Opinion Statement
The medical community has only recently started to focus attention on the role of food in the pathogenesis of irritable bowel syndrome (IBS), though the association between food and gastrointestinal (GI) symptoms has been recognized by patients for decades. Health care providers receive little formal training in the dietary management of IBS and have traditionally viewed dietary interventions with skepticism. There is mounting evidence that links food to changes in motility, visceral sensation, microbiome, permeability, immune activation, and brain–gut interactions—all key elements in the pathogenesis of IBS. The role of specific dietary modification in the management of IBS has not been rigorously investigated until recently. There is now credible evidence suggesting that targeted dietary carbohydrate exclusion provides clinical benefits to IBS patients. There is emerging evidence to suggest that proteins such as gluten, as well as food chemicals, may play a role in IBS.




Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Lovell RM, Ford AC. Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clin Gastroenterol Hepatol. 2012;10(7):712–721 e4.
Longstreth GF et al. Functional bowel disorders. Gastroenterology. 2006;130(5):1480–91.
Eswaran S, Tack J, Chey WD. Food: the forgotten factor in the irritable bowel syndrome. Gastroenterol Clin N Am. 2011;40(1):141–62.
Morcos A, Dinan T, Quigley EM. Irritable bowel syndrome: role of food in pathogenesis and management. J Dig Dis. 2009;10(4):237–46.
Hayes P et al. A dietary survey of patients with irritable bowel syndrome. J Hum Nutr Diet. 2014;27 Suppl 2:36–47.
Simrén M et al. Food-related gastrointestinal symptoms in the irritable bowel syndrome. Digestion. 2001;63(2):108–15.
Chey WD. The role of food in the functional gastrointestinal disorders: introduction to a manuscript series. Am J Gastroenterol. 2013;108(5):694–7.
Hayes PA, Fraher MH, Quigley EM. Irritable bowel syndrome: the role of food in pathogenesis and management. Gastroenterol Hepatol. 2014;10(3):164–74.
Ragnarsson G, Bodemar G. Pain is temporally related to eating but not to defaecation in the irritable bowel syndrome (IBS). Patients' description of diarrhea, constipation and symptom variation during a prospective 6-week study. European J Gastroenterol Hepatol. 1998;10(5):415–21.
Chey WD et al. Utility of the Rome I and Rome II criteria for irritable bowel syndrome in U.S. women. Am J Gastroenterol. 2002;97(11):2803–11.
Kanazawa M, Fukudo S. Effects of fasting therapy on irritable bowel syndrome. Int J Behav Med. 2006;13(3):214–20.
Monsbakken KW, Vandvik PO, Farup PG. Perceived food intolerance in subjects with irritable bowel syndrome—etiology, prevalence and consequences. Eur J Clin Nutr. 2005;60(5):667–72.
Sicherer SH. Food allergy. Lancet. 2002;360(9334):701–10.
Halpert A et al. What patients know about irritable bowel syndrome (IBS) and what they would like to know. National Survey on Patient Educational Needs in IBS and development and validation of the Patient Educational Needs Questionnaire (PEQ). Am J Gastroenterol. 2007;102(9):1972–82.
Yao CK, Gibson PR, Shepherd SJ. Design of clinical trials evaluating dietary interventions in patients with functional gastrointestinal disorders. Am J Gastroenterol. 2013;108(5):748–58.
Boettcher E, Crowe SE. Dietary proteins and functional gastrointestinal disorders. Am J Gastroenterol. 2013;108(5):728–36.
Green PH, Cellier C. Celiac disease. N Engl J Med. 2007;357(17):1731–43.
Bao F, Green PH, Bhagat G. An update on celiac disease histopathology and the road ahead. Arch Pathol Lab Med. 2012;136(7):735–45.
Biesiekierski JR et al. Characterization of adults with a self-diagnosis of nonceliac gluten sensitivity. Nutr Clin Pract. 2014;29(4):504–9. This study provided evidence that many adults are not being adequately evaluated for celiac disease before starting on a GFD.
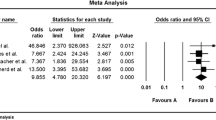
Ford AC et al. Yield of diagnostic tests for celiac disease in individuals with symptoms suggestive of irritable bowel syndrome: systematic review and meta-analysis. Arch Intern Med. 2009;169(7):651–8.
Catassi C et al. Non-celiac gluten sensitivity: the new frontier of gluten related disorders. Nut. 2013;5(10):3839–53.
Verdu EF, Armstrong D, Murray JA. Between celiac disease and irritable bowel syndrome: the "no man's land" of gluten sensitivity. Am J Gastroenterol. 2009;104(6):1587–94.
Vazquez-Roque MI et al. A controlled trial of gluten-free diet in patients with irritable bowel syndrome-diarrhea: effects on bowel frequency and intestinal function. Gastroenterology. 2013;144(5):903–911 e3. This study provided possible mechanisms for NCWS.
Biesiekierski JR et al. Gluten causes gastrointestinal symptoms in subjects without celiac disease: a double-blind randomized placebo-controlled trial. Am J Gastroenterol. 2011;106(3):508–14. quiz 515. This study provided compelling evidence of NCWS in a randomized, double-blind, placebo-controlled rechallenge trial.
Kaukinen K et al. Celiac disease without villous atrophy: revision of criteria called for. Dig Dis Sci. 2001;46(4):879–87.
Johlin Jr FC, Panther M, Kraft N. Dietary fructose intolerance: diet modification can impact self-rated health and symptom control. Nutr Clinical Care. 2004;7(3):92–7.
Biesiekierski JR et al. No effects of gluten in patients with self-reported non-celiac gluten sensitivity after dietary reduction of fermentable, poorly absorbed, short-chain carbohydrates. Gastroenterology. 2013;145(2):320–8 e1–3. The results of this study suggested that the fructan/FODMAP content of wheat was more important to generation of IBS symptoms than gluten, contradicting the conclusions drawn in the same authors’ previous study and lending credence to the notion of “wheat sensitivity” rather than “gluten sensitivity”.
Wahnschaffe U et al. Predictors of clinical response to gluten-free diet in patients diagnosed with diarrhea-predominant irritable bowel syndrome. Clin Gastroenterol Hepatol. 2007;5(7):844–50. quiz 769.
Wahnschaffe U et al. Predictors of clinical response to gluten-free diet in patients diagnosed with diarrhea-predominant irritable bowel syndrome. Clin Gastroenterol Hepatol. 2007;5(7):844–50.
Wahnschaffe U et al. Celiac disease-like abnormalities in a subgroup of patients with irritable bowel syndrome. Gastroenterology. 2001;121(6):1329–38.
Carroccio A et al. Non-celiac wheat sensitivity diagnosed by double-blind placebo-controlled challenge: exploring a new clinical entity. Am J Gastroenterol. 2012;107(12):1898–906. quiz 1907.
Shepherd SJ, Lomer MC, Gibson PR. Short-chain carbohydrates and functional gastrointestinal disorders. Am J Gastroenterol. 2013;108(5):707–17.
Gibson PR et al. Review article: fructose malabsorption and the bigger picture. Aliment Pharmacol Ther. 2007;25(4):349–63.
Brighenti F et al. Comparison of lactulose and inulin as reference standard for the study of resistant starch fermentation using hydrogen breath test. Ital J Gastroenterol. 1995;27(3):122–8.
Tazoe H et al. Roles of short-chain fatty acids receptors, GPR41 and GPR43 on colonic functions. J Physiol Pharmacol. 2008;59 Suppl 2:251–62.
Murray K et al. Differential effects of FODMAPs (fermentable oligo-, di-, mono-saccharides and polyols) on small and large intestinal contents in healthy subjects shown by MRI. Am J Gastroenterol. 2014;109(1):110–9. This study provided evidence for region-specific effects of different types of carbohydrates on luminal distention of the gut.
Symons P, Jones MP, Kellow JE. Symptom provocation in irritable bowel syndrome. Effects of differing doses of fructose-sorbitol. Scand J Gastroenterol. 1992;27(11):940–4.
Nelis GF, Vermeeren MA, Jansen W. Role of fructose-sorbitol malabsorption in the irritable bowel syndrome. Gastroenterology. 1990;99(4):1016–20.
Goldstein R, Braverman D, Stankiewicz H. Carbohydrate malabsorption and the effect of dietary restriction on symptoms of irritable bowel syndrome and functional bowel complaints. Isr Med Assoc J. 2000;2(8):583–7.
Gibson PR, Shepherd SJ. Evidence-based dietary management of functional gastrointestinal symptoms: the FODMAP approach. J Gastroenterol Hepatol. 2010;25(2):252–8.
Austin GL et al. A very low-carbohydrate diet improves symptoms and quality of life in diarrhea-predominant irritable bowel syndrome. Clin Gastroenterol Hepatol. 2009;7(6):706–708 e1.
Brandt LJ et al. An evidence-based position statement on the management of irritable bowel syndrome. Am J Gastroenterol. 2009;104 Suppl 1:S1–S35.
Zhu Y et al. Bloating and distention in irritable bowel syndrome: the role of gas production and visceral sensation after lactose ingestion in a population with lactase deficiency. Am J Gastroenterol. 2013;108(9):1516–25.
Tomba C et al. Is the subjective perception of lactose intolerance influenced by the psychological profile? Aliment Pharmacol Ther. 2012;36(7):660–9.
Yang J et al. Prevalence and presentation of lactose intolerance and effects on dairy product intake in healthy subjects and patients with irritable bowel syndrome. Clin Gastroenterol Hepatol. 2013;11(3):262–268 e1.
Vernia P et al. Lactose malabsorption and irritable bowel syndrome. Effect of a long-term lactose-free diet. Ital J Gastroenterol. 1995;27(3):117–21.
Parker TJ et al. Irritable bowel syndrome: is the search for lactose intolerance justified? Eur J Gastroenterol Hepatol. 2001;13(3):219–25.
Schofl R et al. Effect of a lactose-free diet on irritable bowel syndrome [in German]. Wien Klin Wochenschr. 1993;105(12):342–5.
Bohmer CJ, Tuynman HA. The effect of a lactose-restricted diet in patients with a positive lactose tolerance test, earlier diagnosed as irritable bowel syndrome: a 5-year follow-up study. Eur J Gastroenterol Hepatol. 2001;13(8):941–4.
Rao SS et al. Ability of the normal human small intestine to absorb fructose: evaluation by breath testing. Clin Gastroenterol Hepatol. 2007;5(8):959–63.
Truswell AS, Seach JM, Thorburn AW. Incomplete absorption of pure fructose in healthy subjects and the facilitating effect of glucose. Am J Clin Nutr. 1988;48(6):1424–30.
Jones HF, Butler RN, Brooks DA. Intestinal fructose transport and malabsorption in humans. Am J Physiol Gastrointest Liver Physiol. 2011;300(2):G202–6.
Fernandez-Banares F et al. Sugar malabsorption in functional abdominal bloating: a pilot study on the long-term effect of dietary treatment. Clin Nutr. 2006;25(5):824–31.
Shepherd SJ et al. Dietary triggers of abdominal symptoms in patients with irritable bowel syndrome: randomized placebo-controlled evidence. Clin Gastroenterol Hepatol. 2008;6(7):765–71.
Berg LK et al. Effect of fructose-reduced diet in patients with irritable bowel syndrome, and its correlation to a standard fructose breath test. Scand J Gastroenterol. 2013;48(8):936–43.
Wilder-Smith CH et al. Fructose and lactose intolerance and malabsorption testing: the relationship with symptoms in functional gastrointestinal disorders. Aliment Pharmacol Ther. 2013;37(11):1074–83.
Kyaw MH, Mayberry JF. Fructose malabsorption: true condition or a variance from normality. J Clin Gastroenterol. 2011;45(1):16–21.
Biesiekierski JR. Fructose-induced symptoms beyond malabsorption in FGID. United Eur Gastroenterol J. 2014;2(1):10–3.
Yao CK et al. Dietary sorbitol and mannitol: food content and distinct absorption patterns between healthy individuals and patients with irritable bowel syndrome. J Hum Nutr Diet. 2014;27 Suppl 2:263–75.
Gibson PR, Shepherd SJ. Personal view: food for thought—Western lifestyle and susceptibility to Crohn's disease. The FODMAP hypothesis. Aliment Pharmacol Ther. 2005;21(12):1399–409.
Barrett JS et al. Dietary poorly absorbed, short-chain carbohydrates increase delivery of water and fermentable substrates to the proximal colon. Aliment Pharmacol Ther. 2010;31(8):874–82.
Shepherd SJ, Gibson PR. Fructose malabsorption and symptoms of irritable bowel syndrome: guidelines for effective dietary management. J Am Diet Assoc. 2006;106(10):1631–9.
Staudacher HM et al. Comparison of symptom response following advice for a diet low in fermentable carbohydrates (FODMAPs) versus standard dietary advice in patients with irritable bowel syndrome. J Hum Nutr Diet. 2011;24(5):487–95.
Staudacher HM et al. Fermentable carbohydrate restriction reduces luminal bifidobacteria and gastrointestinal symptoms in patients with irritable bowel syndrome. J Nutr. 2012;142(8):1510–8.
de Roest RH et al. The low FODMAP diet improves gastrointestinal symptoms in patients with irritable bowel syndrome: a prospective study. Int J Clin Pract. 2013;67(9):895–903.
Ong DK et al. Manipulation of dietary short chain carbohydrates alters the pattern of gas production and genesis of symptoms in irritable bowel syndrome. Ital J Gastroenterol Hepatol. 2010;25(8):1366–73.
Halmos EP et al. A diet low in FODMAPs reduces symptoms of irritable bowel syndrome. Gastroenterology. 2014;146(1):67–75 e5. This is the most rigorous study supporting the use of the low-FODMAP diet in IBS patients (a randomized, controlled, single-blind, crossover study, with all meals provided).
Azpiroz F et al. Effect of a low-flatulogenic diet in patients with flatulence and functional digestive symptoms. Neurogastroenterol Motil. 2014;26(6):779–85.
Halmos, E.P., et al., Diets that differ in their FODMAP content alter the colonic luminal microenvironment. Gut, Epub 2014 Jul 12. This study provided evidence that changes in the gut microbiota are seen on the low-FODMAP diet, the long-term implications of which are still unknown.
Feinle-Bisset C, Azpiroz F. Dietary lipids and functional gastrointestinal disorders. Am J Gastroenterol. 2013;108(5):737–47.
Serra J et al. Lipid-induced intestinal gas retention in irritable bowel syndrome. Gastroenterology. 2002;123(3):700–6.
Simren M, Abrahamsson H, Bjornsson ES. An exaggerated sensory component of the gastrocolonic response in patients with irritable bowel syndrome. Gut. 2001;48(1):20–7.
Deiteren A et al. Effect of meal ingestion on ileocolonic and colonic transit in health and irritable bowel syndrome. Dig Dis Sci. 2010;55(2):384–91.
Caldarella MP et al. Visceral sensitivity and symptoms in patients with constipation- or diarrhea-predominant irritable bowel syndrome (IBS): effect of a low-fat intraduodenal infusion. Am J Gastroenterol. 2005;100(2):383–9.
Brennan IM et al. Effects of acute dietary restriction on gut motor, hormone and energy intake responses to duodenal fat in obese men. Int J Obes. 2011;35(3):448–56.
Barbera R, Feinle C, Read NW. Abnormal sensitivity to duodenal lipid infusion in patients with functional dyspepsia. Eur J Gastroenterol Hepatol. 1995;7(11):1051–7.
Wong BS et al. Increased bile acid biosynthesis is associated with irritable bowel syndrome with diarrhea. Clin Gastroenterol Hepatol. 2012;10(9):1009–15 e3.
Raithel M et al. Significance of salicylate intolerance in diseases of the lower gastrointestinal tract. J Physiol Pharmacol. 2005;56 Suppl 5:89–102.
Holton KF et al. The effect of dietary glutamate on fibromyalgia and irritable bowel symptoms. Clin Exp Rheumatol. 2012;30(6 Suppl 74):10–7.
Fuhrer M, Hammer J. Effect of repeated, long term capsaicin ingestion on intestinal chemo- and mechanosensation in healthy volunteers. Neurogastroenterol Motil. 2009;21(5):521–7, e7.
Bohn L et al. Self-reported food-related gastrointestinal symptoms in IBS are common and associated with more severe symptoms and reduced quality of life. Am J Gastroenterol. 2013;108(5):634–41.
Petersen J, Raithel M, Schwelberger HG. Histamine N-methyltransferase and diamine oxidase gene polymorphisms in patients with inflammatory and neoplastic intestinal diseases. Inflamm Res. 2002;51 Suppl 1:S91–2.
Bieganski T et al. Distribution and properties of human intestinal diamine oxidase and its relevance for the histamine catabolism. Biochim Biophys Acta. 1983;756(2):196–203.
Bieganski T. Biochemical, physiological and pathophysiological aspects of intestinal diamine oxidase. Acta Physiol Polonica. 1983;34(1):139–54.
Raithel M et al. The involvement of the histamine degradation pathway by diamine oxidase in manifest gastrointestinal allergies. Inflamm Res. 1999;48 Suppl 1:S75–6.
Rosell-Camps A et al. Histamine intolerance as a cause of chronic digestive complaints in pediatric patients. Rev Esp Enferm Dig. 2013;105(4):201–7.
Schmidt WU et al. Human intestinal diamine oxidase (DAO) activity in Crohn's disease: a new marker for disease assessment? Agents Actions. 1990;30(1–2):267–70.
Raithel M et al. Mucosal histamine content and histamine secretion in Crohn's disease, ulcerative colitis and allergic enteropathy. Int Arch Allergy Immunol. 1995;108(2):127–33.
Wantke F, Gotz M, Jarisch R. The red wine provocation test: intolerance to histamine as a model for food intolerance. Allergy Proc. 1994;15(1):27–32.
Zimatkin SM, Anichtchik OV. Alcohol-histamine interactions. Alcohol Alcohol. 1999;34(2):141–7.
Sattler J et al. Inhibition of intestinal diamine oxidase by detergents: a problem for drug formulations with water insoluble agents applied by the intravenous route? Agents Actions. 1987;20(3–4):270–3.
Sattler J et al. Inhibition of human and canine diamine oxidase by drugs used in an intensive care unit: relevance for clinical side effects? Agents Actions. 1985;16(3–4):91–4.
Schwelberger HG. Histamine intolerance: overestimated or underestimated? Inflamm Res. 2009;58 Suppl 1:51–2.
Bodmer S, Imark C, Kneubuhl M. Biogenic amines in foods: histamine and food processing. Inflamm Res. 1999;48(6):296–300.
Maintz L, Novak N. Histamine and histamine intolerance. Am J Clin Nutr. 2007;85(5):1185–96.
Schwelberger HG et al. Genetic polymorphisms of histamine degrading enzymes: from small-scale screening to high-throughput routine testing. Inflamm Res. 2003;52 Suppl 1:S71–3.
Jansen SC et al. Intolerance to dietary biogenic amines: a review. Ann Allergy , Asthma Immunol. 2003;91(3):233–40. quiz 241–2, 296.
Compliance with Ethics Guidelines
Conflict of Interest
Marisa Spencer and Shanti Eswaran declare that they have no conflict of interest.
William D. Chey has received consultancy fees from Astra-Zeneca, Forest, Ironwood, Perrigo, Prometheus, Nestle, Sucampo, Takeda, Furiex, SK, Ferring, and Entera. He also has received grants from Ironwood, Prometheus, Nestle, and Perrigo.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Spencer, M., Chey, W.D. & Eswaran, S. Dietary Renaissance in IBS: Has Food Replaced Medications as a Primary Treatment Strategy?. Curr Treat Options Gastro 12, 424–440 (2014). https://doi.org/10.1007/s11938-014-0031-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11938-014-0031-x