Opinion statement
Obstructive sleep apnea (OSA) is the most common sleep-related breathing disorder characterized by repetitive episodes of complete or partial obstruction of the upper airway. The prevalence of this disorder is strictly dependent on its gravity. At ≥15 events/h apnea–hypopnea index (AHI), it ranges from 6 to 17% in the general population, with higher rates in men and increasing with age. The hypoxia induced by OSA severely affects the structure and function of blood vessels, culminating in mortality and morbidity. Its negative impact influences also cognitive functioning. Recent papers showed the relationship between OSA and some neurological disorders, such as neurodegenerative diseases, stroke, epilepsy, and headache. OSA may accelerate the onset of mild cognitive impairment and Alzheimer’s disease (AD) and might also represent an independent risk factor for Parkinson’s disease (PD). OSA is also frequent in multisystem atrophy. In the early stages of AD, continuous positive airway pressure (CPAP) treatment might slow down the progression of the disease, thus highlighting the potential importance of OSA screening and a timely intervention in these patients. Moreover, CPAP is effective in reducing daytime sleepiness in PD. OSA may induce seizures by means of sleep disruption and deprivation, as well as cerebral hypoxemia with consequent oxidative stress. It has been demonstrated that CPAP treatment is efficacious in controlling epileptic seizures. OSA can represent a risk factor for stroke and death, mainly related to the endothelial dysfunction, with the formation of atherosclerosis caused by hypoxia through oxidative stress. CPAP treatment in patients with OSA and stroke, if delivered in the early stages, is able to increase the magnitude of neurologic improvement after the vascular accident. There is a strong association between OSA and headache. In particular, there is a “sleep apnea headache” described as a recurrent morning headache, with resolution after effective treatment of sleep apnea. This review clearly shows the importance of taking a sleep history in neurological patients and considering the diagnosis and specific treatment of OSA in these patients.
Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
American Academy of Sleep Medicine. International classification of sleep disorders, 3rd edn. Darien, IL: American Academy of Sleep Medicine.
• Senaratna CV, Perret JL, Lodge CJ, Lowe AJ, Campbell BE, Matheson MC, Hamilton GS, Dharmage SC. Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev. 2016. doi:10.1016/j.smrv.2016.07.002. In this systematic review, the authors pointed out the heterogeneity of methodological approaches in the study investigating the prevalence of OSA in the general population. After taking into account this issue, they concluded that advancing age, male sex, and higher body mass index increase OSA prevalence.
Seneviratne U, Puvanendran K. Excessive daytime sleepiness in obstructive sleep apnea: prevalence, severity, and predictors. Sleep Med. 2004;5:339–43.
Amdo T, Hasaneen N, Gold MS, Gold AR. Somatic syndromes, insomnia, anxiety, and stress among sleep disordered breathing patients. Sleep Breath. 2016;20:759–68.
Harris M, Glozier N, Ratnavadivel R, Grunstein RR. Obstructive sleep apnea and depression. Sleep Med Rev. 2009;13:437–44.
Björnsdóttir E, Benediktsdóttir B, Pack AI, Arnardottir ES, Kuna ST, Gíslason T, et al. The prevalence of depression among untreated obstructive sleep apnea patients using a standardized psychiatric interview. J Clin Sleep Med. 2016;12:105–12.
Lanfranchi P, Somers VA. Obstructive sleep apnea and vascular disease. Respir Res. 2001;2:315–9.
Stranks EK, Crowe SF. The cognitive effects of obstructive sleep apnea: an updated meta-analysis. Arch Clin Neuropsychol. 2016;3:186–93.
Gaig C, Iranzo A. Sleep-disordered breathing in neurodegenerative diseases. Curr Neurol Neurosci Rep. 2012;12:205–17.
Deak MC, Kirsch DB. Sleep-disordered breathing in neurologic conditions. Clin Chest Med. 2014;35:547–56.
Devita M, Montemurro S, Ramponi S, Marvisi M, Villani D, Raimondi MC, et al. Obstructive sleep apnea and its controversial effects on cognition. J Clin Exp Neuropsychol. 2016;15:1–12.
Batool-Anwar S, Kales SN, Patel SR, Varvarigou V, DeYoung PN, Malhotra A. Obstructive sleep apnea and psychomotor vigilance task performance. Nat Sci Sleep. 2014;6:65–71.
Wallace A, Bucks RS. Memory and obstructive sleep apnea: a meta-analysis. Sleep. 2013;36:203–20.
Bucks RS, Olaithe M, Eastwood P. Neurocognitive function in obstructive sleep apnoea: a meta-review. Respirology. 2013;18:61–70.
• Vaessen TJ, Overeem S, Sitskoorn MM. Cognitive complaints in obstructive sleep apnea. Sleep Med Rev. 2015;19:51–8. In this review, the authors investigated the presence and the impact of subjective cognitive deficits in OSA patients, identifying concentration complaints as the most representative and deleterious for quality of life in these patients.
Dewan NA, Nieto FJ, Somers VK. Intermittent hypoxemia and OSA: implications for comorbidities. Chest. 2015;147:266–74.
Ferini-Strambi L, Marelli S, Galbiati A, Castronovo C. Effects of continuous positive airway pressure on cognition and neuroimaging data in sleep apnea. Int J Psychophysiol. 2013;89:203–12.
Canessa N, Castronovo V, Cappa SF, Aloia MS, Marelli S, Falini A, et al. Obstructive sleep apnea: brain structural changes and neurocognitive function before and after treatment. Am J Respir Crit Care Med. 2011;183:1419–26.
Garbarino S, Durando P, Guglielmi O, Dini G, Bersi F, Fornarino S, et al. Sleep apnea, sleep debt and daytime sleepiness are independently associated with road accidents. a cross-sectional study on truck drivers. PLoS One. 2016;11:e0166262.
Zhou J, Camacho M, Tang X, Kushida CA. A review of neurocognitive function and obstructive sleep apnea with or without daytime sleepiness. Sleep Med. 2016;23:99–108.
Dostalova S, Susta M, Vorlova T, Sonka K. Sleepiness in patients with obstructive sleep apnoea—daytime course and impact of nocturnal respiratory events. Neuro Endocrinol Lett. 2012;33:684–8.
Jacobsen JH, Shi L, Mokhlesi B. Factors associated with excessive daytime sleepiness in patients with severe obstructive sleep apnea. Sleep Breath. 2013;17:10629–35.
de Castro RJ, Rosales-Mayor E. Clinical and polysomnographic differences between OSAH patients with/without excessive daytime sleepiness. Sleep Breath. 2013;17:1079–86.
Shear TC, Balachandran JS, Mokhlesi B, Spampinato LM, Knutson KL, Meltzer DO, et al. Risk of sleep apnea in hospitalized older patients. J Clin Sleep Med. 2014;10:1061–6.
Sharkey KM, Orff HJ, Tosi C, Harrington D, Roye GD, Millman RP. Subjective sleepiness and daytime functioning in bariatric patients with obstructive sleep apnea. Sleep Breath. 2013;17:1079–86.
•• Osorio RS, Gumb T, Pirraglia E, Varga AW, Lu SE, Lim J, et al. Sleep-disordered breathing advances cognitive decline in the elderly. Neurology. 2015;84:1964–71. The authors found a link between earlier age in cognitive decline and the presence of SDB. Moreover, the utilization of CPAP was recognized as an effective treatment in order to delay the development of cognitive impairment.
Sheu JJ, Lee HC, Lin HC, Kao LT, Chung SD. A 5-year follow-up study on the relationship between obstructive sleep apnea and Parkinson disease. J Clin Sleep Med. 2015;11:1403–8.
Yeh NC, Tien KJ, Yang CM, Wang JJ, Weng SF. Increased risk of Parkinson’s disease in patients with obstructive sleep apnea: a population-based, propensity score-matched, longitudinal follow-up study. Medicine. 2016;95:e2293.
Braley TJ, Kratz AL, Kaplish N, Chervin RD. Sleep and cognitive function in multiple sclerosis. Sleep. 2016;39:1525–33.
• Yaffe K, Falvey CM, Hoang T. Connections between sleep and cognition in older adults. Lancet Neurol. 2014;13:1017–28. In this comprehensive review, the authors identified SDB as a crucial factor that may support the development of cognitive decline in older adults.
Foley DJ, Masaki K, White L, Larkin EK, Monjan A, Redline S. Sleep-disordered breathing and cognitive impairment in elderly Japanese-American men. Sleep. 2003;26:596–9.
O’Hara R, Schröder CM, Kraemer HC, Kryla N, Cao C, Miller E, et al. Nocturnal sleep apnea/hypopnea is associated with lower memory performance in APOE epsilon4 carriers. Neurology. 2005;65:642–4.
Spira AP, Blackwell T, Stone KL, Redline S, Cauley JA, Ancoli-Israel S, et al. Sleep-disordered breathing and cognition in older women. J Am Geriatr Soc. 2008;56:45–50.
Sforza E, Roche F, Thomas-Anterion C, Kerleroux J, Beauchet O, Celle S, et al. Cognitive function and sleep related breathing disorders in a healthy elderly population: the SYNAPSE Study. Sleep. 2010;33:515–21.
Blackwell T, Yaffe K, Ancoli-Israel S, Redline S, Ensrud KE, Stefanick ML, et al. Associations between sleep architecture and sleep-disordered breathing and cognition in older community-dwelling men: the Osteoporotic Fractures in Men Sleep Study. J Am Geriatr Soc. 2011;59:2217–25.
Cohen-Zion M, Stepnowsky C, Johnson S, Marler M, Dimsdale JE, Ancoli-Israel S. Cognitive changes and sleep disordered breathing in elderly: differences in race. J Psychosom Res. 2004;56:549–53.
Ding X, Kryscio RJ, Turner J, Jicha GA, Cooper G, Caban-Holt A, et al. Self-reported sleep apnea and dementia risk: findings from the Prevention of Alzheimer’s Disease with Vitamin E and Selenium trial. J Am Geriatr Soc. 2016;64:2472–8.
Emamian F, Khazaie H, Tahmasian M, Leschziner GD, Morrell MJ, Hsiung GY, et al. The association between obstructive sleep apnea and Alzheimer’s disease: a meta-analysis perspective. Front Aging Neurosci. 2016;8:78.
•• Yaffe K, Laffan AM, Harrison SL, Redline S, Spira AP, Ensrud KE, et al. Sleep-disordered breathing, hypoxia, and risk of mild cognitive impairment and dementia in older women. JAMA. 2011;306:613–9. In this prospective study, the presence of SDB, and not other measures of sleep disruption (arousal index and wake after sleep onset) or duration (total sleep time), increased the risk of developing cognitive impairment in older women.
Pan W, Kastin AJ. Can sleep apnea cause Alzheimer’s disease? Neurosci Biobehav Rev. 2014;47:656–69.
Kaminska M, Lafontaine AL, Kimoff RJ. The interaction between obstructive sleep apnea and Parkinson’s disease: possible mechanisms and implications for cognitive function. Parkinsons Dis. 2015;2015:849472.
Zeng J, Wei M, Li T, Chen W, Feng Y, Shi R, et al. Risk of obstructive sleep apnea in Parkinson’s disease: a meta-analysis. PLoS One. 2013;8:e82091.
Kipp M, Nyamoya S, Hochstrasser T, Amor S. Multiple sclerosis animal models: a clinical and histopathological perspective. Brain Pathol. 2017;27:123–37.
Braley TJ, Segal BM, Chervin RD. Obstructive sleep apnea and fatigue in patients with multiple sclerosis. J Clin Sleep Med. 2014;10:155–62.
• Troussière AC, Charley CM, Salleron J, Richard F, Delbeuck X, Derambure P, et al. Treatment of sleep apnoea syndrome decreases cognitive decline in patients with Alzheimer’s disease. J Neurol Neurosurg Psychiatr. 2014;85:1405–8. This is a pilot study in which the treatment of OSA by means of CPAP was associated with a slower cognitive decline in patients with Alzheimer’s disease in a 3-year follow-up period.
Neikrug AB, Liu L, Avanzino JA, Maglione JE, Natarajan L, Bradley L, et al. Continuous positive airway pressure improves sleep and daytime sleepiness in patients with Parkinson disease and sleep apnea. Sleep. 2014;37:177–85.
Harmell AL, Neikrug AB, Palmer BW, Avanzino JA, Liu L, Maglione JE, et al. Obstructive sleep apnea and cognition in Parkinson’s disease. Sleep Med. 2016;21:28–34.
Iranzo A, Santamaria J, Tolosa E, Vilaseca I, Valldeoriola F, Martí MJ, et al. Long-term effect of CPAP in the treatment of nocturnal stridor in multiple system atrophy. Neurology. 2004;63:930–2.
Ghorayeb I, Yekhlef F, Bioulac B, Tison F. Continuous positive airway pressure for sleep-related breathing disorders in multiple system atrophy: long-term acceptance. Sleep Med. 2005;6:359–62.
Shimohata T, Tomita M, Nakayama H, Aizawa N, Ozawa T, Nishizawa M. Floppy epiglottis as a contraindication of CPAP in patients with multiple system atrophy. Neurology. 2011;76:1841–2.
Shimohata T, Nakayama H, Aizawa N, Nishizawa M. Discontinuation of continuous positive airway pressure treatment in multiple system atrophy. Sleep Med. 2014;15:1147–9.
Manni R, Terzaghi M, Arbasino C, Sartori I, Galimberti CA, Tartara A. Obstructive sleep apnea in a clinical series of adult epilepsy patients: frequency and features of the comorbidity. Epilepsia. 2003;44:836–40.
Foldvary-Schaefer N, Stephenson L, Bingaman W. Resolution of obstructive sleep apnea with epilepsy surgery? Expanding the relationship between sleep and epilepsy. Epilepsia. 2008;49:1457–9.
Cho JW, Kim DJ, Noh KH, et al. Nocturnal frontal lobe epilepsy presenting as obstructive type sleep apnea. J Epilepsy Res. 2011;1:74–6.
Lin Z, Si Q, Xiaoyi Z. Obstructive sleep apnoea in patients with epilepsy: a meta-analysis. Sleep Breath. 2016. doi:10.1007/s11325-016-1391-3
Sharma A, Molano J, Moseley BD. The STOP-BANG questionnaire improves the detection of epilepsy patients at risk for obstructive sleep apnea. Epilepsy Res. 2016;129:37–40.
Cheng S, Stark CD, Stark RJ. Sleep apnoea and the neurologist. Pract Neurol. 2017;17:21–7.
Nguyen-Michel VH, Pallanca O, Navarro V, Dupont S, Baulac M, Adam C. How are epileptic events linked to obstructive sleep apneas in epilepsy? Seizure. 2015;24:121–3.
Li G, Bauer S, Nowak M, Norwood B, Tackenberg B, Rosenow F, et al. Cytokines and epilepsy. Seizure. 2011;20:249–56.
Rowley S, Patel M. Mitochondrial involvement and oxidative stress in temporal lobe epilepsy. Free Radic Biol Med. 2013;62:121–31.
Ebben MR, Sethi NK, Conte M, Pollak CP, Labar D. Vagus nerve stimulation, sleep apnea and CPAP titration. J Clin Sleep Med. 2008;4:471–3.
Eriksson SH. Epilepsy and sleep. Curr Opin Neurol. 2011;24:171–6.
Khachatryan SG, Prosperetti C, Rossinelli A, Pedrazzi P, Agazzi P, Ratti PL, et al. Sleep-onset central apneas as triggers of severe nocturnal seizures. Sleep Med. 2015;16:1017–9.
Pornsriniyom D, Kim HW, Bena J, Andrews ND, Moul D, Foldvary-Schaefer N. Effect of positive airway pressure therapy on seizure control in patients with epilepsy and obstructive sleep apnea. Epilepsy Behav. 2014;37:270–5.
Maurousset A, De Toffol B, Praline J, Biberon J, Limousin N. High incidence of obstructive sleep apnea syndrome in patients with late-onset epilepsy. Neurophysiol Clin. 2017;47:55–61.
Dinkelacker V. Obstructive sleep apnea in drug-resistant epilepsy: a significant comorbidity warranting diagnosis and treatment. Rev Neurol. 2016;172:361–70.
Rutten-Jacobs LC, Arntz RM, Maaijwee NA, Schoonderwaldt HC, Dorresteijn LD, van Dijk EJ, et al. Long-term mortality after stroke among adults aged 18 to 50 years. JAMA. 2013;309:1136–44.
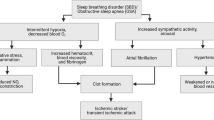
•• Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005;353:2034–41. In this observational cohort study, 1022 patients were enrolled and 697 (68%) were diagnosed as OSA. Strikingly, OSA was associated with an increased risk of stroke and death from any cause.
• Johnson KG, Johnson DC. Frequency of sleep apnea in stroke and TIA patients: a meta-analysis. J Clin Sleep Med. 2010;6:131–7. In this meta-analysis, 2343 ischemic or hemorrhagic stroke and TIA patients were considered. SBD was present in 72% of patients. The authors concluded that since SDB was not detectable through clinical history alone, sleep study is required in stroke and TIA patients.
Mims KN, Kirsch D. Sleep and stroke. Sleep Med Clin. 2016;11:39–51.
Brooks D, Davis L, Vujovic-Zotovic N, Boulias C, Ismail F, Richardson D, et al. Sleep disordered breathing in patients enrolled in an inpatient stroke rehabilitation program. Arch Phys Med Rehabil. 2010;91:659–62.
Das AM, Khan M. Obstructive sleep apnea and stroke. Expert Rev Cardiovasc Ther. 2012;10:525–35.
Franklin KA. Cerebral haemodynamics in obstructive sleep apnoea and Cheyne–Stokes respiration. Sleep Med Rev. 2002;6:429–41.
Fischer AQ, Chaudhary BA, Taormina MA, Akhtar B. Intracranial hemodynamics in sleep apnea. Chest. 1992;102:1402–6.
Balfors EM, Franklin KA. Impairment of cerebral perfusion during obstructive sleep apneas. Am J Respir Crit Care Med. 1994;150:1587–91.
Ip MS, Tse HF, Lam B, Tsang KW, Lam WK. Endothelial function in obstructive sleep apnea and response to treatment. Am J Respir Crit Care Med. 2004;169:348–53.
Wessendorf TE, Thilmann AF, Wang YM, Schreiber A, Konietzko N, Teschler H. Fibrinogen levels and obstructive sleep apnea in ischemic stroke. Am J Respir Crit Care Med. 2000;162:2039–42.
Geiser T, Buck F, Meyer BJ, Bassetti C, Haeberli A, Gugger M. In vivo platelet activation is increased during sleep in patients with obstructive sleep apnea syndrome. Respiration. 2002;69:229–34.
• Hermann DM, Bassetti CL. Role of sleep-disordered breathing and sleep-wake disturbances for stroke and stroke recovery. Neurology. 2016;87:1407–16. In this review, the authors underlined the importance of a systematic employment of clinical procedure for the diagnosis and treatment of SDB in stroke patients.
Mohsenin V. Obstructive sleep apnea: a new preventive and therapeutic target for stroke: a new kid on the block. Am J Med. 2015;128:811–6.
Sandberg O, Franklin KA, Bucht G, Eriksson S, Gustafson Y. Nasal continuous positive airway pressure in stroke patients with sleep apnoea: a randomized treatment study. Eur Respir J. 2001;18:630–4.
Hsu CY, Vennelle M, Li HY, Engleman HM, Dennis MS, Douglas NJ. Sleep-disordered breathing after stroke: a randomised controlled trial of continuous positive airway pressure. J Neurol Neurosurg Psychiatry. 2006;77:1143–9.
Bravata DM, Concato J, Fried T, Ranjbar N, Sadarangani T, McClain V, et al. Auto-titrating continuous positive airway pressure for patients with acute transient ischemic attack: a randomized feasibility trial. Stroke. 2010;41:1464–70.
Svatikova A, Chervin RD, Wing JJ, Sanchez BN, Migda EM, Brown DL. Positional therapy in ischemic stroke patients with obstructive sleep apnea. Sleep Med. 2011;12:262–6.
Ryan CM, Bayley M, Green R, Murray BJ, Bradley TD. Influence of continuous positive airway pressure on outcomes of rehabilitation in stroke patients with obstructive sleep apnea. Stroke. 2011;42:1062–7.
Bravata DM, Concato J, Fried T, Ranjbar N, Sadarangani T, McClain V, et al. Continuous positive airway pressure: evaluation of a novel therapy for patients with acute ischemic stroke. Sleep. 2011;34:1271–7.
Minnerup J, Ritter MA, Wersching H, Kemmling A, Okegwo A, Schmidt A, et al. Continuous positive airway pressure ventilation for acute ischemic stroke: a randomized feasibility study. Stroke. 2012;43:1137–9.
Brown DL, Chervin RD, Kalbfleisch JD, Zupancic MJ, Migda EM, Svatikova A, et al. Sleep Apnea Treatment after Stroke (SATS) trial: is it feasible? J Stroke Cerebrovasc Dis. 2013;22:1216–24.
Parra O, Sánchez-Armengol Á, Capote F, Bonnin M, Arboix A, Campos-Rodríguez F, et al. Efficacy of continuous positive airway pressure treatment on 5-year survival in patients with ischaemic stroke and obstructive sleep apnea: a randomized controlled trial. J Sleep Res. 2015;24:47–53.
•• McEvoy RD, Antic NA, Heeley E, Luo Y, Ou Q, Zhang X, et al. CPAP for prevention of cardiovascular events in obstructive sleep apnea. N Engl J Med. 2016;375:919–31. This study, involving 2717 patients with moderate-to-severe OSA and coronary or cerebrovascular disease, emphasizes how the use of CPAP did not prevent cardiovascular events when compared with traditional care.
Mello-Fujita L, Kim LJ, Palombini Lde O, Rizzi C, Tufik S, Andersen ML, et al. Treatment of obstructive sleep apnea syndrome associated with stroke. Sleep Med. 2015;16:691–6.
Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004;24 Suppl 1:9–160.
Kristiansen HA, Kværner KJ, Akre H, Øverland B, Sandvik L, Russell MB. Sleep apnoea headache in the general population. Cephalalgia. 2012;32:451–8.
Graff-Radford SB, Newman A. Obstructive sleep apnea and cluster headache. Headache. 2004;44:607–10.
Stark CD, Stark RJ. Sleep and chronic daily headache. Curr Pain Headache Rep. 2015;19:468.
Guchlerner M, Kardos P, Liss-Koch E, Franke J, Wunderlich N, Bertog S, et al. PFO and right-to-left shunting in patients with obstructive sleep apnea. J Clin Sleep Med. 2012;8:375–80.
Bigal ME, Lipton RB, Holland PR, Goadsby PJ. Obesity, migraine, and chronic migraine: possible mechanisms of interaction. Neurology. 2007;68:1851–61.
Singh NN, Sahota P. Sleep-related headache and its management. Curr Treat Options Neurol. 2013;15:704–22.
Goksan B, Gunduz A, Karadeniz D, Ağan K, Tascilar FN, Tan F, et al. Morning headache in sleep apnoea: clinical and polysomnographic evaluation and response to nasal continuous positive airway pressure. Cephalalgia. 2009;29:635–41.
• Kallweit U, Hidalgo H, Uhl V, Sándor PS. Continuous positive airway pressure therapy is effective for migraines in sleep apnea syndrome. Neurology. 2011;76:1189–91. This study provided evidence that CPAP given for 1 year significantly decreases the frequency of migraine in OSA patients.
Johnson KG, Ziemba AM, Garb JL. Improvement in headaches with continuous positive airway pressure for obstructive sleep apnea: a retrospective analysis. Headache. 2013;53:333–43.
Marklund M, Carlberg B, Forsgren L, Olsson T, Stenlund H, Franklin KA. Oral appliance therapy in patients with daytime sleepiness and snoring or mild to moderate sleep apnea: a randomized clinical trial. JAMA Intern Med. 2015;175:1278–85.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Giulia Elisabetta Lombardi, Sara Marelli, and Andrea Galbiati declare that they have no conflict of interest.
Luigi Ferini-Strambi reports personal fees from Resmed, Philips Respironics, Mundipharma, Italfarmaco, UCB Pharma, and Valeas.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Sleep Disorders
Rights and permissions
About this article
Cite this article
Ferini-Strambi, L., Lombardi, G.E., Marelli, S. et al. Neurological Deficits in Obstructive Sleep Apnea. Curr Treat Options Neurol 19, 16 (2017). https://doi.org/10.1007/s11940-017-0451-8
Published:
DOI: https://doi.org/10.1007/s11940-017-0451-8