Abstract
Purpose of Review
To review risk factors for AUS complications and present a systematic approach to their diagnosis and management.
Recent Findings
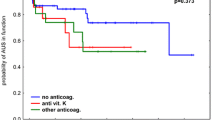
Established risk factors for AUS complications include catheterization, channel TURP, pelvic radiation, urethroplasty, anticoagulation, cardiovascular disease, diabetes mellitus, frailty index, hypertension, low albumin, and low testosterone. We present our algorithm for diagnosis and management of AUS complications.
Summary
Despite being the gold standard of treatment for men with SUI, major and minor complications can occur at any point after AUS insertion. Careful consideration of the urologic, medical, and operative risk factors for each patient can help prevent complications. A systematic approach to early and late complications facilitates their identification and effective management. The evaluating urologist must have a thorough understanding of potential AUS complications in order to restore quality of life in men with bothersome SUI.




Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Tutolo M, Cornu J-N, Bauer RM, Ahyai S, Bozzini G, Heesakkers J, et al. Efficacy and safety of artificial urinary sphincter (AUS): results of a large multi-institutional cohort of patients with mid-term follow-up. Neurourol Urodyn. 2019;38(2):710–8. https://doi.org/10.1002/nau.23901.
Viers BR, Linder BJ, Rivera ME, Rangel LJ, Ziegelmann MJ, Elliott DS. Long-term quality of life and functional outcomes among primary and secondary artificial urinary sphincter implantations in men with stress urinary incontinence. J Urol. 2016;196(3):838–43. https://doi.org/10.1016/j.juro.2016.03.076.
•• Khouri RK, Ortiz NM, Baumgarten AS, et al. Artificial urinary sphincter outperforms sling for moderate male stress urinary incontinence. Urology. 2020. https://doi.org/10.1016/j.urology.2020.03.028Demonstrates the expanded role for AUS in male SUI.
Sacco E, Gandi C, Marino F, Totaro A, di Gianfrancesco L, Palermo G, et al. Artificial urinary sphincter significantly better than fixed sling for moderate postprostatectomy stress urinary incontinence: a propensity score-matched study. BJU Int. 2020;127:229–37. https://doi.org/10.1111/bju.15197.
Kaiho Y, Masuda H, Takei M, Hirayama T, Mitsui T, Yokoyama M, et al. Surgical and patient reported outcomes of artificial urinary sphincter implantation: a multicenter, prospective, observational study. J Urol. 2018;199(1):245–50. https://doi.org/10.1016/j.juro.2017.08.077.
Te Dorsthorst MJ, van der Doelen MJ, Farag F, Martens FMJ, Heesakkers JPFA. Survival of the artificial urinary sphincter in a changing patient profile. World J Urol. 2019;37(5):899–906. https://doi.org/10.1007/s00345-018-2448-7.
Rivera ME, Linder BJ, Ziegelmann MJ, Viers BR, Rangel LJ, Elliott DS. The impact of prior radiation therapy on artificial urinary sphincter device survival. J Urol. 2016;195(4 Pt 1):1033–7. https://doi.org/10.1016/j.juro.2015.10.119.
Averbeck MA, Woodhouse C, Comiter C, Bruschini H, Hanus T, Herschorn S, et al. Surgical treatment of post-prostatectomy stress urinary incontinence in adult men: report from the 6th International Consultation on Incontinence. Neurourol Urodyn. 2019;38(1):398–406. https://doi.org/10.1002/nau.23845.
Linder BJ, Rangel LJ, Elliott DS. Evaluating success rates after artificial urinary sphincter placement: a comparison of clinical definitions. Urology. 2018;113:220–4. https://doi.org/10.1016/j.urology.2017.10.033.
Wingate JT, Erickson BA, Murphy G, Smith TG, Breyer BN, Voelzke BB, et al. Multicenter analysis of patient reported outcomes following artificial urinary sphincter placement for male stress urinary incontinence. J Urol. 2018;199(3):785–90. https://doi.org/10.1016/j.juro.2017.09.089.
• Sandhu JS, Breyer B, Comiter C, et al. Incontinence after prostate treatment: AUA/SUFU Guideline. J Urol. 2019;202(2):369–78. https://doi.org/10.1097/JU.0000000000000314Provides clinical guidelines for male SUI.
Boswell TC, Elliott DS, Rangel LJ, Linder BJ. Long-term device survival and quality of life outcomes following artificial urinary sphincter placement. Transl Androl Urol. 2020;9(1):56–61. https://doi.org/10.21037/tau.2019.08.02.
Radomski SB, Ruzhynsky V, Wallis CJD, Herschorn S. Complications and interventions in patients with an artificial urinary sphincter: long-term results. J Urol. 2018;200(5):1093–8. https://doi.org/10.1016/j.juro.2018.05.143.
DeLay KJ, Haney NM, Chiang J, et al. Comparison of adjuvant radiation therapy before or after artificial urinary sphincter placement: a multi-institutional, retrospective analysis. Urology. 2018;113:160–5. https://doi.org/10.1016/j.urology.2017.11.041.
Linder BJ, Rivera ME, Ziegelmann MJ, Elliott DS. Long-term outcomes following artificial urinary sphincter placement: an analysis of 1082 cases at Mayo Clinic. Urology. 2015;86(3):602–7. https://doi.org/10.1016/j.urology.2015.05.029.
Fuchs JS, Shakir N, McKibben MJ, Scott JM, Morey AF. Prolonged duration of incontinence for men before initial anti-incontinence surgery: an opportunity for improvement. Urology. 2018;119:149–54. https://doi.org/10.1016/j.urology.2018.05.006.
Nelson M, Dornbier R, Kirshenbaum E, Eguia E, Sweigert P, Baker M, et al. Use of surgery for post-prostatectomy incontinence. J Urol. 2020;203(4):786–91. https://doi.org/10.1097/JU.0000000000000618.
Seideman CA, Zhao LC, Hudak SJ, Mierzwiak J, Adibi M, Morey AF. Is prolonged catheterization a risk factor for artificial urinary sphincter cuff erosion? Urology. 2013;82(4):943–6. https://doi.org/10.1016/j.urology.2013.06.044.
Khene Z-E, Paret F, Perrouin-Verbe M-A, Prudhomme T, Hascoet J, Nedelec M, et al. Artificial urinary sphincter in male patients with Spina bifida: comparison of perioperative and functional outcomes between bulbar urethra and bladder neck cuff placement. J Urol. 2018;199(3):791–7. https://doi.org/10.1016/j.juro.2017.09.140.
Cohen AJ, Boysen W, Kuchta K, Faris S, Milose J. Artificial urinary sphincter longevity following transurethral resection of the prostate in the setting of prostate cancer. World J Urol. 2019;37(12):2755–61. https://doi.org/10.1007/s00345-019-02684-z.
Mock S, Dmochowski RR, Brown ET, Reynolds WS, Kaufman MR, Milam DF. The impact of urethral risk factors on transcorporeal artificial urinary sphincter erosion rates and device survival. J Urol. 2015;194(6):1692–6. https://doi.org/10.1016/j.juro.2015.06.088.
McGeady JB, McAninch JW, Truesdale MD, Blaschko SD, Kenfield S, Breyer BN. Artificial urinary sphincter placement in compromised urethras and survival: a comparison of virgin, radiated and reoperative cases. J Urol. 2014;192(6):1756–61. https://doi.org/10.1016/j.juro.2014.06.088.
Fuller TW, Ballon-Landa EE, Gallo K, et al. Outcomes and risk factors of revision and replacement artificial urinary sphincter implantation in radiated and non-radiated patients. J Urol. 2020. https://doi.org/10.1097/JU.0000000000000749.
Srivastava A, Joice GA, Patel HD, Manka MG, Sopko NA, Wright EJ. Impact of adjuvant radiation on artificial urinary sphincter durability in postprostatectomy patients. Urology. 2018;114:212–7. https://doi.org/10.1016/j.urology.2017.12.029.
Moser DC, Kaufman MR, Milam DF, Johnsen NV, Cleves MA, Broghammer JA, et al. Impact of radiation and transcorporeal artificial sphincter placement in patients with prior urethral cuff erosion: results from a retrospective multicenter analysis. J Urol. 2018;200(6):1338–43. https://doi.org/10.1016/j.juro.2018.06.069.
Kaufman MR, Milam DF, Johnsen NV, Cleves MA, Broghammer JA, Brant WO, et al. Prior radiation therapy decreases time to idiopathic erosion of artificial urinary sphincter: a multi-institutional analysis. J Urol. 2018;199(4):1037–41. https://doi.org/10.1016/j.juro.2017.11.046.
Hüsch T, Kretschmer A, Thomsen F, Kronlachner D, Kurosch M, Obaje A, et al. Risk factors for failure of male slings and artificial urinary sphincters: results from a large middle european cohort study. Urol Int. 2017;99(1):14–21. https://doi.org/10.1159/000449232.
Kretschmer A, Buchner A, Grabbert M, Stief CG, Pavlicek M, Bauer RM. Risk factors for artificial urinary sphincter failure. World J Urol. 2016;34(4):595–602. https://doi.org/10.1007/s00345-015-1662-9.
Raj GV, Peterson AC, Webster GD. Outcomes following erosions of the artificial urinary sphincter. J Urol. 2006;175(6):2186–90; discussion 2190. https://doi.org/10.1016/S0022-5347(06)00307-7.
Brant WO, Erickson BA, Elliott SP, Powell C, Alsikafi N, McClung C, et al. Risk factors for erosion of artificial urinary sphincters: a multicenter prospective study. Urology. 2014;84(4):934–8. https://doi.org/10.1016/j.urology.2014.05.043.
Godwin CA, Linder BJ, Rivera ME, Ziegelmann MJ, Elliott DS. Effects of smoking status on device survival among individuals undergoing artificial urinary sphincter placement. Am J Mens Health. 2018;12(5):1398–402. https://doi.org/10.1177/1557988316651133.
Medendorp AR, Anger JT, Jin C, Amin KA, Hampson LA, Lee UJ, et al. The Impact of Frailty on Artificial Urinary Sphincter Placement and Removal Procedures. Urology. 2019;129:210–6. https://doi.org/10.1016/j.urology.2019.04.015.
Ginsburg KB, Schwabe JR, Cochrane JA, Tapper A, Burks F, Rambhatla A. Low serum albumin correlates with adverse events following surgery for male urinary incontinence: Analysis of the American College of Surgeons National Surgical Quality Improvement Project. Urology. 2020;137:178–82. https://doi.org/10.1016/j.urology.2019.12.004.
McKibben MJ, Fuentes J, Shakir N, et al. Low Serum Testosterone is Present in Nearly Half of Men Undergoing Artificial Urinary Sphincter Placement. Urology. 2018;118:208–12. https://doi.org/10.1016/j.urology.2018.04.018.
Hofer MD, Morey AF, Sheth K, Tausch TJ, Siegel J, Cordon BH, et al. Low serum testosterone level predisposes to artificial urinary sphincter cuff erosion. Urology. 2016;97:245–9. https://doi.org/10.1016/j.urology.2016.04.065.
Hughes M, Caza T, Li G, Daugherty M, Blakley S, Nikolavsky D. Histologic characterization of the post-radiation urethral stenosis in men treated for prostate cancer. World J Urol. 2019;38:2269–77. https://doi.org/10.1007/s00345-019-03031-y.
Tibbs MK. Wound healing following radiation therapy: a review. Radiother Oncol. 1997;42(2):99–106. https://doi.org/10.1016/s0167-8140(96)01880-4.
Maurer V, Marks P, Dahlem R, Rosenbaum C, Meyer CP, Riechardt S, et al. Prospective analysis of artificial urinary sphincter AMS 800 implantation after buccal mucosa graft urethroplasty. World J Urol. 2019;37(4):647–53. https://doi.org/10.1007/s00345-019-02631-y.
Lai HH, Boone TB. Complex artificial urinary sphincter revision and reimplantation cases--how do they fare compared to virgin cases? J Urol. 2012;187(3):951–5. https://doi.org/10.1016/j.juro.2011.10.153.
Rosenbaum CM, Pham T, Dahlem R, Maurer V, Marks P, Vetterlein MW, et al. The impact of surgical sequence on outcome rates of artificial urinary sphincter implantation: comparative effectiveness of primary, secondary and repeat implantation. World J Urol. 2019;38:2289–94. https://doi.org/10.1007/s00345-019-03029-6.
Zhang F, Liao L. Artificial urinary sphincter implantation: an important component of complex surgery for urinary tract reconstruction in patients with refractory urinary incontinence. BMC Urol. 2018;18(1):3. https://doi.org/10.1186/s12894-018-0314-y.
Selph JP, Madden-Fuentes R, Peterson AC, Webster GD, Lentz AC. Long-term artificial urinary sphincter outcomes following a prior rectourethral fistula repair. Urology. 2015;86(3):608–12. https://doi.org/10.1016/j.urology.2015.06.012.
Heiner SM, Viers BR, Rivera ME, Linder BJ, Elliott DS. What is the fate of artificial urinary sphincters among men undergoing repetitive bladder cancer treatment? Investig Clin Urol. 2018;59(1):44–8. https://doi.org/10.4111/icu.2018.59.1.44.
Hofer MD, Kapur P, Cordon BH, Hamoun F, Russell D, Scott JM, et al. Low testosterone levels result in decreased periurethral vascularity via an androgen receptor-mediated process: pilot study in urethral stricture tissue. Urology. 2017;105:175–80. https://doi.org/10.1016/j.urology.2017.02.037.
Lavi A, Boone TB, Cohen M, Gross M. The patient beyond the sphincter-cognitive and functional considerations affecting the natural history of artificial urinary sphincters. Urology. 2020;137:14–8. https://doi.org/10.1016/j.urology.2019.11.031.
Kim M, Choi D, Hong JH, Kim C-S, Ahn H, Choo M-S. Factors contributing to treatment outcomes of post-prostatectomy incontinence surgery for the selection of the proper surgical procedure for individual patients: a single-center experience. Neurourol Urodyn. 2018;37(6):1978–87. https://doi.org/10.1002/nau.23543.
Ziegelmann MJ, Linder BJ, Avant RA, Elliott DS. Bacterial cultures at the time of artificial urinary sphincter revision surgery in clinically uninfected devices: a contemporary series. J Urol. 2019;201(6):1152–7. https://doi.org/10.1097/JU.0000000000000102.
Darouiche RO, Wall MJ, Itani KMF, et al. Chlorhexidine-alcohol versus povidone-iodine for surgical-site antisepsis. N Engl J Med. 2010;362(1):18–26. https://doi.org/10.1056/NEJMoa0810988.
Yeung LL, Grewal S, Bullock A, Lai HH, Brandes SB. A comparison of chlorhexidine-alcohol versus povidone-iodine for eliminating skin flora before genitourinary prosthetic surgery: a randomized controlled trial. J Urol. 2013;189(1):136–40. https://doi.org/10.1016/j.juro.2012.08.086.
Lightner DJ, Wymer K, Sanchez J, Kavoussi L. Best practice statement on urologic procedures and antimicrobial prophylaxis. J Urol. 2020;203(2):351–6. https://doi.org/10.1097/JU.0000000000000509.
Kavoussi NL, Siegel JA, Viers BR, Pagliara TJ, Hofer MD, Cordon BH, et al. Preoperative urine culture results correlate poorly with bacteriology of urologic prosthetic device infections. J Sex Med. 2017;14(1):163–8. https://doi.org/10.1016/j.jsxm.2016.10.017.
Kavoussi NL, Viers BR, Pagilara TJ, Siegel JA, Hofer MD, Cordon B, et al. Are urine cultures necessary prior to urologic prosthetic surgery? Sex Med Rev. 2018;6(1):157–61. https://doi.org/10.1016/j.sxmr.2017.03.007.
Adamsky MA, Boysen WR, Cohen AJ, Ham S, Dmochowski RR, Faris SF, et al. Evaluating the role of postoperative oral antibiotic administration in artificial urinary sphincter and inflatable penile prosthesis explantation: a nationwide analysis. Urology. 2018;111:92–8. https://doi.org/10.1016/j.urology.2017.07.064.
Dropkin BM, Chisholm LP, Dallmer JD, Johnsen NV, Dmochowski RR, Milam DF, et al. Penile prosthesis insertion in the era of antibiotic stewardship-are postoperative antibiotics necessary? J Urol. 2020;203(3):611–4. https://doi.org/10.1097/JU.0000000000000578.
de Cógáin MR, Elliott DS. The impact of an antibiotic coating on the artificial urinary sphincter infection rate. J Urol. 2013;190(1):113–7. https://doi.org/10.1016/j.juro.2013.01.015.
Hüsch T, Kretschmer A, Thomsen F, Kronlachner D, Kurosch M, Obaje A, et al. Antibiotic coating of the artificial urinary sphincter (AMS 800): is it worthwhile? Urology. 2017;103:179–84. https://doi.org/10.1016/j.urology.2016.12.056.
Simhan J, Morey AF, Zhao LC, Tausch TJ, Scott JF, Hudak SJ, et al. Decreasing need for artificial urinary sphincter revision surgery by precise cuff sizing in men with spongiosal atrophy. J Urol. 2014;192(3):798–803. https://doi.org/10.1016/j.juro.2014.03.115.
Bergeson RL, Yi YA, Baker RC, Ward EE, Davenport MT, Morey AF. Urethral atrophy is now a rare cause for artificial urinary sphincter revision surgery in the contemporary 3.5 cm cuff era. Transl Androl Urol. 2020;9(1):50–5. https://doi.org/10.21037/tau.2019.07.18.
Loh-Doyle JC, Hartman N, Nazemi A, Wayne K, Doumanian LR, Ginsberg DA, et al. Mechanical failure rates of artificial urinary sphincter components: is the 3.5-cm urethral cuff at higher risk? Neurourol Urodyn. 2019;38(1):187–92. https://doi.org/10.1002/nau.23825.
Simhan J, Morey AF, Singla N, Tausch TJ, Scott JF, Lemack GE, et al. 3.5 cm artificial urinary sphincter cuff erosion occurs predominantly in irradiated patients. J Urol. 2015;193(2):593–7. https://doi.org/10.1016/j.juro.2014.07.115.
McKibben MJ, Shakir N, Fuchs JS, Scott JM, Morey AF. Erosion rates of 3.5-cm artificial urinary sphincter cuffs are similar to larger cuffs. BJU Int. 2018. https://doi.org/10.1111/bju.14483.
Patel N, Golan R, Halpern JA, Sun T, Asafu-Adjei AD, Chughtai B, et al. A contemporary analysis of dual inflatable penile prosthesis and artificial urinary sphincter outcomes. J Urol. 2019;201(1):141–6. https://doi.org/10.1016/j.juro.2018.07.046.
Boysen WR, Cohen AJ, Kuchta K, Park S, Milose J. Combined placement of artificial urinary sphincter and inflatable penile prosthesis does not increase risk of perioperative complications or impact long-term device survival. Urology. 2019;124:264–70. https://doi.org/10.1016/j.urology.2018.10.033.
Ajay D, Mendez MH, Wang R, Westney OL. Treatment of urinary incontinence in patients with erectile dysfunction. Sex Med Rev. 2020. https://doi.org/10.1016/j.sxmr.2020.04.006.
Kavoussi NL, Hofer MD, Viers BR, Cordon BH, Mooney RP, Pagliara TJ, et al. Synchronous ipsilateral high submuscular placement of prosthetic balloons and reservoirs. J Sex Med. 2017;14(2):264–8. https://doi.org/10.1016/j.jsxm.2016.12.001.
Loh-Doyle JC, Ashrafi A, Nazemi A, Ghodoussipour S, Thompson E, Wayne K, et al. Dual prosthetic implantation after radical cystoprostatectomy and neobladder: outcomes of the inflatable penile prosthesis and artificial urinary sphincter in bladder cancer survivors. Urology. 2019;127:127–32. https://doi.org/10.1016/j.urology.2019.01.010.
Sundaram V, Cordon BH, Hofer MD, Morey AF. Is risk of artificial urethral sphincter cuff erosion higher in patients with penile prosthesis? J Sex Med. 2016;13(9):1432–7. https://doi.org/10.1016/j.jsxm.2016.06.013.
Linder BJ, Piotrowski JT, Ziegelmann MJ, Rivera ME, Rangel LJ, Elliott DS. Perioperative complications following artificial urinary sphincter placement. J Urol. 2015;194(3):716–20. https://doi.org/10.1016/j.juro.2015.02.2945.
Chouhan JD, Terlecki RP. A user’s guide for surgery involving the artificial urinary sphincter. Sex Med Rev. 2019;7(1):167–77. https://doi.org/10.1016/j.sxmr.2018.10.004.
Rozanski AT, Tausch TJ, Ramirez D, Simhan J, Scott JF, Morey AF. Immediate urethral repair during explantation prevents stricture formation after artificial urinary sphincter cuff erosion. J Urol. 2014;192(2):442–6. https://doi.org/10.1016/j.juro.2014.02.007.
Chertack N, Chaparala H, Angermeier KW, Montague DK, Wood HM. Foley or fix: a comparative analysis of reparative procedures at the time of explantation of artificial urinary sphincter for cuff erosion. Urology. 2016;90:173–8. https://doi.org/10.1016/j.urology.2015.11.040.
Gross MS, Broghammer JA, Kaufman MR, Milam DF, Brant WO, Cleves MA, et al. Urethral stricture outcomes after artificial urinary sphincter cuff erosion: results from a multicenter retrospective analysis. Urology. 2017;104:198–203. https://doi.org/10.1016/j.urology.2017.01.020.
Keihani S, Chandrapal JC, Peterson AC, Broghammer JA, Chertack N, Elliott SP, et al. Outcomes of urethroplasty to treat urethral strictures arising from artificial urinary sphincter erosions and rates of subsequent device replacement. Urology. 2017;107:239–45. https://doi.org/10.1016/j.urology.2017.05.049.
Henry GD, Graham SM, Cornell RJ, Cleves MA, Simmons CJ, Vakalopoulos I, et al. A multicenter study on the perineal versus penoscrotal approach for implantation of an artificial urinary sphincter: cuff size and control of male stress urinary incontinence. J Urol. 2009;182(5):2404–9. https://doi.org/10.1016/j.juro.2009.07.068.
Anusionwu I, Miles-Thomas J, Hernandez DJ, Wright EJ. Anatomical and manometric comparison of perineal and transscrotal approaches to artificial urinary sphincter placement. J Urol. 2012;188(5):1834–6. https://doi.org/10.1016/j.juro.2012.07.032.
Schlomer BJ, Dugi DD, Valadez C, Morey AF. Correlation of penile and bulbospongiosus measurements: implications for artificial urinary sphincter cuff placement. J Urol. 2010;183(4):1474–8. https://doi.org/10.1016/j.juro.2009.12.032.
Cordon BH, Singla N, Singla AK. Artificial urinary sphincters for male stress urinary incontinence: current perspectives. Med Devices (Auckl). 2016;9:175–83. https://doi.org/10.2147/MDER.S93637.
Saffarian A, Walsh K, Walsh IK, Stone AR. Urethral atrophy after artificial urinary sphincter placement: is cuff downsizing effective? J Urol. 2003;169(2):567–9. https://doi.org/10.1097/01.ju.0000046665.89269.f7.
Shakir NA, Fuchs JS, McKibben MJ, et al. Refined nomogram incorporating standing cough test improves prediction of male transobturator sling success. Neurourol Urodyn. 2018;37(8):2632–7. https://doi.org/10.1002/nau.23703.
Ficarra V, Novara G, Rosen RC, Artibani W, Carroll PR, Costello A, et al. Systematic review and meta-analysis of studies reporting urinary continence recovery after robot-assisted radical prostatectomy. Eur Urol. 2012;62(3):405–17. https://doi.org/10.1016/j.eururo.2012.05.045.
Hoffman D, Vijay V, Peng M, Sussman RD, Rosenblum N, Brucker BM, et al. Effect of Radiation on Male Stress Urinary Incontinence and the Role of Urodynamic Assessment. Urology. 2019;125:58–63. https://doi.org/10.1016/j.urology.2018.11.031.
Ko KJ, Lee CU, Kim TH, Suh YS, Lee K-S. Predictive factors of de novo overactive bladder after artificial urinary sphincter implantation in men with postprostatectomy incontinence. Urology. 2018;113:215–9. https://doi.org/10.1016/j.urology.2017.09.027.
Jahromi MS, Engle K, Furlong D, Guevara Méndez A, Gomez CS. Overactive bladder and urgency urinary incontinence in men undergoing artificial urinary sphincter placement. Neurourol Urodyn. April 2020;39:1489–93. https://doi.org/10.1002/nau.24378.
Lightner DJ, Gomelsky A, Souter L, Vasavada SP. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU Guideline Amendment 2019. J Urol. 2019;202(3):558–63. https://doi.org/10.1097/JU.0000000000000309.
Rahnama’i MS, Marcelissen TAT, Brierley B, Schurch B, de Vries P. Long-term compliance and results of intravesical botulinum toxin A injections in male patients. Neurourol Urodyn. 2017;36(7):1855–9. https://doi.org/10.1002/nau.23196.
Brucker BM, Demirtas A, Fong E, Kelly C, Nitti VW. Artificial urinary sphincter revision: the role of ultrasound. Urology. 2013;82(6):1424–8. https://doi.org/10.1016/j.urology.2013.07.064.
Selph JP, Belsante MJ, Gupta S, Ajay D, Lentz A, Webster G, et al. The ohmmeter identifies the site of fluid leakage during artificial urinary sphincter revision surgery. J Urol. 2015;194(4):1043–8. https://doi.org/10.1016/j.juro.2015.05.075.
Chung E, Cartmill R. Diagnostic challenges in the evaluation of persistent or recurrent urinary incontinence after artificial urinary sphincter (AUS) implantation in patients after prostatectomy. BJU Int. 2013;112(Suppl):32–5. https://doi.org/10.1111/bju.12207.
Yang DY, Linder BJ, Miller AR, Rangel LJ, Elliott DS. Can time to failure predict the faulty component in artificial urinary sphincter device malfunctions? Int J Urol. 2018;25(2):146–50. https://doi.org/10.1111/iju.13485.
Linder BJ, Viers BR, Ziegelmann MJ, Rivera ME, Rangel LJ, Elliott DS. Artificial urinary sphincter mechanical failures-is it better to replace the entire device or just the malfunctioning component? J Urol. 2016;195(5):1523–8. https://doi.org/10.1016/j.juro.2015.10.084.
Rozanski AT, Viers BR, Shakir NA, Pagliara TJ, Scott JM, Morey AF. Is removal of the pressure-regulating balloon necessary after artificial urinary sphincter cuff erosion? Urology. 2018;113:225–9. https://doi.org/10.1016/j.urology.2017.11.003.
Wiedemann L, Cornu J-N, Haab E, Peyrat L, Beley S, Cathelineau X, et al. Transcorporal artificial urinary sphincter implantation as a salvage surgical procedure for challenging cases of male stress urinary incontinence: surgical technique and functional outcomes in a contemporary series. BJU Int. 2013;112(8):1163–8. https://doi.org/10.1111/bju.12386.
Davenport MT, Akhtar AM, Shakir NA, et al. Comparison of 3.5 cm and transcorporal cuffs in high-risk artificial urinary sphincter populations. Transl Androl Urol. 2020;9(1):62–6. https://doi.org/10.21037/tau.2019.09.33.
•• Ortiz NM, Wolfe AR, Baumgarten AS, et al. Artificial urinary sphincter cuff erosion “Heat Map” shows similar anatomic characteristics for transcorporal and standard approach. J Urol. 2020. https://doi.org/10.1097/JU.0000000000001148Demonstrates the lack of evidence to support transcorporal AUS placement.
Maurer V, Dahlem R, Rosenbaum CM, Gild P, Vetterlein MW, Schüttfort V, et al. Distal double cuff vs transcorporal cuff as salvage options-a prospective analysis of different artificial urinary sphincter (AMS 800) Implantation Sites. Urology. 2019;133:234–9. https://doi.org/10.1016/j.urology.2019.07.018.
Maurer V, Marks P, Dahlem R, Rosenbaum CM, Meyer CP, Riechardt S, et al. Functional outcomes of artificial urinary sphincter implantation with distal bulbar double cuff in men with and without a history of external beam radiotherapy: an analysis of a prospective database. BJU Int. 2019;124(6):1040–6. https://doi.org/10.1111/bju.14882.
Yafi FA, DeLay KJ, Stewart C, Chiang J, Sangkum P, Hellstrom WJG. Device survival after primary implantation of an artificial urinary sphincter for male stress urinary incontinence. J Urol. 2017;197(3 Pt 1):759–65. https://doi.org/10.1016/j.juro.2016.08.107.
Ahyai SA, Ludwig TA, Dahlem R, Soave A, Rosenbaum C, Chun FKH, et al. Outcomes of single- vs double-cuff artificial urinary sphincter insertion in low- and high-risk profile male patients with severe stress urinary incontinence. BJU Int. 2016;118(4):625–32. https://doi.org/10.1111/bju.13449.
Manka MG, Wright EJ. Does use of a second cuff improve artificial urinary sphincter effectiveness? Evaluation using a comparative cadaver model. J Urol. 2015;194(6):1688–91. https://doi.org/10.1016/j.juro.2015.06.102.
Smith PJ, Hudak SJ, Scott JF, Zhao LC, Morey AF. Transcorporal artificial urinary sphincter cuff placement is associated with a higher risk of postoperative urinary retention. Can J Urol. 2013;20(3):6773–7 http://www.ncbi.nlm.nih.gov/pubmed/23783046. Accessed 20 Mar 2021.
Pearlman AM, Rasper AM, Terlecki RP. Proof of concept: exposing the myth of urethral atrophy after artificial urinary sphincter via assessment of circumferential recovery after capsulotomy and intraoperative pressure profiling of the pressure regulating balloon. Investig Clin Urol. 2018;59(4):275–9. https://doi.org/10.4111/icu.2018.59.4.275.
Bugeja S, Ivaz SL, Frost A, Andrich DE, Mundy AR. Urethral atrophy after implantation of an artificial urinary sphincter: fact or fiction? BJU Int. 2016;117(4):669–76. https://doi.org/10.1111/bju.13324.
Moses RA, Keihani S, Craig JR, Basilius J, Hotaling JM, Lenherr SM, et al. Efficacy of pressure regulating balloon exchange in men with post artificial urinary sphincter persistent or recurrent stress urinary incontinence. Urology. 2019;123:252–7. https://doi.org/10.1016/j.urology.2018.07.052.
Srivastava A, Joice GA, Patel HD, Manka MG, Sopko NA, Wright EJ. Causes of artificial urinary sphincter failure and strategies for surgical revision: implications of device component survival. Eur Urol Focus. 2019;5(5):887–93. https://doi.org/10.1016/j.euf.2018.02.014.
Loh-Doyle JC, Nazemi A, Ashrafi A, Doumanian LR, Ginsberg DA, Boyd SD. Predictors of device-related complications after exchange of the pressure-regulating balloon in men with an artificial urinary sphincter. Urology. 2020;135:154–8. https://doi.org/10.1016/j.urology.2019.09.026.
Yarlagadda VK, Kilgore ML, Selph JP. Analysis of cost of component replacement versus entire device replacement during artificial urinary sphincter revision surgery. Neurourol Urodyn. 2018;37(6):1931–6. https://doi.org/10.1002/nau.23533.
•• Khouri RK, Baumgarten AS, Ortiz NM, et al. Pressure regulating balloon herniation: a correctable cause of artificial urinary sphincter malfunction. Urology. 2020. https://doi.org/10.1016/j.urology.2020.01.036Newly identifies a correctible cause of AUS malfunction.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors were performed in accordance with all applicable ethical standards including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines.
Conflict of Interest
Dr. Allen Morey receives honoraria for being a guest lecturer/meeting participant for Boston Scientific and Coloplast Corp.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Men's Health
Rights and permissions
About this article
Cite this article
Khouri, R.K., Ortiz, N.M., Dropkin, B.M. et al. Artificial Urinary Sphincter Complications: Risk Factors, Workup, and Clinical Approach. Curr Urol Rep 22, 30 (2021). https://doi.org/10.1007/s11934-021-01045-x
Accepted:
Published:
DOI: https://doi.org/10.1007/s11934-021-01045-x