Abstract
Purpose of Review
This paper will review the importance of fever in patients with acute brain injury admitted to the neurologic critical care unit, the common etiologies of fever, and how to manage it.
Recent Findings
Fever’s negative impact on the outcome of patients with acute brain injury due to various etiologies is well cemented in the literature. There are numerous etiologies for fever that can be divided into infectious and non-infectious etiologies. It is important to investigate incidents of fever appropriately to avoid any major infectious complications. Recent advances in technology provided clinicians ways to measure and control fever precisely and consistently to mitigate secondary brain injury with a feedback computerized mechanism such as surface and intravascular cooling targeted management systems. Subsequently, shivering may complicate fever management which might lead to worsen outcomes in brain-injured patients. Therefore, monitoring for shivering with proper therapy should be instated while continuously monitoring and treating fever.
Summary
Fever adds insult to injury in critically ill patients admitted to the neurologic critical care unit. It is important to investigate the etiology, treat the source, and proactively control fever and shivering to avoid worse outcomes.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
O’Grady NP, Barie PS, Bartlett JG, Bleck T, Carroll K, Kalil AC, et al. Guidelines for evaluation of new fever in critically ill adult patients: 2008 update from the American College of Critical Care Medicine and the Infectious Diseases Society of America. Crit Care Med. 2008;36(4):1330–49. https://doi.org/10.1097/CCM.0b013e318169eda9.
Laupland KB, Shahpori R, Kirkpatrick AW, Ross T, Gregson DB, Stelfox HT. Occurrence and outcome of fever in critically ill adults. Crit Care Med. 2008;36(5):1531–5. https://doi.org/10.1097/CCM.0b013e318170efd3.
Commichau C, Scarmeas N, Mayer SA. Risk factors for fever in the neurologic intensive care unit. Neurology. 2003;60(5):837–41. https://doi.org/10.1212/01.wnl.0000047344.28843.eb.
Stocchetti N, Rossi S, Zanier ER, Colombo A, Beretta L, Citerio G. Pyrexia in head-injured patients admitted to intensive care. Intensive Care Med. 2002;28(11):1555–62. https://doi.org/10.1007/s00134-002-1513-1.
Diringer MN, Reaven NL, Funk SE, Uman GC. Elevated body temperature independently contributes to increased length of stay in neurologic intensive care unit patients. Crit Care Med. 2004;32(7):1489–95. https://doi.org/10.1097/01.ccm.0000129484.61912.84.
Kilpatrick MM, Lowry DW, Firlik AD, Yonas H, Marion DW. Hyperthermia in the neurosurgical intensive care unit. Neurosurgery. 2000;47(4):850–5; discussion 5–6. https://doi.org/10.1097/00006123-200010000-00011.
Rincon F, Patel U, Schorr C, Lee E, Ross S, Dellinger RP, et al. Brain injury as a risk factor for fever upon admission to the intensive care unit and association with in-hospital case fatality: a matched cohort study. J Intensive Care Med. 2015;30(2):107–14. https://doi.org/10.1177/0885066613508266.
Erickson RS, Kirklin SK. Comparison of ear-based, bladder, oral, and axillary methods for core temperature measurement. Crit Care Med. 1993;21(10):1528–34. https://doi.org/10.1097/00003246-199310000-00022.
Erickson RS, Meyer LT. Accuracy of infrared ear thermometry and other temperature methods in adults. Am J Crit Care. 1994;3(1):40–54.
Schmitz T, Bair N, Falk M, Levine C. A comparison of five methods of temperature measurement in febrile intensive care patients. Am J Crit Care. 1995;4(4):286–92.
Lefrant JY, Muller L, de La Coussaye JE, Benbabaali M, Lebris C, Zeitoun N, et al. Temperature measurement in intensive care patients: comparison of urinary bladder, oesophageal, rectal, axillary, and inguinal methods versus pulmonary artery core method. Intensive Care Med. 2003;29(3):414–8. https://doi.org/10.1007/s00134-002-1619-5.
•• Picetti E, Oddo M, Prisco L, Helbok R, Taccone FS. A survey on fever monitoring and management in patients with acute brain injury: the SUMMA study. J Neurosurg Anesthesiol. 2019;31(4):399–405. https://doi.org/10.1097/ANA.0000000000000536. This is a world-wide survey on fever monitoring and management of patients with acute brain injury highlighting the substantial variability of fever definition, how to measure it and how to treat it.
Fallis WM. Monitoring urinary bladder temperature in the intensive care unit: state of the science. Am J Crit Care. 2002;11(1):38–45; quiz 7.
Cunha BA. Clinical approach to fever in the neurosurgical intensive care unit: focus on drug fever. Surg Neurol Int. 2013;4(Suppl 5):S318–22. https://doi.org/10.4103/2152-7806.111432.
Marik PE. Fever in the ICU. Chest. 2000;117(3):855–69. https://doi.org/10.1378/chest.117.3.855.
Oliveira-Filho J, Ezzeddine MA, Segal AZ, Buonanno FS, Chang Y, Ogilvy CS, et al. Fever in subarachnoid hemorrhage: relationship to vasospasm and outcome. Neurology. 2001;56(10):1299–304. https://doi.org/10.1212/wnl.56.10.1299.
Savage KE, Oleson CV, Schroeder GD, Sidhu GS, Vaccaro AR. Neurogenic fever after acute traumatic spinal cord injury: a qualitative systematic review. Global Spine J. 2016;6(6):607–14. https://doi.org/10.1055/s-0035-1570751.
Thompson HJ. Evidence-base for fever interventions following stroke. Stroke. 2015;46(5):e98–100. https://doi.org/10.1161/STROKEAHA.115.008188.
Hocker SE, Tian L, Li G, Steckelberg JM, Mandrekar JN, Rabinstein AA. Indicators of central fever in the neurologic intensive care unit. JAMA Neurol. 2013;70(12):1499–504. https://doi.org/10.1001/jamaneurol.2013.4354.
Rabinstein AA, Sandhu K. Non-infectious fever in the neurological intensive care unit: incidence, causes and predictors. J Neurol Neurosurg Psychiatry. 2007;78(11):1278–80. https://doi.org/10.1136/jnnp.2006.112730.
O’Grady NP, Barie PS, Bartlett JG, Bleck T, Garvey G, Jacobi J, et al. Practice guidelines for evaluating new fever in critically ill adult patients. Task Force of the Society of Critical Care Medicine and the Infectious Diseases Society of America. Clin Infect Dis. 1998;26(5):1042–59. https://doi.org/10.1086/520308.
Albrich WC, Dusemund F, Bucher B, Meyer S, Thomann R, Kuhn F, et al. Effectiveness and safety of procalcitonin-guided antibiotic therapy in lower respiratory tract infections in “real life”: an international, multicenter poststudy survey (ProREAL). Arch Intern Med. 2012;172(9):715–22. https://doi.org/10.1001/archinternmed.2012.770.
Rello J, Ollendorf DA, Oster G, Vera-Llonch M, Bellm L, Redman R, et al. Epidemiology and outcomes of ventilator-associated pneumonia in a large US database. Chest. 2002;122(6):2115–21. https://doi.org/10.1378/chest.122.6.2115.
•• Abulhasan YB, Rachel SP, Chatillon-Angle MO, Alabdulraheem N, Schiller I, Dendukuri N, et al. Healthcare-associated infections in the neurological intensive care unit: results of a 6-year surveillance study at a major tertiary care center. Am J Infect Control. 2018;46(6):656–62. https://doi.org/10.1016/j.ajic.2017.12.001. This is a prospective large scale surveillance study over a 6 years period looking at healthcare-associated infections in a neurological intensive care units providing estimated risk of common healthcare associated infections in neurocritical care patients and effect on hospitalization.
Rello J, Ausina V, Ricart M, Puzo C, Net A, Prats G. Nosocomial pneumonia in critically ill comatose patients: need for a differential therapeutic approach. Eur Respir J. 1992;5(10):1249–53.
Abulhasan YB, Abdullah AA, Shetty SA, Ramadan MA, Yousef W, Mokaddas EM. Health care-associated infections in a neurocritical care unit of a developing country. Neurocrit Care. 2020;32(3):836–46. https://doi.org/10.1007/s12028-019-00856-8.
Tay L, Ong PL, Lang L. Nosocomial infections in a neurosurgery department. Ann Acad Med Singap. 1987;16(4):565–70.
Hinduja A, Dibu J, Achi E, Patel A, Samant R, Yaghi S. Nosocomial infections in patients with spontaneous intracerebral hemorrhage. Am J Crit Care. 2015;24(3):227–31. https://doi.org/10.4037/ajcc2015422.
Kalil AC, Metersky ML, Klompas M, Muscedere J, Sweeney DA, Palmer LB, et al. Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 clinical practice guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016;63(5):e61–111. https://doi.org/10.1093/cid/ciw353.
Chen C, Zhang B, Yu S, Sun F, Ruan Q, Zhang W, et al. The incidence and risk factors of meningitis after major craniotomy in China: a retrospective cohort study. PLoS ONE. 2014;9(7). https://doi.org/10.1371/journal.pone.0101961.
Kourbeti IS, Vakis AF, Ziakas P, Karabetsos D, Potolidis E, Christou S, et al. Infections in patients undergoing craniotomy: risk factors associated with post-craniotomy meningitis. J Neurosurg. 2015;122(5):1113–9. https://doi.org/10.3171/2014.8.JNS132557.
Arabi Y, Memish ZA, Balkhy HH, Francis C, Ferayan A, Al Shimemeri A, et al. Ventriculostomy-associated infections: incidence and risk factors. Am J Infect Control. 2005;33(3):137–43. https://doi.org/10.1016/j.ajic.2004.11.008.
Tunkel AR, Hasbun R, Bhimraj A, Byers K, Kaplan SL, Scheld WM, et al. 2017 Infectious Diseases Society of America’s clinical practice guidelines for healthcare-associated ventriculitis and meningitis. Clin Infect Dis. 2017;64(6):e34–65. https://doi.org/10.1093/cid/ciw861.
Deshpande A, Pasupuleti V, Thota P, Pant C, Rolston DD, Sferra TJ, et al. Community-associated Clostridium difficile infection and antibiotics: a meta-analysis. J Antimicrob Chemother. 2013;68(9):1951–61. https://doi.org/10.1093/jac/dkt129.
Loo VG, Bourgault AM, Poirier L, Lamothe F, Michaud S, Turgeon N, et al. Host and pathogen factors for Clostridium difficile infection and colonization. N Engl J Med. 2011;365(18):1693–703. https://doi.org/10.1056/NEJMoa1012413.
Surawicz CM, Brandt LJ, Binion DG, Ananthakrishnan AN, Curry SR, Gilligan PH, et al. Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infections. Am J Gastroenterol. 2013;108(4):478–98; quiz 99. https://doi.org/10.1038/ajg.2013.4.
Zinreich SJ. Rhinosinusitis: radiologic diagnosis. Otolaryngol Head Neck Surg. 1997;117(3 Pt 2):S27-34. https://doi.org/10.1016/s0194-5998(97)70004-4.
Johnson DH, Cunha BA. Drug fever. Infect Dis Clin North Am. 1996;10(1):85–91. https://doi.org/10.1016/s0891-5520(05)70287-7.
Caroff SN, Mann SC. Neuroleptic malignant syndrome and malignant hyperthermia. Anaesth Intensive Care. 1993;21(4):477–8.
Barba R, Di Micco P, Blanco-Molina A, Delgado C, Cisneros E, Villalta J, et al. Fever and deep venous thrombosis. Findings from the RIETE registry. J Thromb Thrombolysis. 2011;32(3):288–92. https://doi.org/10.1007/s11239-011-0604-7.
Chalouhi N, Daou B, Rincon F, Montano M, Kent A, Barkley K, et al. Risk of venous thromboembolism in patients with large hemispheric infarction undergoing decompressive hemicraniectomy. Neurocrit Care. 2016;25(1):105–9. https://doi.org/10.1007/s12028-016-0252-z.
Goldstein JN, Fazen LE, Wendell L, Chang Y, Rost NS, Snider R, et al. Risk of thromboembolism following acute intracerebral hemorrhage. Neurocrit Care. 2009;10(1):28–34. https://doi.org/10.1007/s12028-008-9134-3.
Kim KS, Brophy GM. Symptomatic venous thromboembolism: incidence and risk factors in patients with spontaneous or traumatic intracranial hemorrhage. Neurocrit Care. 2009;11(1):28–33. https://doi.org/10.1007/s12028-009-9201-4.
Orlando R 3rd, Gleason E, Drezner AD. Acute acalculous cholecystitis in the critically ill patient. Am J Surg. 1983;145(4):472–6. https://doi.org/10.1016/0002-9610(83)90042-9.
Meyfroidt G, Baguley IJ, Menon DK. Paroxysmal sympathetic hyperactivity: the storm after acute brain injury. Lancet Neurol. 2017;16(9):721–9. https://doi.org/10.1016/S1474-4422(17)30259-4.
•• Greer DM, Ritter J, Helbok R, Badjatia N, Ko SB, Guanci M, et al. Impact of fever prevention in brain-injured patients (INTREPID): study protocol for a randomized controlled trial. Neurocrit Care. 2021;35(2):577–89. https://doi.org/10.1007/s12028-021-01208-1. INTREPID is an ongoing prospective randomized open blinded endpoint study of fever prevention versus standard usual care in patients with stroke based on intention-t- treat population
Vaity C, Al-Subaie N, Cecconi M. Cooling techniques for targeted temperature management post-cardiac arrest. Crit Care. 2015;19:103. https://doi.org/10.1186/s13054-015-0804-1.
Mackowiak PA. Concepts of fever. Arch Intern Med. 1998;158(17):1870–81. https://doi.org/10.1001/archinte.158.17.1870.
•• Picetti E, Minardi F, Rossi S. How to manage fever in brain-injured patients. Minerva Anestesiol. 2020;86(1):88–94. https://doi.org/10.23736/S0375-9393.19.13901-6. This is a review by Picetti et al on how to measure fever in patients with brain injury and suggest treatment modalities.
Kasner SE, Wein T, Piriyawat P, Villar-Cordova CE, Chalela JA, Krieger DW, et al. Acetaminophen for altering body temperature in acute stroke: a randomized clinical trial. Stroke. 2002;33(1):130–4. https://doi.org/10.1161/hs0102.101477.
Koennecke HC, Leistner S. Prophylactic antipyretic treatment with acetaminophen in acute ischemic stroke: a pilot study. Neurology. 2001;57(12):2301–3. https://doi.org/10.1212/wnl.57.12.2301.
Peacock WF, Breitmeyer JB, Pan C, Smith WB, Royal MA. A randomized study of the efficacy and safety of intravenous acetaminophen compared to oral acetaminophen for the treatment of fever. Acad Emerg Med. 2011;18(4):360–6. https://doi.org/10.1111/j.1553-2712.2011.01043.x.
•• Ianosi B, Rass V, Gaasch M, Huber L, Lindner A, Hackl WO, et al. An observational study on the use of intravenous non-opioid analgesics and antipyretics in poor-grade subarachnoid hemorrhage: effects on hemodynamics and systemic and brain temperature. Ther Hypothermia Temp Manag. 2020;10(1):27–36. https://doi.org/10.1089/ther.2018.0046. Ianosi et al conducted an observational study on the effect of IV NSAIDs and non-opioids analgesics including paracetamol, diclofenac and metamizole on cerebral hemodynamics and temperature for febrile for patients with poor grade SAH, showing common hemodynamic side effects with increase in use of vasopressor support in both febrile and non-febrile patients.
Picetti E, De Angelis A, Villani F, Antonini MV, Rossi I, Servadei F, et al. Intravenous paracetamol for fever control in acute brain injury patients: cerebral and hemodynamic effects. Acta Neurochir (Wien). 2014;156(10):1953–9; discussion 9. https://doi.org/10.1007/s00701-014-2129-2.
Morris PE, Promes JT, Guntupalli KK, Wright PE, Arons MM. A multi-center, randomized, double-blind, parallel, placebo-controlled trial to evaluate the efficacy, safety, and pharmacokinetics of intravenous ibuprofen for the treatment of fever in critically ill and non-critically ill adults. Crit Care. 2010;14(3):R125. https://doi.org/10.1186/cc9089.
Picetti E, Servadei F, Reverberi C, De Carlo F, Rossi I, Antonini MV, et al. Low-dose intramuscular diclofenac sodium for fever control in acute brain injury. World Neurosurg. 2016;95:241–5. https://doi.org/10.1016/j.wneu.2016.08.032.
Schiefecker AJ, Pfausler B, Beer R, Sohm F, Sabo J, Knauseder V, et al. Parenteral diclofenac infusion significantly decreases brain-tissue oxygen tension in patients with poor-grade aneurysmal subarachnoid hemorrhage. Crit Care. 2013;17(3):R88. https://doi.org/10.1186/cc12714.
Cormio M, Citerio G, Spear S, Fumagalli R, Pesenti A. Control of fever by continuous, low-dose diclofenac sodium infusion in acute cerebral damage patients. Intensive Care Med. 2000;26(5):552–7. https://doi.org/10.1007/s001340051203.
Cormio M, Citerio G. Continuous low dose diclofenac sodium infusion to control fever in neurosurgical critical care. Neurocrit Care. 2007;6(2):82–9. https://doi.org/10.1007/s12028-007-0002-3.
Palmer JD, Sparrow OC, Iannotti F. Postoperative hematoma: a 5-year survey and identification of avoidable risk factors. Neurosurgery. 1994;35(6):1061–4; discussion 4–5. https://doi.org/10.1227/00006123-199412000-00007.
Moore N, Salvo F, Duong M, Blin P, Pariente A. Cardiovascular risks associated with low-dose ibuprofen and diclofenac as used OTC. Expert Opin Drug Saf. 2014;13(2):167–79. https://doi.org/10.1517/14740338.2014.846324.
Morgan SP. A comparison of three methods of managing fever in the neurologic patient. J Neurosci Nurs. 1990;22(1):19–24. https://doi.org/10.1097/01376517-199002000-00006.
O’Donnell J, Axelrod P, Fisher C, Lorber B. Use and effectiveness of hypothermia blankets for febrile patients in the intensive care unit. Clin Infect Dis. 1997;24(6):1208–13. https://doi.org/10.1086/513660.
Badjatia N, Bodock M, Guanci M, Rordorf GA. Rapid infusion of cold saline (4 degrees C) as adjunctive treatment of fever in patients with brain injury. Neurology. 2006;66(11):1739–41. https://doi.org/10.1212/01.wnl.0000218166.54150.0a.
Sonder P, Janssens GN, Beishuizen A, Henry CL, Rittenberger JC, Callaway CW, et al. Efficacy of different cooling technologies for therapeutic temperature management: a prospective intervention study. Resuscitation. 2018;124:14–20. https://doi.org/10.1016/j.resuscitation.2017.12.026.
Mayer SA, Kowalski RG, Presciutti M, Ostapkovich ND, McGann E, Fitzsimmons BF, et al. Clinical trial of a novel surface cooling system for fever control in neurocritical care patients. Crit Care Med. 2004;32(12):2508–15. https://doi.org/10.1097/01.ccm.0000147441.39670.37.
Diringer MN, Neurocritical Care Fever Reduction Trial G. Treatment of fever in the neurologic intensive care unit with a catheter-based heat exchange system. Crit Care Med. 2004;32(2):559–64. https://doi.org/10.1097/01.CCM.0000108868.97433.3F.
Andrews PJD, Verma V, Healy M, Lavinio A, Curtis C, Reddy U, et al. Targeted temperature management in patients with intracerebral haemorrhage, subarachnoid haemorrhage, or acute ischaemic stroke: consensus recommendations. Br J Anaesth. 2018;121(4):768–75. https://doi.org/10.1016/j.bja.2018.06.018.
Madden LK, Hill M, May TL, Human T, Guanci MM, Jacobi J, et al. The implementation of targeted temperature management: an evidence-based guideline from the Neurocritical Care Society. Neurocrit Care. 2017;27(3):468–87. https://doi.org/10.1007/s12028-017-0469-5.
•• Ferreira RES, de Paiva BLC, de Freitas FGR, Machado FR, Silva GS, Raposo RM, et al. Efficacy and safety of a nasopharyngeal catheter for selective brain cooling in patients with traumatic brain injury: a prospective, non-randomized pilot study. Neurocrit Care. 2021;34(2):581–92. https://doi.org/10.1007/s12028-020-01052-9. This prospective non-randomized pilot trial tested the use of a novel nasopharyngeal catheter in patients with traumatic brain injury showing its safety and efficacy by providing selective cooling.
•• Badjatia N, Gupta N, Sanchez S, Haymore J, Tripathi H, Shah R, et al. Safety and feasibility of a novel transnasal cooling device to induce normothermia in febrile cerebrovascular patients. Neurocrit Care. 2021;34(2):500–7. https://doi.org/10.1007/s12028-020-01044-9. This is a single center safety and feasbility study of a novel transnasal cooling device to induce and maintain normothermia in ischemic and hemorrhagic stroke patients. Authors found it to be safe and feasibile without significant shivering, paving the way for a multicenter trial.
Alfonsi P. Postanaesthetic shivering. Epidemiology, pathophysiology and approaches to prevention and management. Minerva Anestesiol. 2003;69(5):438–42.
Ciofolo MJ, Clergue F, Devilliers C, Ben Ammar M, Viars P. Changes in ventilation, oxygen uptake, and carbon dioxide output during recovery from isoflurane anesthesia. Anesthesiology. 1989;70(5):737–41. https://doi.org/10.1097/00000542-198905000-00004.
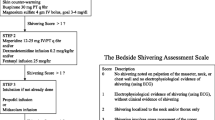
Badjatia N, Strongilis E, Gordon E, Prescutti M, Fernandez L, Fernandez A, et al. Metabolic impact of shivering during therapeutic temperature modulation: the Bedside Shivering Assessment Scale. Stroke. 2008;39(12):3242–7. https://doi.org/10.1161/STROKEAHA.108.523654.
Olson DM, Grissom JL, Williamson RA, Bennett SN, Bellows ST, James ML. Interrater reliability of the bedside shivering assessment scale. Am J Crit Care. 2013;22(1):70–4. https://doi.org/10.4037/ajcc2013907.
Badjatia N, Strongilis E, Prescutti M, Fernandez L, Fernandez A, Buitrago M, et al. Metabolic benefits of surface counter warming during therapeutic temperature modulation. Crit Care Med. 2009;37(6):1893–7. https://doi.org/10.1097/CCM.0b013e31819fffd3.
De Witte J, Sessler DI. Perioperative shivering: physiology and pharmacology. Anesthesiology. 2002;96(2):467–84. https://doi.org/10.1097/00000542-200202000-00036.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Jamil R. Dibu declares that he has no conflict of interest. Rehan Haque declares that he has no conflict of interest. Samer Shoshan declares that he has no conflict of interest. Yasser B. Abulhasan declares that he has no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of Topical Collection on Critical Care Neurology
Rights and permissions
About this article
Cite this article
Dibu, J.R., Haque, R., Shoshan, S. et al. Treatment of Fever in Neurologically Critically Ill Patients. Curr Treat Options Neurol 24, 515–531 (2022). https://doi.org/10.1007/s11940-022-00732-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11940-022-00732-5