Abstract
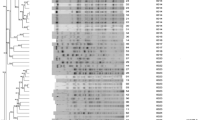
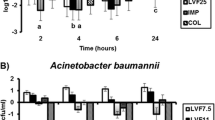
Pseudomonas aeruginosa can develop resistance. Therefore, it is necessary to design proper treatment for it. Pseudomonas aeruginosa can develop resistance against levofloxacin due to the development of efflux pumps. However, the development of these efflux pumps cannot develop resistance against imipenem. Additionally, the MexCDOprJ efflux system which is responsible for the resistance of Pseudomonas aeruginosa to levofloxacin is highly susceptible to imipenem. The objective of the study was to evaluate the emergence of resistance of Pseudomonas aeruginosa against 750 mg levofloxacin, 250 mg imipenem, and a combination of 750 mg levofloxacin and 250 mg imipenem. An in vitro pharmacodynamic model was selected for the evaluation of the emergence of resistance. Pseudomonas aeruginosa strain 236, Pseudomonas aeruginosa strain GB2, and Pseudomonas aeruginosa strain GB65 were selected. Susceptibility testing of both antibiotics was done by agar dilution methodology. A disk diffusion bioassay was performed for antibiotics. RT-PCR measurement was done for the evaluation of expressions of Pseudomonas aeruginosa genes. Samples were tested at 2 h, 4 h, 6 h, 8 h, 12 h, 16 h, 24 h, and 30 h. Levofloxacin and imipenem both individually reported a decrease in colony-forming unit per milliliter of strength in the initial stage but in the later stage both develop resistance individually. Levofloxacin with imipenem had no resistance to Pseudomonas aeruginosa during 30 h. Time after the start of development of resistance or decrease in clinical efficacy was higher for levofloxacin and imipenem combination in all strains. The concentration of Pseudomonas aeruginosa at the time after the start of development of resistance or decrease in clinical efficacy was fewer for levofloxacin and imipenem combination. Levofloxacin with imipenem is recommended for the treatment of infection due to Pseudomonas aeruginosa.







Similar content being viewed by others
Data Availability
The data of the study has been included in this study.
References
Lister, P. D., & Wolter, D. J. (2005). Levofloxacin-imipenem combination prevents the emergence of resistance among clinical isolates of Pseudomonas aeruginosa. Clinical Infectious Diseases, 40(Suppl 2), S105–S114.
Chiong, F., Wasef, M. S., Liew, K. C., Cowan, R., Tsai, D., Lee, Y. P., Croft, L., Harris, O., Gwini, S. M., & Athan, E. (2021). The impact of infectious diseases consultation on the management and outcomes of Pseudomonas aeruginosa bacteraemia in adults: A retrospective cohort study. BMC Infectious Diseases, 21(1), 671.
Tian, H. L., Shi, W., Zhou, H. F., Yuan, L., Yao, K. H., Rexiati, D., & Xu, A. M. (2018). Serotype distribution and drug resistance of Streptococcus pneumoniae, Haemophilus influenzae and Moraxella catarrhalis isolated from nasopharynx of Uygur children. Chinese Journal of Pediatrics, 56(4), 279–283. (In Chinese).
Hirabayashi, A., Kato, D., Tomita, Y., Iguchi, M., Yamada, K., Kouyama, Y., Morioka, H., Tetsuka, N., & Yagi, T. (2017). Risk factors for and role of OprD protein in increasing minimal inhibitory concentrations of carbapenems in clinical isolates of Pseudomonas aeruginosa. Journal of Medical Microbiology, 66(11), 1562–1572.
Purssell, A., & Poole, K. (2013). Functional characterization of the NfxB repressor of the mexCD-oprJ multidrug efflux operon of Pseudomonas aeruginosa. Microbiology, 159(Pt 10), 2058–2073.
Horna, G., López, M., Guerra, H., Saénz, Y., & Ruiz, J. (2018). Interplay between MexAB-OprM and MexEF-OprN in clinical isolates of Pseudomonas aeruginosa. Science and Reports, 8(1), 16463.
Sanz-García, F., Hernando-Amado, S., López-Causapé, C., Oliver, A., & Martínez, J. L. (2022). Low Ciprofloxacin concentrations select multidrug-resistant mutants overproducing efflux pumps in clinical isolates of Pseudomonas aeruginosa. Microbiology Spectrum, 10(5):e0072322. https://doi.org/10.1128/spectrum.00723-22
Sood, A., Angrup, A., Ray, P., & Bala, K. (2021). Comparative evaluation of agar dilution and broth microdilution by commercial and in-house plates for Bacteroides fragilis group: An economical and expeditious approach for resource-limited settings. Anaerobe, 71, 102443.
Ternant, D., Le Tilly, O., Picon, L., Moussata, D., Passot, C., Bejan-Angoulvant, T., Desvignes, C., Mulleman, D., Goupille, P., & Paintaud, G. (2021). Infliximab efficacy may be linked to full TNF-α blockade in peripheral compartment-a double central-peripheral target-mediated drug disposition (TMDD) model. Pharmaceutics, 13(11), 1821.
Louie, A., Grasso, C., Bahniuk, N., Van Scoy, B., Brown, D. L., Kulawy, R., & Drusano, G. L. (2010). The combination of meropenem and levofloxacin is synergistic with respect to both Pseudomonas aeruginosa kill rate and resistance suppression. Antimicrobial Agents and Chemotherapy, 54(6), 2646–2654. https://doi.org/10.1128/AAC.00065-10
Prashar, S., Portales Guemes, M., Shivbaran, P., Jimenez Alvarez, E., Soha, C., Nacer, S., McDonough, M., Plano, G. V., & Torruellas, G. J. (2021). Novel disk diffusion assay on magnesium oxalate agar to evaluate the susceptibility of Yersinia pestis to type III secretion system inhibitors. MicrobiolSpectr, 39(1), e0000521.
Fatima, H., Goel, N., Sinha, R., & Khare, S. K. (2021). Recent strategies for inhibiting multidrug-resistant and β-lactamase producing bacteria: A review. Colloids and Surfaces. B, Biointerfaces, 205, 111901.
Bottery, M. J., Matthews, J. L., Wood, A. J., Johansen, H. K., Pitchford, J. W., & Friman, V. P. (2022). Inter-species interactions alter antibiotic efficacy in bacterial communities. ISME Journal, 16(3), 812–821.
Chalhoub, H., Sáenz, Y., Nichols, W. W., Tulkens, P. M., & Van Bambeke, F. (2018). Loss of activity of ceftazidime-avibactam due to MexAB-OprM efflux and overproduction of AmpC cephalosporinase in Pseudomonas aeruginosa isolated from patients suffering from cystic fibrosis. International Journal of Antimicrobial Agents, 52(5), 697–701.
Lin, Y., Song, Z., & Xi, Z. (2021). The anticancer potency of artemisinin and its derivatives. SPR, 1(2), 90–98.
Gupta, S., Kumar, R., Sharma, A., Jindal, S., & Pandav, G. (2021). Role of stem cell in treatment of various dental and systemic diseases. SPR, 1(2), 71–79.
Kaur, G. (2021). Garima. Sharma S, Functional matrix hypothesis: A review of literature, SPR, 1(2), 80–89.
Xu, Y., Zhang, Y., Zheng, X., Yu, K., Sun, Y., Liao, W., Jia, H., Xu, C., Zhou, T., & Shen, M. (2021). The prevalence and functional characteristics of CrpP-like in Pseudomonas aeruginosa isolates from China. European Journal of Clinical Microbiology and Infectious Diseases, 40(12), 2651–2656.
Garg, H. (2021). Digital twin technology: Revolutionary to improve personalized healthcare. SPR, 1(1), 32–34.
Author information
Authors and Affiliations
Contributions
All authors have contributed equally to this manuscript.
Corresponding author
Ethics declarations
Ethical Approval
The Institutional Ethical Committees of Chengdu Medical College has approved the study.
Consent to Participate
Not applicable.
Consent to Publish
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lu, Q., Yang, Q. Study on the Mechanism of Levofloxacin Combined with Imipenem Against Pseudomonas aeruginosa. Appl Biochem Biotechnol 196, 690–700 (2024). https://doi.org/10.1007/s12010-023-04516-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12010-023-04516-8