Abstract
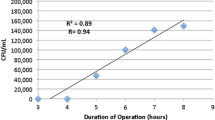
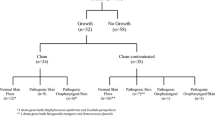
Various guidelines have been proposed regarding which portions of a surgical gown may be considered sterile. Unfortunately, the validity of these recommendations has not been definitively established. We therefore evaluated gown sterility after major spinal surgery to assess the legitimacy of these guidelines. We used sterile culture swabs to obtain samples of gown fronts at 6-inch increments and at the elbow creases of 50 gowns at the end of 29 spinal operations. Another 50 gowns were swabbed immediately after they were applied to serve as negative controls. Bacterial growth was assessed using semiquantitative plating techniques on a nonselective, broad-spectrum media. Contamination was observed at all locations of the gown with rates ranging from 6% to 48%. Compared with the negative controls, the contamination rates were greater at levels 24 inches or less and 48 inches or more relative to the ground and at the elbow creases. The section between the chest and operative field had the lowest contamination rates. Based on these results, we consider the region between the chest and operative field to be the most sterile and any contact with the gown outside this area, including the elbow creases, should be avoided to reduce the risk of infection.


Similar content being viewed by others
References
Al-Maiyah M, Bajwa A, Mackenney P, Port A, Gregg PJ, Hill D, Finn P. Glove perforation and contamination in primary total hip arthroplasty. J Bone Joint Surg Br. 2005;87:556–559.
AORN Recommended Practices Committee. Recommended practices for maintaining a sterile field. AORN J. 2006;83:402–404, 407–410, 413–416.
Boess-Lott R, Stecik S. The Ophthalmic Surgical Assistant. 1st Ed. Thorofare, NJ: Slack Inc; 1999.
Boots RJ, Howe S, George N, Harris FM, Faoagali J. Clinical utility of hygroscopic heat and moisture exchangers in intensive care patients. Crit Care Med. 1997;25:1707–1712.
Davis N, Curry A, Gambhir AK, Panigrahi H, Walker CR, Wilkins EG, Worsley MA, Kay PR. Intraoperative bacterial contamination in operations for joint replacement. J Bone Joint Surg Br. 1999;81:886–889.
Eckersley JR, Williamson DM. Glove punctures in an orthopaedic trauma unit. Injury. 1990;21:177–178.
Ellner PD, Stoessel CJ, Drakeford E, Vasi F. A new culture medium for medical bacteriology. Am J Clin Pathol. 1966;45:502–504.
Fang A, Hu SS, Endres N, Bradford DS. Risk factors for infection after spinal surgery. Spine. 2005;30:1460–1465.
Granzow JW, Smith JW, Nichols RL, Waterman RS, Muzik AC. Evaluation of the protective value of hospital gowns against blood strike-through and methicillin-resistant Staphylococcus aureus penetration. Am J Infect Control. 1998;26:85–93.
Greenough CG. An investigation into contamination of operative suction. J Bone Joint Surg Br. 1986;68:151–153.
Herruzo-Cabrera R, Vizcaino-Alcaide MJ, Pinedo-Castillo C, Rey-Calero J. Diagnosis of local infection of a burn by semiquantitative culture of the eschar surface. J Burn Care Rehabil. 1992;13:639–641.
Hussein JR, Villar RN, Gray AJ, Farrington M. Use of light handles in the laminar flow operating theatre: is it a cause of bacterial concern? Ann R Coll Surg Engl. 2001;83:353–354.
Keller RB, Pappas AM. Infection after spinal fusion using internal fixation instrumentation. Orthop Clin North Am. 1972;3:99–111.
Linares J, Dominguez MA, Martin R. Current laboratory techniques in the diagnosis of catheter-related infections. Nutrition. 1997;13(4 suppl):10S–14S.
Maffulli N, Capasso G, Testa V. Glove perforation in pediatric orthopaedic surgery. J Pediatr Orthop. 1991;11:25–27.
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for Prevention of Surgical Site Infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control. 1999;27:97–132; quiz 133–134; discussion 96.
Massie JB, Heller JG, Abitbol JJ, McPherson D, Garfin SR. Postoperative posterior spinal wound infections. Clin Orthop Relat Res. 1992;284:99–108.
Mills SJ, Holland DJ, Hardy AE. Operative field contamination by the sweating surgeon. Aust N Z J Surg. 2000;70:837–839.
Pissiotis CA, Komborozos V, Papoutsi C, Skrekas G. Factors that influence the effectiveness of surgical gowns in the operating theatre. Eur J Surg. 1997;163:597–604.
Ritter MA. Surgical wound environment. Clin Orthop Relat Res. 1984;190:11–13.
Ritter MA, French ML, Hart JB. Microbiological studies in a horizontal wall-less laminar air-flow operating room during actual surgery. Clin Orthop Relat Res. 1973;97:16–18.
Robinson AH, Drew S, Anderson J, Bentley G, Ridgway GL. Suction tip contamination in the ultraclean-air operating theatre. Ann R Coll Surg Engl. 1993;75:254–256.
Sankar B, Ray P, Rai J. Suction drain tip culture in orthopaedic surgery: a prospective study of 214 clean operations. Int Orthop. 2004;28:311–314.
Schultz RB, Probe RA, Holmes GP. Contamination risks from a high-speed bone burr. Spine. 1996;21:1796–1797.
Spry C. Essentials of Perioperative Nursing. 2nd Ed. Gaithersburg, MD: Aspen Publishers; 1997.
Thanni LO, Yinusa W. Incidence of glove failure during orthopedic operations and the protective effect of double gloves. J Natl Med Assoc. 2003;95:1184–1188.
Weinstein MA, McCabe JP, Cammisa FP Jr. Postoperative spinal wound infection: a review of 2,391 consecutive index procedures. J Spinal Disord. 2000;13:422–426.
Whalan C. Assisting at Surgical Operations: A Practical Guide. Cambridge, UK: Cambridge University Press; 2006.
Wimmer C, Gluch H, Franzreb M, Ogon M. Predisposing factors for infection in spine surgery: a survey of 850 spinal procedures. J Spinal Disord. 1998;11:124–128.
Yinusa W, Li YH, Chow W, Ho WY, Leong JC. Glove punctures in orthopaedic surgery. Int Orthop. 2004;28:36–39.
Acknowledgments
We thank Debbie Callan and Patty Farrel for invaluable assistance with microbiology techniques.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research.
About this article
Cite this article
Bible, J.E., Biswas, D., Whang, P.G. et al. Which Regions of the Operating Gown Should be Considered Most Sterile?. Clin Orthop Relat Res 467, 825–830 (2009). https://doi.org/10.1007/s11999-008-0341-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-008-0341-1