurrence and mortality. Increased cadmium (Cd) exposure from smoking may play a role in progression of the disease. In this study, inductively coupled plasma mass spectrometry was used to determine Cd, arsenic (As), lead (Pb), and zinc (Zn) levels in formalin-fixed paraffin embedded tumor and tumor-adjacent non-neoplastic tissue of never- and ever-smokers with prostate cancer. In smokers, metal levels were also evaluated with regard to biochemical and distant recurrence of disease. Smokers (N = 25) had significantly higher Cd (median ppb, p = 0.03) and lower Zn (p = 0.002) in non-neoplastic tissue than never-smokers (N = 21). Metal levels were not significantly different in tumor tissue of smokers and non-smokers. Among smokers, Cd level did not differ by recurrence status. However, the ratio of Cd ppb to Pb ppb was significantly higher in both tumor and adjacent tissue of cases with distant recurrence when compared with cases without distant recurrence (tumor tissue Cd/Pb, 6.36 vs. 1.19, p = 0.009, adjacent non-neoplastic tissue Cd/Pb, 6.36 vs. 1.02, p = 0.038). Tissue Zn levels were also higher in smokers with distant recurrence (tumor, p = 0.039 and adjacent non-neoplastic, p = 0.028). These initial findings suggest that prostate tissue metal levels may differ in smokers with and without recurrence. If these findings are confirmed in larger studies, additional work will be needed to determine whether variations in metal levels are drivers of disease progression or are simply passengers of the disease process.
Similar content being viewed by others
Abbreviations
- ACBP/DBI:
-
acyl-CoA binding inhibitor/diazepam binding inhibitor
- ALAD:
-
Delta-aminolevulinic acid dehydratase
- As:
-
Arsenic
- Cd:
-
Cadmium
- FFPE:
-
Formalin-fixed paraffin embedded tissue
- ICP-MS:
-
Inductively coupled plasma mass spectrometry
- Pb:
-
Lead
- ppb:
-
Parts per billion
- PSA:
-
Prostate specific antigen
References
Colditz G (1996) Consensus conference: smoking and prostate cancer. Cancer Causes Control 7(5):560–562
Ray G, Henson DE, Schwartz AM (2010) Cigarette smoking as a cause of cancers other than lung cancer: an exploratory study using the Surveillance, Epidemiology, and End Results Program. Chest 138(3):491–499
Zu K, Giovannucci E (2009) Smoking and aggressive prostate cancer: a review of the epidemiologic evidence. Cancer Causes Control 20(10):1799–1810
Moreira DM, Antonelli JA, Presti JC Jr, Aronson WJ, Terris MK, Kane CJ, Amling CL, Freedland SJ (2010) Association of cigarette smoking with interval to biochemical recurrence after radical prostatectomy: results from the SEARCH database. Urology 76(5):1218–1223. doi:10.1016/j.urology.2010.01.066
Joshu CE, Mondul AM, Meinhold CL, Humphreys EB, Han M, Walsh PC, Platz EA (2011) Cigarette smoking and prostate cancer recurrence after prostatectomy. J Natl Cancer Inst 103(10):835–838. doi:10.1093/jnci/djr124
Kenfield SA, Stampfer MJ, Chan JM, Giovannucci E (2011) Smoking and prostate cancer survival and recurrence. JAMA 305(24):2548–2555. doi:10.1001/jama.2011.879
Giovannucci E, Liu Y, Platz EA, Stampfer MJ, Willett WC (2007) Risk factors for prostate cancer incidence and progression in the health professionals follow-up study. Int J Cancer 121(7):1571–1578. doi:10.1002/ijc.22788
Hartwig A (2013) Cadmium and cancer. Metal Ions Life Sci 11:491–507. doi:10.1007/978-94-007-5179-8_15
Joseph P (2009) Mechanisms of cadmium carcinogenesis. Toxicol Appl Pharmacol 238(3):272–279. doi:10.1016/j.taap.2009.01.011
Toxicological Profile For Cadmium (2012) (trans: U.S. Department of Health and Human Services PHS, Agency for Substances and Disease Registry (ATSDR)).
Beryllium, Cadmium, Mercury, and Exposures in the Glass Manufacturing Industry (1993). IARC Monographs on the Evaluation of Carcinogenic Risks to Humans vol 58.
Verougstraete V, Lison D, Hotz P (2003) Cadmium, lung and prostate cancer: a systematic review of recent epidemiological data. J ToxicolEnviron Health B Crit Rev 6(3):227–255
Sahmoun AE, Case LD, Jackson SA, Schwartz GG (2005) Cadmium and prostate cancer: a critical epidemiologic analysis. Cancer Investig 23(3):256–263
Chen YC, Pu YS, Wu HC, Wu TT, Lai MK, Yang CY, Sung FC (2009) Cadmium burden and the risk and phenotype of prostate cancer. BMC Cancer 9:429
Platz EA, Helzlsouer KJ, Hoffman SC, Morris JS, Baskett CK, Comstock GW (2002) Prediagnostic toenail cadmium and zinc and subsequent prostate cancer risk. Prostate 52(4):288–296
Vinceti M, Venturelli M, Sighinolfi C, Trerotoli P, Bonvicini F, Ferrari A, Bianchi G, Serio G, Bergomi M, Vivoli G (2007) Case–control study of toenail cadmium and prostate cancer risk in Italy. Sci Total Environ 373(1):77–81
Ogunlewe JO, Osegbe DN (1989) Zinc and cadmium concentrations in indigenous blacks with normal, hypertrophic, and malignant prostate. Cancer 63(7):1388–1392
Brys M, Nawrocka AD, Miekos E, Zydek C, Foksinski M, Barecki A, Krajewska WM (1997) Zinc and cadmium analysis in human prostate neoplasms. Biol Trace Elem Res 59(1–3):145–152
Anetor JI, Ajose F, Anetor GO, Iyanda AA, Babalola OO, Adeniyi FA (2008) High cadmium/zinc ratio in cigarette smokers: potential implications as a biomarker of risk of prostate cancer. Niger J Physiol Sci 23(1–2):41–49
Sarafanov AG, Todorov TI, Centeno JA, Macias V, Gao W, Liang WM, Beam C, Gray MA, Kajdacsy-Balla AA (2011) Prostate cancer outcome and tissue levels of metal ions. Prostate 71(11):1231–1238
Lazarevic K, Nikolic D, Stosic L, Milutinovic S, Videnovic J, Bogdanovic D (2012) Determination of lead and arsenic in tobacco and cigarettes: an important issue of public health. Cent Eur J Public Health 20(1):62–66
Rybicki BA, Neslund-Dudas C, Bock CH, Rundle A, Savera AT, Yang JJ, Nock NL, Tang D (2008) Polycyclic aromatic hydrocarbon–DNA adducts in prostate and biochemical recurrence after prostatectomy. Clin Cancer Res 14(3):750–757
Sarafanov AG, Todorov TI, Kajdacsy-Balla A, Gray MA, Macias V, Centeno JA (2008) Analysis of iron, zinc, selenium and cadmium in paraffin-embedded prostate tissue specimens using inductively coupled plasma mass-spectrometry. J Trace Elem Med Biol 22(4):305–314
Bae DS, Gennings C, Carter WH Jr, Yang RS, Campain JA (2001) Toxicological interactions among arsenic, cadmium, chromium, and lead in human keratinocytes. Toxicol Sci Off J Soc Toxicol 63(1):132–142
Smith DR, Kahng MW, Quintanilla-Vega B, Fowler BA (1998) High-affinity renal lead-binding proteins in environmentally-exposed humans. Chem Biol Int 115(1):39–52
Quintanilla-Vega B, Smith DR, Kahng MW, Hernandez JM, Albores A, Fowler BA (1995) Lead-binding proteins in brain tissue of environmentally lead-exposed humans. Chem Biol Int 98(3):193–209
Bergdahl IA, Grubb A, Schutz A, Desnick RJ, Wetmur JG, Sassa S, Skerfving S (1997) Lead binding to delta-aminolevulinic acid dehydratase (ALAD) in human erythrocytes. Pharmacol Toxicol 81(4):153–158
Iguchi K, Ito M, Usui S, Mizokami A, Namiki M, Hirano K (2008) Downregulation of thymosin beta4 expression by androgen in prostate cancer LNCaP cells. J Androl 29(2):207–212. doi:10.2164/jandrol.107.003608
Ettinger SL, Sobel R, Whitmore TG, Akbari M, Bradley DR, Gleave ME, Nelson CC (2004) Dysregulation of sterol response element-binding proteins and downstream effectors in prostate cancer during progression to androgen independence. Cancer Res 64(6):2212–2221
van Bemmel DM, Boffetta P, Liao LM, Berndt SI, Menashe I, Yeager M, Chanock S, Karami S, Zaridze D, Matteev V, Janout V, Kollarova H, Bencko V, Navratilova M, Szeszenia-Dabrowska N, Mates D, Slamova A, Rothman N, Han SS, Rosenberg PS, Brennan P, Chow WH, Moore LE (2011) Comprehensive analysis of 5-aminolevulinic acid dehydrogenase (ALAD) variants and renal cell carcinoma risk among individuals exposed to lead. PLoS One 6(7):e20432
Costello LC, Franklin RB (2011) Zinc is decreased in prostate cancer: an established relationship of prostate cancer! J Biol Inorg Chem 16(1):3–8
Leitzmann MF, Stampfer MJ, Wu K, Colditz GA, Willett WC, Giovannucci EL (2003) Zinc supplement use and risk of prostate cancer. J Natl Cancer Inst 95(13):1004–1007
Lawson KA, Wright ME, Subar A, Mouw T, Hollenbeck A, Schatzkin A, Leitzmann MF (2007) Multivitamin use and risk of prostate cancer in the National Institutes of Health-AARP Diet and Health Study. J Natl Cancer Inst 99(10):754–764. doi:10.1093/jnci/djk177
Prasad AS, Mukhtar H, Beck FW, Adhami VM, Siddiqui IA, Din M, Hafeez BB, Kucuk O (2010) Dietary zinc and prostate cancer in the TRAMP mouse model. J Med Food 13(1):70–76. doi:10.1089/jmf.2009.0042
Funding
Wayne State University, President’s Research Enhancement Program (to C.N.D.), the National Institute of Environmental Health Sciences (R01 ES011126 to B.A.R.), and the Department of Defense (W81XWH-07-1-0252 to C.N.D.)
Conflict of Interest
None declared
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Neslund-Dudas, C., Kandegedara, A., Kryvenko, O.N. et al. Prostate Tissue Metal Levels and Prostate Cancer Recurrence in Smokers. Biol Trace Elem Res 157, 107–112 (2014). https://doi.org/10.1007/s12011-013-9874-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-013-9874-6