Abstract
Background
The incidence and injury patterns of open fractures of the proximal ulna are poorly elucidated and little evidence exists to guide management.
Questions/purposes
The purpose of this study was to compare the (1) bony injury patterns; (2) range of motion (ROM) and frequency of union; and (3) postoperative complications between open and closed fractures of the proximal ulna.
Methods
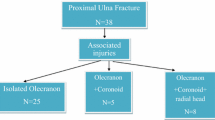
Seventy-nine consecutive open fractures of the proximal ulna were identified. After excluding fracture-dislocations, penetrating injuries, and pediatric injuries, 60 were compared in a retrospective case-control study with an age- and sex-matched group of 91 closed fractures to compare the bony injury patterns based on radiographic review. In a subset of 39 open and 39 closed fractures with sufficient followup, chart and radiographic review was performed by someone other than the operating surgeon to compare differences in final ROM, union, and postoperative complication rates at a minimum followup of 3 months (mean, 22 and 15 months; range, 3–86 months and 3–51 months for open and closed fractures, respectively). A total of 12% of the fractures were open (79 of 671) at the three study centers, and the majority of fractures were intraarticular (45 of 60 [75%]) with Gustilo-Anderson Type I and II wounds (54 of 60 [90%]).
Results
Overall, open fractures of the proximal ulna overall did not have more complex bony injury patterns, but there were more anterior olecranon fracture-dislocations among the open fracture group (nine of 60 [15%] versus two of 91 [2%]; p = 0.004) and more posterior olecranon fracture-dislocations in the closed fracture group (31 of 91 [34%] versus seven of 60 [12%]; p = 0.002). Final ROM was not different in both groups and all fractures healed. There was no difference in wound infection rate but a higher secondary procedure rate among open fractures of the proximal ulna (39% versus 23%, p = 0.014).
Conclusions
In contrast to open fractures of the distal humerus, open fractures of the proximal ulna present with mild soft tissue injuries and do not have more complex bony injury patterns than closed fractures. Our findings suggest that open fractures of the proximal ulna are the result of tension failure of the skin secondary to the limited soft tissue envelope around the proximal ulna. Open fractures of the proximal ulna should be regarded as relatively mild injuries that are not different in severity and prognosis compared with closed fractures.
Level of Evidence
Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence
Similar content being viewed by others
References
Abrams GD, Bellino MJ, Cheung EV. Risk factors for development of heterotopic ossification of the elbow after fracture fixation. J Shoulder Elbow Surg. 2012;21:1550–1554.
Bell J-E, Leung BC, Spratt KF, Koval KJ, Weinstein JD, Goodman DC, Tosteson ANA. Trends and variation in incidence, surgical treatment, and repeat surgery of proximal humeral fractures in the elderly. J Bone Joint Surg Am. 2011;93:121–131.
Chaudhary S, Patil N, Bagaria V, Harshavardhan NS, Hussain N. Open intercondylar fractures of the distal humerus: Management using a mini-external fixator construct. J Shoulder Elbow Surg. 2008;17:465–470.
Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am. 2001;26:908–915.
Court-Brown CM, Bugler KE, Clement ND, Duckworth AD, McQueen MM. The epidemiology of open fractures in adults. A 15-year review. Injury. 2012;43:891–897.
Court-Brown CM, Rimmer S, Prakash U, McQueen MM. The epidemiology of open long bone fractures. Injury. 1998;29:529–534.
Dellinger EP, Miller SD, Wertz MJ, Grypma M, Droppert B, Anderson PA. Risk of infection after open fracture of the arm or leg. Arch Surg. 1988;123:1320–1327.
Duckworth AD, Clement ND, Aitken SA, Court-Brown CM, McQueen MM. The epidemiology of fractures of the proximal ulna. Injury. 2012;43:343–346.
Lennarson PJ, Mostafavi H, Traynelis VC, Walters BC. Management of type II dens fractures: a case-control study. Spine. 2000;25:1234–1237.
McKee MD, Kim J, Kebaish K, Stephen DJ, Kreder HJ, Schemitsch EH. Functional outcome after open supracondylar fractures of the humerus. The effect of the surgical approach. J Bone Joint Surg Br. 2000;82:646–651.
Min W, Anwar A, Ding BC, Tejwani NC. Open distal humerus fractures—review of the literature. Bull NYU Hosp Jt Dis. 2010;68:257–261.
Min W, Ding BC, Tejwani NC. Comparative functional outcome of AO/OTA type C distal humerus fractures: open injuries do worse than closed fractures. J Trauma Acute Care Surg. 2012;72:E27–32.
Mostafavi HR, Tornetta P 3rd. Open fractures of the humerus treated with external fixation. Clin Orthop Relat Res. 1997;337:187–197.
Rouleau DM, Sandman E, van Riet R, Galatz LM. Management of fractures of the proximal ulna. J Am Acad Orthop Surg. 2013;21:149–160.
Sahajpal D, Wright TW. Proximal ulna fractures. J Hand Surg Am. 2009;34:357–362.
Acknowledgments
We thank David Ring MD, PhD for his guidance in study design and data analysis.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Boston University Medical Center, Boston, MA, USA, and Partners Healthcare, Brigham and Women’s and Massachusetts General Hospital, Boston, MA, USA.
About this article
Cite this article
Yi, P.H., Weening, A.A., Shin, S.R. et al. Injury Patterns and Outcomes of Open Fractures of the Proximal Ulna Do Not Differ From Closed Fractures. Clin Orthop Relat Res 472, 2100–2104 (2014). https://doi.org/10.1007/s11999-014-3489-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-014-3489-x