Abstract
Purpose of review
The management of valvular heart disease has been dramatically influenced by recent evolutions in biomedical technology and surgical practice. With an aging population worldwide and accompanying increase in the prevalence of surgical valve disease, an understanding of prosthetic valve behavior and durability is essential for proper patient selection and management. This report offers an overview of the definitions, mechanisms, management, and clinical impact of structural valve degeneration and failure.
Recent findings
Published literature has employed variable definitions and outcome measures, complicating our understanding of bioprosthetic valve behavior and function. The pathophysiology leading to structural valve degeneration is multifactorial and involves mechanical, hematologic, and immunologic elements. Technological advancements have resulted in improved valve performance and new strategies to mitigate the risks of degeneration.
Summary
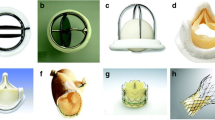
While mechanical valves have demonstrated negligible durability concerns, the benefits of bioprosthetic valves must be weighed against their potential for structural degeneration and subsequent reintervention. Valve selection should involve patient-specific deliberation, and guidelines have been established to help guide risk reduction strategies. Surgical valve replacement remains the standard of care for prosthetic valve failure, but emerging technology offers the potential to slow the development of structural degeneration and transcatheter valve-in-valve options are being increasingly explored.



Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Iung B, Baron G, Butchart EG, Delahaye F, Gohlke-Barwofl C, Levang OW, et al. A prospective survey of patients with valvular heart disease in europe: the euro heart survey on valvular heart disease. Eur Heart J. 2003;24(13):1231–43.
Nkomo VT, Gardin JM, Dkelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M. Burden of valvular heart disease: a population-based study. Lancet. 2006;368(9540):1005–11.
Van Geldorp MW, Heuvelman HJ, Kappetein AP, Busschbach JJ, Takkenberg JJ, Bogers AJ. The effect of aortic valve replacement on quality of life in symptomatic patients with severe aortic stenosis. Neth Hear J. 2013;21(1):28–35.
Isaacs AJ, Shuhaiber J, Salemi A, Isom OW, Sedrakyan A. National trends in utilization and in-hospital outcomes of mechanical versus bioprosthetic aortic valve replacements. J Thorac Cardiovasc Surg. 2015;149(5):1262–9.
Akins CW, Miller DC, Turina MI, Kouchoukos NT, Blakstone EH, Grunkemeier GL, et al. Councils of the American Association for Thoracic Surgery; Society of Thoracic Surgeons; European Association for Cardio-Thoracic Surgery; Ad Hoc Liaison Committee for Standardizing Definitions of Prosthetic Heart Valve Morbidity. Guidelines for reporting mortality and morbidity after cardiac valve interventions. J Thorac Cardiovasc Surg. 2008;135:732–8.
Swanson JS, Starr A. The ball valve experience over three decades. Ann Thorac Surg. 1989;48:S51–2.
Hammermeister K, Sethi GK, Henderson WG, Grover FL, Oprian C, Rahimtoola SH. Outcomes 15 years after valve replacement with a mechanical versus a bioprosthetic valve: final report of the Veterans Affairs randomized trial. J Am Coll Cardiol. 2000;36(4):1152–8.
Toole JM, Stroud MR, Kratz JM, Crumbley AJ, Bradley SM, Crawford FA, et al. Twenty-five year experience with the St. Jude medical mechanical valve prosthesis. Ann Thorac Surg. 2010;89:1402–9.
Harris C, Croce B, Cao C. Tissue and mechanical heart valves. Ann Cardiothorac Surg. 2015;4(4):399.
Edmunds LH, Clark RE, Cohn LH, Grunkemeier GL, Miller DC, Weisel RD. Guidelines for reporting morbidity and mortality after cardiac valvular operations. J Thorac Cardiovasc Surg. 1996;112:708–11.
Zoghbi WA, Chambers JB, Dumesnil JG, Foster E, Gottdiener JS, Grayburn PA, et al. Recommendation for evaluation of prosthetic valves with echocardiography and doppler ultrasound: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Task Force on Prosthetic Valves, developed in conjunction with the American College of Cardiology Cardiovascular Imaging Committee, Cardiac Imaging Committee of the American Heart Association, the European Association of Echocardiography, a registered branch of the European Society of Cardiology, the Japanese Society of Echocardiography and the Canadian Society of Echocardiography, endorsed by the American College of Cardiology Foundation, American Heart Association, European Association of Echocardiography, a registered branch of the European Society of Cardiology, the Japanese Society of Echocardiography, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2009;22:975–1014.
Capodanno D, Petronio AS, Prendergast B, Eltchaninoff H, Vahanian A, Modine T, et al. Standardized definitions of structural deterioration and valve failure in assessing long-term durability of transcatheter and surgical aortic bioprosthetic valves: a consensus statement from the European Association of Percutaneous Cardiovascular Interventions (EAPCI) endorsed by the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur J Cardiothorac Surg. 2017;52:408–17. Recent and thorough European consortium consensus statement on prosthetic valve evaluation.
Dvir D, Bourguignon T, Otto CM, Hahn RT, Rosenhek R, Webb JG, et al. Standardized definition of structural valve degeneration for surgical and transcatheter bioprosthetic aortic valves. Circulation. 2018;137:388–99. International consortium proposal for standardization of definitions for valvular degeneration and recommendations for follow-up protocols in an effort to improve the quality of data analysis and clinical decision-making for patients with bioprosthetic valves.
Forcillo J, Pellerin M, Perrault LP, Cartier R, Bouchard D, Demers P, et al. Carpentier-Edwards pericardial valve in the aortic position: 25-years experience. Ann Thorac Surg. 2013;96:486–93.
Bourguignon T, Bouquiaux-Stablo AL, Canolfi P, Mirza A, Loardi C, May MA, et al. Very long-term outcomes of the Carpentier-Edwards Perimount valve in aortic position. Ann Thorac Surg. 2015;99:831–7.
Senage T, Le Tourneau T, Foucher Y, Pattier S, Cueff C, Michel M, et al. Early structural valve deterioration of mitroflow aortic bioprosthesis: mode, incidence, and impact on outcome in a large cohort of patients. Circulation. 2014;130(23):2012–20.
Saleeb SF, Newburger JW, Geva T, Baird CW, Gauvreau K, Padera RF, et al. Accelerated degeneration of a bovine pericardial bioprosthetic aortic valve in children and young adults. Circulation. 2014;130:51–60.
De Paulis R, D’Aleo S, Bellisario A, Salica A, Weltert LP, Scaffa R, et al. The fate of small-size pericardial heart valve prostheses in an older patient population. J Thorac Cardiovasc Surg. 2017;153:31–9. Single center large volume report of early-onset structural valve degeneration for 19mm and 21mm Mitroflow valves leading to widespread discontinuation of their use.
Gunn JM, Malmberg M, Vahasilta T, Lahti AL, Kuttila KT. Thirty-year results after implantation of the Bjork-Shiley convexo-concave heart valve prosthesis. Ann Thorac Surg. 2014;97:552–6.
Starr A, Grunkemeier GL. Durability of the Starr-Edwards heart valve: early decisions led to successful results. Tex Heart Inst J. 2016;43(1):2–3.
Tillquist MN, Maddox TM. Cardiac crossroads: deciding between mechanical or bioprosthetic heart valve replacement. Patient Prefer Adherence. 2011;5:91–9.
Thubrikar MJ, Deck JD, Aouad J, Nolan SP. Role of mechanical stress in calcification of aortic bioprosthetic valves. J Thorac Cardiovasc Surg. 1983;86:115–25.
Vesely I, Barber JE, Ratliff NB. Tissue damage and calcification may be independent mechanisms of bioprosthetic heart valve failure. J Heart Valve Dis. 2001;10(4):471–7.
Chen W, Schoen FJ, Levy RJ. Mechanism of efficacy of 2-amino oleic acid for inhibition of calcification of glutaraldehyde-penetrated porcine bioprosthetic heart valves. Circulation. 1994;90:323–9.
Schoen FJ, Tsao JW, Levy RJ. Calcification of bovine pericardium used in cardiac valve bioprostheses. Implications for the mechanisms of bioprosthetic tissue mineralization. Am J Pathol. 1986;123:134–45.
Manji RA, Zhu LF, Nijjar NK, Rayner DC, Korbutt GS, Churchill TA, et al. Glutaraldehyde-fixed bioprosthetic heart valve conduits calcify and fail from xenograft rejection. Circulation. 2006;114:318–27.
Rahimtoola SH. Choice of prosthetic heart valve in adults: an update. J Am Coll Cardiol. 2010;55:2413–26.
Rodriguez-Gabella T, Voisine P, Puri R, Pibarot P, Rodes-Cabau J. Aortic bioprosthetic valve durability: incidence, mechanisms, predictors, and management of surgical and transcatheter valve degeneration. J Am Coll Cardiol. 2017;70:1013–28.
Cote N, Pibarot P, Clavel MA. Incidence, risk factors, clinical impact, and management of bioprosthesis structural valve degeneration. Curr Opin Cardiol. 2017;32:123–9. Comprehensive review of the risk factors for bioprosthetic valve degeneration including discussion of immunologic and inflammatory mechanisms.
Le Tourneau T, Marechaux S, Vicentelli A, Ennezat PV, Modine T, Polge AS, et al. Cardiovascular risk factors as predictors of early and late survival after bioprosthetic valve replacement for aortic stenosis. J Heart Valve Dis. 2007;16:483–8.
Pibarot P, Dumesnil JG. Prosthetic heart valves: selection of the optimal prosthesis and long-term management. Circulation. 2009;119:1034–48.
Williams ML, Bavaria JE, Acker MA, Desai ND, Vallabhajosyula P, Hargrove WC, et al. Valve Selection in end-stage renal disease: should it always be biological? Ann Thorac Surg. 2016;1102:1531–5.
McClure RS, Narayanasamy N, Wiegerinck E, Lipsitz S, Maloney A, Byrne JG, et al. Late outcomes for aortic valve replacement with the Carpentier-Edwards pericardial bioprosthesis: up to 17-year follow-up in 1000 patients. Ann Thorac Surg. 2010;89(5):1410–6.
Foroutan F, Guyatt GH, O’Brien K, Bain E, Stein M, Bhagra S, et al. Prognosis after surgical replacement with a bioprosthetic aortic valve in patients with severe symptomatic aortic stenosis: systematic review of observational studies. BMJ. 2016;28:354. Metanalysis review of published outcomes for bioprosthetic aortic valve replacement demonstrating a low incidence of structural degeneration at 10 years with subsequent escalation of adverse events in later follow-up.
Jones JM, O’Kane H, Gladstone DJ, Sarsam MA, Campalani G, MacGowan SW, et al. Repeat heart valve surgery: risk factors for operative mortality. J Thorac Cardiovasc Surg. 2001;122:913–8.
Maganti M, Rao V, Armstrong S, Feindel CM, Scully HE, David TE. Redo Valvular Surgery in Elderly Patients. Ann Throac Surg. 2009;87:521–5.
Leontyev S, Borger MA, Davierwala P, Walther T, Lehmann S, Kempfert J, et al. Redo Aortic Valve Surgery: Early and Late Outcomes. Ann Thorac Surg. 2011;91:1120–6.
Mehaffey HJ, Hawkins RB, Schubert S, Fonner C, Yarboro LT, Quader M, et al. Contemporary outcomes in reoperative mitral valve surgery. Heart. 2018;104:652–6. Recent large volume STS database outcomes review comparing primary mitral valve surgical risk with redo intervention.
Silaschi M, Wendler O, Seiffert M, Castro L, Lubos E, Schirmer J, et al. Transcatheter valve-in-valve implantation versus redo surgical aortic valve replacement in patients with failed aortic bioprostheses. Interact Cardiovasc Thorac Surg. 2017;24:63–70.
Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Fleisher LA, et al. 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College Of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2017;70(2):252–89.
Goldstone AB, Chiu P, Baiocchi M, Lingala B, Patrick WL, Fischbein MP, et al. Mechanical or biologic prostheses for aortic-valve and mitral-valve replacement. N Engl J Med. 2017;377:1847–57. NIH-sponsored retrospective population-based study suggesting a mortality benefit with the use of mechanical valves until age 70 in the mitral position and age 55 for aortic valves.
Fiedler AG, Tolis G. Surgical Treatment of valvular heart disease: overview of mechanical and tissue prostheses, advantages, disadvantages, and implications for clinical use. Curr Treat Options Cardio Med. 2018;20(1):7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Valvular Heart Disease
Rights and permissions
About this article
Cite this article
Baldwin, A.C.W., Tolis, G. Tissue Valve Degeneration and Mechanical Valve Failure. Curr Treat Options Cardio Med 21, 33 (2019). https://doi.org/10.1007/s11936-019-0735-2
Published:
DOI: https://doi.org/10.1007/s11936-019-0735-2