Abstract
Purpose of Review
Kidney transplantation is the best treatment for end-stage renal disease. However, due to organ shortage, suboptimal grafts are increasingly being used.
Recent Findings
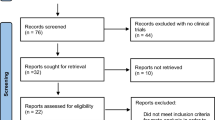
We carried out a review on the methods and techniques of organ optimization in the cadaveric setting.
Summary
Donor care is the first link in a chain of care. Right after brain death, there is a set of changes, of which hormonal and hemodynamic changes are the most relevant. Several studies have been conducted to determine which drugs to administer, although in most cases, the results are not definitive. The main goal seems rather achieve a set of biochemical and hemodynamic objectives. The ischemia–reperfusion injury is a critical factor for kidney damage in transplantation. One of the ways found to deal with this type of injury is preconditioning. Local and remote ischemic preconditioning has been studied for various organs, but studies on the kidney are scarce. A new promising area is pharmacological preconditioning, which is taking its first steps. Main surgical techniques were established in the late twentieth century. Some minor new features have been introduced to deal with anatomical variations or the emergence of donation after circulatory death. Finally, after harvesting, it is necessary to ensure the best conditions for the kidneys until the time of transplantation. Much has evolved since static cold preservation, but the best preservation conditions are yet to be determined. Conservation in the cold has come to be questioned, and great results have appeared at temperatures closer to physiological.
Similar content being viewed by others
References
Wolfe RA, Ashby VB, Milford EL, Ojo AO, Ettenger RE, Agodoa LY, et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med. 1999;341:1725–30.
NHS Blood and Transplant. Annual Report on Kidney Transplantation 2017/18, https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/12256/nhsbt-kidney-transplantation-annual-report-2017-2018.pdf (2018).
Summers DM, Watson CJE, Pettigrew GJ, Johnson RJ, Collett D, Neuberger JM, et al. Kidney donation after circulatory death (DCD): state of the art. Kidney Int. 2015;88:241–9.
Wood KE, Becker BN, McCartney JG, et al. Care of the potential organ donor. N Engl J Med. 2004;351:2730–9.
Anderson TA, Bekker P, Vagefi PA. Anesthetic considerations in organ procurement surgery: a narrative review. Can J Anesth Can d’anesthésie. 2015;62:529–39.
van Der Hoeven JAB, Molema G, Ter Horst GJ, et al. Relationship between duration of brain death and hemodynamic (in)stability on progressive dysfunction and increased immunologic activation of donor kidneys. Kidney Int. 2003;64:1874–82.
Malinoski DJ, Patel MS, Ahmed O, Daly MC, Mooney S, Graybill CO, et al. The impact of meeting donor management goals on the development of delayed graft function in kidney transplant recipients. Am J Transplant. 2013;13:993–1000.
Gottmann U, Brinkkoetter PT, Bechtler M, Hoeger S, Karle C, Schaub M, et al. Effect of pre-treatment with catecholamines on cold preservation and ischemia/reperfusion-injury in rats. Kidney Int. 2006;70:321–8.
Schaub M, Ploetz CJ, Gerbaulet D, Fang L, Kranich P, Stadlbauer TH, et al. Effect of dopamine on inflammatory status in kidneys of brain-dead rats. Transplantation. 2004;77:1333–40.
Liu Z, Hoeger S, Schnuelle P, Feng Y, Goettmann U, Waldherr R, et al. Donor dopamine pretreatment inhibits tubulitis in renal allografts subjected to prolonged cold preservation. Transplantation. 2007;83:297–303.
Schnuelle P, Lorenz D, Mueller A, et al. Donor catecholamine use reduces acute allograft rejection and improves graft survival after cadaveric renal transplantation1. Kidney Int. 1999;56:738–46. 1 by Lu, p. 756.
Schnuelle P, Berger S, de Boer J, et al. Effects of catecholamine application to brain-dead donors on graft survival in solid organ transplantation. Transplantation. 2001;72:455–63.
Schnuelle P, Schmitt WH, Weiss C, Habicht A, Renders L, Zeier M, et al. Effects of dopamine donor pretreatment on graft survival after kidney transplantation: a randomized trial. Clin J Am Soc Nephrol. 2017;12:493–501.
Schnuelle P, Mundt HM, Drüschler F, Schmitt WH, Yard BA, Krämer BK, et al. Impact of spontaneous donor hypothermia on graft outcomes after kidney transplantation. Am J Transplant. 2018;18:704–14.
Salim A, Velmahos GC, Brown C, Belzberg H, Demetriades D. Aggressive organ donor management significantly increases the number of organs available for transplantation. J Trauma. 2005;58:991–4.
Al-Khafaji A, Elder M, Lebovitz DJ, et al. Protocolized fluid therapy in brain-dead donors: the multicenter randomized MOnIToR trial. Intensive Care Med. 2015;41:418–26.
Limnell N, Schramko AA. Is brain-dead donor fluid therapy with colloids associated with better kidney grafts? Exp Clin Transplant. 2018;16:55–60.
Cittanova ML, Leblanc I, Legendre C, Mouquet C, Riou B, Coriat P. Effect of hydroxyethylstarch in brain-dead kidney donors on renal function in kidney-transplant recipients. Lancet. 1996;348:1620–2.
Blasco V, Colavolpe JC, Antonini F, et al. Long-term outcome in kidney recipients from donors treated with hydroxyethylstarch 130/0.4 and hydroxyethylstarch 200/0.6. Br J Anaesth. 2015;115:798.
Patel MS, Niemann CU, Sally MB, de la Cruz S, Zatarain J, Ewing T, et al. The impact of hydroxyethyl starch use in deceased organ donors on the development of delayed graft function in kidney transplant recipients: a propensity-adjusted analysis. Am J Transplant. 2015;15:2152–8.
Novitzky D, Cooper DKC, Rosendale JD, Kauffman HM. Hormonal therapy of the brain-dead organ donor: experimental and clinical studies. Transplantation. 2006;82:1396–401.
Buchanan IA, Mehta VA. Thyroid hormone resuscitation after brain death in potential organ donors: a primer for neurocritical care providers and narrative review of the literature. Clin Neurol Neurosurg. 2018;165:96–102.
Novitzky D, Mi Z, Sun Q, Collins JF, Cooper DK. Thyroid hormone therapy in the management of 63,593 brain-dead organ donors. Transplantation. 2014;98:1119–27.
Novitzky D, Cooper DK, Reichart B. The value of hormonal therapy in improving organ viability in the transplant donor. Transplant Proc. 1987;19:2037–8.
Venkateswaran RV, Steeds RP, Quinn DW, Nightingale P, Wilson IC, Mascaro JG, et al. The haemodynamic effects of adjunctive hormone therapy in potential heart donors: a prospective randomized double-blind factorially designed controlled trial. Eur Heart J. 2009;30:1771–80.
Macdonald PS, Aneman A, Bhonagiri D, Jones D, O'Callaghan G, Silvester W, et al. A systematic review and meta-analysis of clinical trials of thyroid hormone administration to brain dead potential organ donors. Crit Care Med. 2012;40:1635–44.
Benck U, Gottmann U, Hoeger S, et al. Donor desmopressin is associated with superior graft survival after kidney transplantation. Transplantation. 2011;92:1252–8.
Guesde R, Barrou B, Leblanc I, Ourahma S, Goarin JP, Coriat P, et al. Administration of desmopressin in brain-dead donors and renal function in kidney recipients. Lancet. 1998;352:1178–81.
Sally MB, Ewing T, Crutchfield M, et al. Determining optimal threshold for glucose control in organ donors after neurologic determination of death. J Trauma Acute Care Surg. 2014;76:62–9.
Nicolas-Robin A, Barouk JD, Darnal E, Riou B, Langeron O. Free cortisol and accuracy of total cortisol measurements in the diagnosis of adrenal insufficiency in brain-dead patients. Anesthesiology. 2011;115:568–74.
Barklin A. Systemic inflammation in the brain-dead organ donor. Acta Anaesthesiol Scand. 2009;53:425–35.
Kainz A, Wilflingseder J, Mitterbauer C, et al. Steroid pretreatment of organ donors to prevent Postischemic renal allograft failure. Ann Intern Med. 2010;153:222.
Reindl-Schwaighofer R, Kainz A, Jelencsics K, et al. Steroid pretreatment of organ donors does not impact on early rejection and long-term kidney allograft survival: results from a multicenter randomized, controlled trial. Am J Transplant. 2019;19:1770–6.
Dupuis S, Amiel J-A, Desgroseilliers M, et al. Corticosteroids in the management of brain-dead potential organ donors: a systematic review. Br J Anaesth. 2014;113:346–59.
D’Aragon F, Belley-Cote E, Agarwal A, et al. Effect of corticosteroid administration on neurologically deceased organ donors and transplant recipients: a systematic review and meta-analysis. BMJ Open. 2017;7:e014436.
Niemann CU, Feiner J, Swain S, Bunting S, Friedman M, Crutchfield M, et al. Therapeutic hypothermia in deceased organ donors and kidney-graft function. N Engl J Med. 2015;373:405–14.
Schnuelle P, Benck U, Krämer BK, et al. Impact of donor core body temperature on graft survival after heart transplantation. Transplantation. 2018;102:1891–900.
Cardinal H, Lamarche F, Grondin S, Marsolais P, Lagacé AM, Duca A, et al. Organ donor management and delayed graft function in kidney transplant recipients: a multicenter retrospective cohort study. Am J Transplant. 2019;19:277–84.
Patel MS, Zatarain J, De La Cruz S, et al. The impact of meeting donor management goals on the number of organs transplanted per expanded criteria donor. JAMA Surg. 2014;149:969.
Patel MS, De La Cruz S, Sally MB, et al. Active donor management during the hospital phase of care is associated with more organs transplanted per donor. J Am Coll Surg. 2017;225:525–31.
Hoeger S, Benck U, Petrov K, et al. Atorvastatin donor pre-treatment in a model of brain death and allogeneic kidney transplantation in rat. Ann Transplant. 17:79–85.
Tuuminen R, Nykänen AI, Saharinen P, Gautam P, Keränen MA, Arnaudova R, et al. Donor simvastatin treatment prevents ischemia–reperfusion and acute kidney injury by preserving microvascular barrier function. Am J Transplant. 2013;13:2019–34.
Orban J-C, Fontaine E, Cassuto E, et al. Effects of cyclosporine A pretreatment of deceased organ donors on kidney graft function (Cis-A-rein): study protocol for a randomized controlled trial. Trials. 2018;19:231.
Orban J-C, Quintard H, Cassuto E, et al. Effect of N-acetylcysteine pretreatment of deceased organ donors on renal allograft function. Transplantation. 2015;99:746–53.
de la Cruz JS, Sally MB, Zatarain JR, et al. The impact of blood transfusions in deceased organ donors on the outcomes of 1,884 renal grafts from United Network for Organ Sharing Region 5. J Trauma Acute Care Surg. 2015;79:S164–70.
Chen C-C, Chapman WC, Hanto DW. Ischemia–reperfusion injury in kidney transplantation. Front Biosci (Elite Ed). 2015;7:117–34.
Kosieradzki M, Rowiński W. Ischemia/reperfusion injury in kidney transplantation: mechanisms and prevention. Transplant Proc. 2008;40:3279–88.
Huang Y, Shan J, Wang C, Ma J, Li D, Li L, et al. Can ischemic preconditioning alone really protect organs from ischemia reperfusion injury in transplantation. Transpl Immunol. 2009;20:127–31.
Kitamura M. Endoplasmic reticulum stress and unfolded protein response in renal pathophysiology: Janus faces. Am J Physiol Physiol. 2008;295:F323–34.
Mitchell T, Saba H, Laakman J, Parajuli N, MacMillan-Crow L. Role of mitochondrial-derived oxidants in renal tubular cell cold-storage injury. Free Radic Biol Med. 2010;49:1273–82.
Woo Yang C, Jong Ahn H, Young Jung J, et al. Preconditioning with cyclosporine A or fk506 differentially regulates mitogen-activated protein kinase expression in rat kidneys with ischemia/reperfusion injury. Transplantation. 2003;75:20–4.
Yin T, Sandhu G, Wolfgang CD, Burrier A, Webb RL, Rigel DF, et al. Tissue-specific pattern of stress kinase activation in ischemic/reperfused heart and kidney. J Biol Chem. 1997;272:19943–50.
Hussein AE-AM, Shokeir AA, Sarhan ME, et al. Effects of combined erythropoietin and epidermal growth factor on renal ischaemia/reperfusion injury: a randomized experimental controlled study. BJU Int. 2011;107:323–8.
Araki M, Fahmy N, Zhou L, Kumon H, Krishnamurthi V, Goldfarb D, et al. Expression of IL-8 during reperfusion of renal allografts is dependent on ischemic time. Transplantation. 2006;81:783–8.
Chatauret N, Thuillier R, Hauet T. Preservation strategies to reduce ischemic injury in kidney transplantation: pharmacological and genetic approaches. Curr Opin Organ Transplant. 2011;16:180–7.
Ambros JT, Herrero-Fresneda I, Borau OG, Boira JM. Ischemic preconditioning in solid organ transplantation: from experimental to clinics. Transpl Int. 2007;20:219–29.
Murry CE, Jennings RB, Reimer KA. Preconditioning with ischemia: a delay of lethal cell injury in ischemic myocardium. Circulation. 1986;74:1124–36.
Torras J, Herrero-Fresneda I, Lloberas N, Riera M, Ma Cruzado J, Ma Grinyó J. Promising effects of ischemic preconditioning in renal transplantation. Kidney Int. 2002;61:2218–27.
Tsai BM, Wang M, March KL, Turrentine MW, Brown JW, Meldrum DR. Preconditioning: evolution of basic mechanisms to potential therapeutic strategies. Shock. 2004;21:195–209.
Selzner N, Boehnert M, Selzner M. Preconditioning, postconditioning, and remote conditioning in solid organ transplantation: basic mechanisms and translational applications. Transplant Rev. 2012;26:115–24.
Kosieradzki M, Ametani M, Southard JH, Mangino MJ. Is ischemic preconditioning of the kidney clinically relevant? Surgery. 2003;133:81–90.
Behrends M, Walz MK, Kribben A, et al. No protection of the porcine kidney by ischaemic preconditioning. Exp Physiol. 2000;85:819–27.
Yamasowa H, Shimizu S, Inoue T, Takaoka M, Matsumura Y. Endothelial nitric oxide contributes to the renal protective effects of ischemic preconditioning. J Pharmacol Exp Ther. 2005;312:153–9.
Park KM, Byun J-Y, Kramers C, Kim JI, Huang PL, Bonventre JV. Inducible nitric-oxide synthase is an important contributor to prolonged protective effects of ischemic preconditioning in the mouse kidney. J Biol Chem. 2003;278:27256–66.
Cao C, Wang S, Fan L, Wan X, Liu X, Chen X. Renal protection by ischemic preconditioning is associated with p50/p50 homodimers. Am J Nephrol. 2010;31:1–8.
Hill P, Shukla D, Tran MGB, Aragones J, Cook HT, Carmeliet P, et al. Inhibition of hypoxia inducible factor hydroxylases protects against renal ischemia–reperfusion injury. J Am Soc Nephrol. 2008;19:39–46.
van der Woude FJ, Schnuelle P, Yard BA. Preconditioning strategies to limit graft immunogenicity and cold ischemic organ injury. J Investig Med. 2004;52:323–9.
Wever KE, Menting TP, Rovers M, et al. Ischemic preconditioning in the animal kidney, a systematic review and meta-analysis. PLoS One. 2012;7:e32296.
Baker JE. Erythropoietin mimics ischemic preconditioning. Vasc Pharmacol. 2005;42:233–41.
Yang CW, Li C, Jung JY, Shin SJ, Choi BS, Lim SW, et al. Preconditioning with erythropoietin protects against subsequent ischemia–reperfusion injury in rat kidney. FASEB J. 2003;17:1754–5.
Ates E, Yalcin AU, Yilmaz S, et al. Protective effect of erythropoietin on renal ischemia and reperfusion injury. ANZ J Surg. 2005;75:1100–5.
Ishii Y, Sawada T, Murakami T, et al. Renoprotective effect of erythropoietin against ischaemia–reperfusion injury in a non-human primate model. Nephrol Dial Transplant. 2011;26:1157–62.
Moriyama MT, Tanaka T, Morita N, Ishii T, Chikazawa I, Suga K, et al. Renal protective effects of erythropoietin on ischemic reperfusion injury. Cell Transplant. 2010;19:713–21.
Nakao A, Faleo G, Shimizu H, et al. Ex vivo carbon monoxide prevents cytochrome P450 degradation and ischemia/reperfusion injury of kidney grafts. Kidney Int. 2008;74:1009–16.
Yoshida J, Ozaki KS, Nalesnik MA, Ueki S, Castillo-Rama M, Faleo G, et al. Ex vivo application of carbon monoxide in UW solution prevents transplant-induced renal ischemia/reperfusion injury in pigs. Am J Transplant. 2010;10:763–72.
Ozaki KS, Kimura S, Murase N. Use of carbon monoxide in minimizing ischemia/reperfusion injury in transplantation. Transplant Rev. 2012;26:125–39.
García-Cenador B, Blanco-Gozalo V, López-Montañés D, Sanz Giménez-Rico JR, López-Novoa JM, López-Hernández FJ. Cardiotrophin-1 improves kidney preservation, graft function, and survival in transplanted rats. Transplantation. 2018;102:e404–12.
Lobb I, Davison M, Carter D, et al. Hydrogen sulfide treatment mitigates renal allograft ischemia–reperfusion injury during cold storage and improves early transplant kidney function and survival following allogeneic renal transplantation. J Urol. 2015;194:1806–15.
Kim YO, Li C, Sun BK, Kim JS, Lim SW, Choi BS, et al. Preconditioning with 1,25-Dihydroxyvitamin D3 protects against subsequent ischemia–reperfusion injury in the rat kidney. Nephron Exp Nephrol. 2005;100:e85–94.
Kaizu T, Tamaki T, Tanaka M, Uchida Y, Tsuchihashi S, Kawamura A, et al. Preconditioning with tin-protoporphyrin IX attenuates ischemia/reperfusion injury in the rat kidney. Kidney Int. 2003;63:1393–403.
Herrero I, Torras J, Riera M, et al. Prevention of cold ischaemia–reperfusion injury by an endothelin receptor antagonist in experimental renal transplantation. Nephrol Dial Transplant. 1999;14:872–80.
Barber E, Menéndez S, León OS, Barber MO, Merino N, Calunga JL, et al. Prevention of renal injury after induction of ozone tolerance in rats submitted to warm ischaemia. Mediat Inflamm. 1999;8:37–41.
Lledó-García E, Subirá-Ríos D, Rodríguez–Martínez D, et al. Sildenafil as a protecting drug for warm ischemic kidney transplants: experimental results. J Urol. 2009;182:1222–5.
Starzl TE, Miller C, Broznick B, et al. An improved technique for multiple organ harvesting. Surg Gynecol Obstet. 1987;165:343–8.
Rosenthal JT, Shaw BW Jr, et al. Principles of multiple organ procurement from cadaver donors. Ann Surg. 1983;198:617.
Starzl TE, Hakala TR, Shaw BW, et al. A flexible procedure for multiple cadaveric organ procurement. Surg Gynecol Obstet. 1984;158:223–30.
Imagawa DK, Olthoff KM, Yersiz H, et al. Rapid en bloc technique for pancreas–liver procurement: improved early liver function. Transplantation. 1996;61:1605–9.
Wunderlich H, Brockmann JG, Voigt R, Rauchfuss F, Pascher A, Brose S, et al. DTG procurement guidelines in heart beating donors. Transpl Int. 2011;24:733–57.
Reich DJ, Mulligan DC, Abt PL, Pruett TL, Abecassis MM, D'Alessandro A, et al. ASTS recommended practice guidelines for controlled donation after cardiac death organ procurement and transplantation. Am J Transplant. 2009;9:2004–11.
Belli LS, De Carlis L, Romani F, et al. Kidney and liver initial graft function under different procurement techniques. Transplant Proc. 1989;21:1209–10.
Sánchez-Hidalgo JM, Rodríguez-Ortiz L, Arjona-Sánchez Á, Ayllón-Terán MD, Gómez-Luque I, Ciria-Bru R, et al. “Super-rapid” technique in donation after circulatory death liver donors: advantages and disadvantages. Transplant Proc. 2019;51:25–7.
Marconi L, Figueiredo A. Cadaver donor organ procurement: technical aspects and surgical options. In: Figueiredo A, Lledó-García E, editors. European textbook on kidney transplantation: ESTU-EAU; 2017. p. 303–3018.
Yilmaz M, Piskin T, Akbulut S, Ersan V, Gonultas F, Yilmaz S. Is routine sternotomy necessary for organ recovery from deceased donors? A comparative retrospective study. Transplant Proc. 2012;44:1644–7.
Southard JH, Belzer FO. Organ preservation. Annu Rev Med. 1995;46:235–47.
Stevens RB, Skorupa JY, Rigley TH, Yannam GR, Nielsen KJ, Schriner ME, et al. Increased primary non-function in transplanted deceased-donor kidneys flushed with histidine–tryptophan–ketoglutarate solution. Am J Transplant. 2009;9:1055–62.
Stewart ZA, Lonze BE, Warren DS, et al. Histidine–tryptophan–ketoglutarate (HTK) is associated with reduced graft survival of deceased donor kidney transplants. Am J Transplant. 2009;9:1048–54.
O’Callaghan JM, Knight SR, Morgan RD, et al. Preservation solutions for static cold storage of kidney allografts: a systematic review and meta-analysis. Am J Transplant. 2012;12:896–906.
Lynch RJ, Kubus J, Chenault RH, Pelletier SJ, Campbell DA, Englesbe MJ. Comparison of histidine–tryptophan–ketoglutarate and University of Wisconsin preservation in renal transplantation. Am J Transplant. 2008;8:567–73.
Nunes P, Mota A, Figueiredo A, Macário F, Rolo F, Dias V, et al. Efficacy of renal preservation: comparative study of Celsior and University of Wisconsin solutions. Transplant Proc. 2007;39:2478–9.
Tillou X, Collon S, Surga N, Jaureguy M, Viart L, Mazouz H, et al. Comparison of UW and Celsior: long-term results in kidney transplantation. Ann Transplant. 2013;18:146–52.
Dikdan GS, Mora-Esteves C, Koneru B. Review of randomized clinical trials of donor management and organ preservation in deceased donors. Transp J. 2012;94:425–41.
Mühlbacher F, Langer F, Mittermayer C. Preservation solutions for transplantation. Transplant Proc. 1999;31:2069–70.
Chatauret N, Coudroy R, Delpech PO, Vandebrouck C, Hosni S, Scepi M, et al. Mechanistic analysis of nonoxygenated hypothermic machine perfusion’s protection on warm ischemic kidney uncovers greater eNOS phosphorylation and vasodilation. Am J Transplant. 2014;14:2500–14.
Jochmans I, Nicholson ML, Hosgood SA. Kidney perfusion. Curr Opin Organ Transplant. 2017;22:260–6.
Moers C, Smits JM, Maathuis M-HJ, et al. Machine perfusion or cold storage in deceased-donor kidney transplantation. N Engl J Med. 2009;360:7–19.
Moers C, Pirenne J, Paul A, et al. Machine perfusion or cold storage in deceased-donor kidney transplantation. N Engl J Med. 2012;366:770–1.
Watson CJE, Wells AC, Roberts RJ, et al. Cold machine perfusion versus static cold storage of kidneys donated after cardiac death: a UK multicenter randomized controlled trial. Am J Transplant. 2010;10:1991–9.
Hosgood SA, Yang B, Bagul A, et al. A comparison of hypothermic machine perfusion versus static cold storage in an experimental model of renal ischemia reperfusion injury. Transplantation. 2010;89:830–7.
Jochmans I, Moers C, Smits JM, et al. Machine perfusion versus cold storage for the preservation of kidneys donated after cardiac death. Ann Surg. 2010;252:756–64.
Gallinat A, Moers C, Treckmann J, et al. Machine perfusion versus cold storage for the preservation of kidneys from donors ≥65 years allocated in the Eurotransplant Senior Programme. Nephrol Dial Transplant. 2012;27:4458–63.
Hameed AM, Pleass HC, Wong G, et al. Maximizing kidneys for transplantation using machine perfusion. Medicine (Baltimore). 2016;95:e5083.
O’Callaghan JM, Morgan RD, Knight SR, et al. Systematic review and meta-analysis of hypothermic machine perfusion versus static cold storage of kidney allografts on transplant outcomes. Br J Surg. 2013;100:991–1001.
Leite RR d A, Schanaider A, Da-Fonseca ER, et al. Máquina de perfusão versus armazenamento estático na preservação renal de doadores com morte encefálica: revisão sistemática e metanálise. Rev Col Bras Cir. 2019;46:e2079.
Martínez Arcos L, Fabuel Alcañiz JJ, Gómez Dos Santos V, Burgos Revilla FJ. Functional results of renal preservation in hypothermic pulsatile machine perfusion versus cold preservation: systematic review and meta-analysis of clinical trials. Transplant Proc. 2018;50:24–32.
Thuillier R, Delpy E, Matillon X, Kaminski J, Kasil A, Soussi D, et al. Preventing acute kidney injury during transplantation: the application of novel oxygen carriers. Expert Opin Investig Drugs. 2019;28:643–57.
Minor T, VonHorn C. Rewarming injury after cold preservation. Int J Mol Sci:20. Epub ahead of print 2019. https://doi.org/10.3390/ijms20092059.
Dragun D, Hoff U, Park J-K, et al. Prolonged cold preservation augments vascular injury independent of renal transplant immunogenicity and function. Kidney Int. 2001;60:1173–81.
Brinkkoetter P-T, Song H, Lösel R, et al. Hypothermic injury: the mitochondrial calcium, ATP and ROS love–hate triangle out of balance. Cell Physiol Biochem. 2008;22:195–204.
Thuillier R, Hauet T. Impact of hypothermia and oxygen deprivation on the cytoskeleton in organ preservation models. Biomed Res Int. 2018;2018:8926724.
Le Pape S, Pasini-Chabot O, Couturier P, et al. Decoding cold ischaemia time impact on kidney graft: the kinetics of the unfolded protein response pathways. Artif Cells, Nanomedicine, Biotechnol. 2018;46:S873–85.
Ratigan ED, McKay DB. Exploring principles of hibernation for organ preservation. Transplant Rev. 2016;30:13–9.
Hosgood SA, Nicholson HFL, Nicholson ML. Oxygenated kidney preservation techniques. Transplantation. 2012;93:455–9.
Treckmann J, Nagelschmidt M, Minor T, Saner F, Saad S, Paul A. Function and quality of kidneys after cold storage, machine perfusion, or retrograde oxygen persufflation: results from a porcine autotransplantation model. Cryobiology. 2009;59:19–23.
Gallinat A, Paul A, Efferz P, et al. Role of oxygenation in hypothermic machine perfusion of kidneys from heart beating donors. Transplantation. 2012;94:809–13.
O’Callaghan JM, Pall KT, Pengel LHM, et al. Supplemental oxygen during hypothermic kidney preservation: a systematic review. Transplant Rev. 2017;31:172–9.
Schopp I, Reissberg E, Lüer B, et al. Controlled rewarming after hypothermia: adding a new principle to renal preservation. Clin Transl Sci. 2015;8:475–8.
Mahboub P, Ottens P, Seelen M, et al. Gradual rewarming with gradual increase in pressure during machine perfusion after cold static preservation reduces kidney ischemia reperfusion injury. PLoS One. 2015;10:e0143859.
Hamar M, Urbanellis P, Kaths MJ, et al. Normothermic ex vivo kidney perfusion reduces warm ischemic injury of porcine kidney grafts retrieved after circulatory death. Transplantation. 102. Epub ahead of print 2018. https://doi.org/10.1097/TP.0000000000002245.
Nicholson ML, Hosgood SA. Renal transplantation after ex vivo normothermic perfusion: the first clinical study. Am J Transplant. 2013;13:1246–52.
Hosgood SA, Saeb-Parsy K, Hamed MO, Nicholson ML. Successful transplantation of human kidneys deemed untransplantable but resuscitated by ex vivo normothermic machine perfusion. Am J Transplant. 2016;16:3282–5.
Hosgood SA, Thompson E, Moore T, et al. Normothermic machine perfusion for the assessment and transplantation of declined human kidneys from donation after circulatory death donors. Br J Surg. 105. Epub ahead of print 2018. https://doi.org/10.1002/bjs.10733.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Edgar Tavares da Silva and Arnaldo Figueiredo each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of Topical Collection on Kidney Diseases
Rights and permissions
About this article
Cite this article
Tavares-da-Silva, E., Figueiredo, A. Renal Procurement: Techniques for Optimizing the Quality of the Graft in the Cadaveric Setting. Curr Urol Rep 21, 12 (2020). https://doi.org/10.1007/s11934-020-0963-8
Published:
DOI: https://doi.org/10.1007/s11934-020-0963-8