Abstract
Purpose of Review
In this article, we review why patients may fail medical therapy for benign prostatic hyperplasia (BPH) and by doing so, gain a better understanding of the disease process and how to optimize the care of these patients.
Recent Findings
A growing body of literature has attempted to better characterize the various mechanisms by which patients develop BPH as well as identify predictors of disease progression and treatment failure.
Summary
BPH is a heterogenous disease process. A more personalized approach to treatment, including patient selection for medical or surgical management, would allow us to optimize patient care.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Speakman M, Kirby R, Doyle S, Ioannou C. Burden of male lower urinary tract symptoms (LUTS) suggestive of benign prostatic hyperplasia (BPH) - focus on the UK. BJU Int. 2015;115:508–19. https://doi.org/10.1111/bju.12745.
Wei JT, Calhoun E, Jacobsen SJ. Urologic diseases in America project: benign prostatic hyperplasia. J Urol. 2005;173:1256–61. https://doi.org/10.1097/01.ju.0000155709.37840.fe.
Caine M, Pfau A, Perlberg S. The use of alpha-adrenergic blockers in benign prostatic obstruction. Br J Urol. 1976;48:255–63. https://doi.org/10.1111/j.1464-410X.1976.tb10214.x.
Lepor H, Tang R, Meretyk S, Shapiro E. Alpha1 adrenoceptor subtypes in the human prostate. J Urol. 1993;149(3):640–2. https://doi.org/10.1016/S0022-5347(17)36170-0.
Lepor H, Auerbach S, Puras-Baez A, Narayan P, Soloway M, Lowe F, et al. A randomized, placebo-controlled multicenter study of the efficacy and safety of terazosin in the treatment of benign prostatic hyperplasia. J Urol. 1992;148(5):1467–74. https://doi.org/10.1016/S0022-5347(17)36941-0.
Kahokehr A, Gilling PJ. Landmarks in BPH - from aetiology to medical and surgical management. Nat Rev Urol. 2014;11:118–22. https://doi.org/10.1038/nrurol.2013.318.
Marks LS. 5alpha-reductase: history and clinical importance. Rev Urol. 2004.
Okeigwe I, Kuohung W. 5-alpha reductase deficiency: a 40-year retrospective review. Curr Opin Endocrinol Diabetes Obes. 2014;21:483–7. https://doi.org/10.1097/MED.0000000000000116.
Gormley GJ, Stoner E, Bruskewitz RC, Imperato-McGinley J, Walsh PC, McConnell JD, et al. The effect of finasteride in men with benign prostatic hyperplasia. N Engl J Med. 1992;327:1185–91. https://doi.org/10.1056/NEJM199210223271701.
Narayan P, Tewari A. A second phase III multicenter placebo controlled study of 2 dosages of modified release tamsulosin in patients with symptoms of benign prostatic hyperplasia. J Urol. 1998;160:1701–6. https://doi.org/10.1016/S0022-5347(01)62386-3.
McVary KT, Roehrborn CG, Avins AL, et al. Update on AUA guideline on the management of benign prostatic hyperplasia. J Urol. 2011;185:1793–803. https://doi.org/10.1016/j.juro.2011.01.074.
Lepor H, Williford WO, Barry MJ, Brawer MK, Dixon CM, Gormley G, Haakenson C, Machi M, Narayan P, Padley RJ The efficacy of terazosin, finasteride, or both in benign prostatic hyperplasia. Veterans Affairs Cooperative Studies Benign Prostatic Hyperplasia Study Group. N Engl J Med 1996. doi:https://doi.org/10.1056/NEJM199608223350801, 335, 533, 540.
Kirby RS, Roehrborn C, Boyle P, Bartsch G, Jardin A, Cary MM, et al. Efficacy and tolerability of doxazosin and finasteride, alone or in combination, in treatment of symptomatic benign prostatic hyperplasia: the Prospective European Doxazosin and Combination Therapy (PREDICT) trial. Urology. 2003;61:119–26. https://doi.org/10.1016/S0090-4295(02)02114-3.
Lepor H. Phase III multicenter placebo-controlled study of tamsulosin in benign prostatic hyperplasia. Urology. 1998;51:892–900. https://doi.org/10.1016/S0090-4295(98)00126-5.
Roehrborn CG. Alfuzosin 10 mg once daily prevents overall clinical progression of benign prostatic hyperplasia but not acute urinary retention: results of a 2-year placebo-controlled study. BJU Int. 2006;97:734–41. https://doi.org/10.1111/j.1464-410X.2006.06110.x.
Marks LS, Gittelman MC, Hill LA, Volinn W, Hoel G. Rapid efficacy of the highly selective α1A-adrenoceptor antagonist silodosin in men with signs and symptoms of benign prostatic hyperplasia: pooled results of 2 phase 3 studies. J Urol. 2009;181:2634–40. https://doi.org/10.1016/j.juro.2009.02.034.
Nickel JC, Gilling P, Tammela TL, Morrill B, Wilson TH, Rittmaster RS. Comparison of dutasteride and finasteride for treating benign prostatic hyperplasia: the Enlarged Prostate International Comparator Study (EPICS). BJU Int. 2011;108:388–94. https://doi.org/10.1111/j.1464-410X.2011.10195.x.
Cindolo L, Berardinelli F, Fanizza C, Romero M, Pirozzi L, Tamburro FR, et al. Clinical effects and economical impact of dutasteride and finasteride therapy in Italian men with LUTS. Arch Ital di Urol e Androl. 2013;85:200–6. https://doi.org/10.4081/aiua.2013.4.200.
Kaplan SA, Chung DE, Lee RK, Scofield S, Te AE. A 5-year retrospective analysis of 5α-reductase inhibitors in men with benign prostatic hyperplasia: finasteride has comparable urinary symptom efficacy and prostate volume reduction, but less sexual side effects and breast complications than dutasteride. Int J Clin Pract. 2012;66:1052–5. https://doi.org/10.1111/j.1742-1241.2012.03010.x.
• Welk B, McArthur E, Ordon M, Anderson KK, Hayward J, Dixon S. Association of suicidality and depression with 5α-reductase inhibitors. JAMA Intern Med. 2017;177:683–91. https://doi.org/10.1001/jamainternmed.2017.0089. This large, matched cohort study raises awareness that depression may be a possible and until recently unknown side effect of 5ARIs. The results call into question our current practice patterns.
Pietrzyk B, Olszanecka-Glinianowicz M, Owczarek A, Gabryelewicz T, Almgren-Rachtan A, Prajsner A, et al. Depressive symptoms in patients diagnosed with benign prostatic hyperplasia. Int Urol Nephrol. 2015;47:431–40. https://doi.org/10.1007/s11255-015-0920-5.
Irwig MS. Depressive symptoms and suicidal thoughts among former users of finasteride with persistent sexual side effects. J Clin Psychiatry. 2012;73:1220–3. https://doi.org/10.4088/JCP.12m07887.
Duan Y, Grady JJ, Albertsen PC, Helen Wu Z. Tamsulosin and the risk of dementia in older men with benign prostatic hyperplasia. Pharmacoepidemiol Drug Saf. 2018;27:340–8. https://doi.org/10.1002/pds.4361.
Tae BS, Jeon JJ, Choi H, Cheon J, Park JY, Base JH. Alpha-blocker and risk of dementia in patients with benign prostate hyperplasia: a nationwide population-based study using the National Health Insurance Service database. J Urol. 2019.
McVary KT, Roehrborn CG, Kaminetsky JC, et al. Tadalafil relieves lower urinary tract symptoms secondary to benign prostatic hyperplasia. J Urol. 2007;177:1401–7. https://doi.org/10.1016/j.juro.2006.11.037.
McVary KT, Monnig W, Camps JL, Young JM, Tseng LJ, van den Ende G. Sildenafil citrate improves erectile function and urinary symptoms in men with erectile dysfunction and lower urinary tract symptoms associated with benign prostatic hyperplasia: a randomized, double-blind trial. J Urol. 2007;177:1071–7. https://doi.org/10.1016/j.juro.2006.10.055.
Stief CG, Porst H, Neuser D, Beneke M, Ulbrich E. A randomised, placebo-controlled study to assess the efficacy of twice-daily vardenafil in the treatment of lower urinary tract symptoms secondary to benign prostatic hyperplasia. Eur Urol. 2008;53:1236–44. https://doi.org/10.1016/j.eururo.2008.01.075.
Brock GB, McVary KT, Roehrborn CG, et al. Direct effects of tadalafil on lower urinary tract symptoms versus indirect effects mediated through erectile dysfunction symptom improvement: integrated data analyses from 4 placebo controlled clinical studies. J Urol. 2014;191:405–11. https://doi.org/10.1016/j.juro.2013.09.057.
Gravas S, T. Bach AB, M. Drake, M. Gacci.2016 Management of non-neurogenic male lower urinary tract symptoms (LUTS), incl. benign prostatic obstruction (BPO). In: European Association of Urology 2016. doi:https://doi.org/10.1017/CBO9781107415324.004.
Kaplan SA, Roehrborn CG, Rovner ES, Carlsson M, Bavendam T, Guan Z. Tolterodine and tamsulosin for treatment of men with lower urinary tract symptoms and overactive bladder: a randomized controlled trial. J Am Med Assoc. 2006;296:2319–28. https://doi.org/10.1001/jama.296.19.2319.
McConnell JD, Roehrborn CG, Bautista OM, Andriole GL Jr, Dixon CM, Kusek JW, et al. The long-term effect of doxazosin, finasteride, and combination therapy on the clinical progression of benign prostatic hyperplasia. N Engl J Med. 2003;349:2387–98. https://doi.org/10.1056/NEJMoa030656.
Kaplan SA, McConnell JD, Roehrborn CG, et al. Combination therapy with doxazosin and finasteride for benign prostatic hyperplasia in patients with lower urinary tract symptoms and a baseline total prostate volume of 25 ml or greater. J Urol. 2006;175:217–20. https://doi.org/10.1016/S0022-5347(05)00041-8.
Roehrborn CG, Siami P, Barkin J, Damião R, Major-Walker K, Nandy I, et al. The effects of combination therapy with dutasteride and tamsulosin on clinical outcomes in men with symptomatic benign prostatic hyperplasia: 4-year results from the CombAT study. Eur Urol. 2010;57:123–31. https://doi.org/10.1016/j.eururo.2009.09.035.
Verhamme KMC, Dieleman JP, Bleumink GS, Bosch JLHR, Stricker BHC, Sturkenboom MCJM. Treatment strategies, patterns of drug use and treatment discontinuation in men with LUTS suggestive of benign prostatic hyperplasia: the Triumph project. Eur Urol. 2003;44:539–45. https://doi.org/10.1016/S0302-2838(03)00376-2.
Nichol MB, Knight TK, Wu J, Barron R, Penson DF. Evaluating use patterns of and adherence to medications for benign prostatic hyperplasia. J Urol. 2009;181:2214–22. https://doi.org/10.1016/j.juro.2009.01.033.
Cindolo L, Pirozzi L, Fanizza C, Romero M, Tubaro A, Autorino R, et al. Drug adherence and clinical outcomes for patients under pharmacological therapy for lower urinary tract symptoms related to benign prostatic hyperplasia: population-based cohort study. Eur Urol. 2015;68:418–25. https://doi.org/10.1016/j.eururo.2014.11.006.
Shapiro E, Hartanto V, Lepor H. The response to alpha blockade in benign prostatic hyperplasia is related to the percent area density of prostate smooth muscle. Prostate. 1992;21:297–307. https://doi.org/10.1002/pros.2990210406.
Kojima Y, Sasaki S, Kubota Y, Hayase M, Hayashi Y, Shinoura H, et al. Expression of α1-adrenoceptor subtype mRNA as a predictor of the efficacy of subtype selective α1-adrenoceptor antagonists in the management of benign prostatic hyperplasia. J Urol. 2008;179:1040–6. https://doi.org/10.1016/j.juro.2007.10.082.
Niu Y, Ge R, Hu L, Diaz C, Wang Z, Wu CL, et al. Reduced levels of 5-α reductase 2 in adult prostate tissue and implications for BPH therapy. Prostate. 2011. https://doi.org/10.1002/pros.21348.
Bechis SK, Otsetov AG, Ge R, Wang Z, Vangel MG, Wu CL, et al. Age and obesity promote methylation and suppression of 5α-reductase 2: implications for personalized therapy of benign prostatic hyperplasia. J Urol. 2015;194:1031–7. https://doi.org/10.1016/j.juro.2015.04.079.
Kang PM, Kim YJ, Seo WT, et al. Correlation between 5-α reductase type 2 protein expression and methylation of 5-α reductase type 2 promotor gene of benign prostatic hyperplasia. World J Urol. 2018.
Gu X, Na R, Huang T, Wang L, Tao S, Tian L, et al. SRD5A1 and SRD5A2 are associated with treatment for benign prostatic hyperplasia with the combination of 5α-reductase inhibitors and α-adrenergic receptor antagonists. J Urol. 2013;190:615–9. https://doi.org/10.1016/j.juro.2013.03.024.
Ribal MJ. The link between benign prostatic hyperplasia and inflammation. Eur Urol Suppl. 2013;12:103–9. https://doi.org/10.1016/j.eursup.2013.08.001.
Robert G, Descazeaud A, Nicolaïew N, Terry S, Sirab N, Vacherot F, et al. Inflammation in benign prostatic hyperplasia: a 282 patients’ immunohistochemical analysis. Prostate. 2009;69:1774–80. https://doi.org/10.1002/pros.21027.
Chughtai B, Lee R, Te A, Kaplan S. Role of inflammation in benign prostatic hyperplasia. Rev Urol. 2011. https://doi.org/10.3909/riu0535.
Mishra VC, Allen DJ, Nicolaou C, Sharif H, Hudd C, Karim OMA, et al. Does intraprostatic inflammation have a role in the pathogenesis and progression of benign prostatic hyperplasia? BJU Int. 2007;100:327–31. https://doi.org/10.1111/j.1464-410X.2007.06910.x.
• Albisinni S, Biaou I, Marcelis Q, Aoun F, De Nunzio C, Roumeguère T. New medical treatments for lower urinary tract symptoms due to benign prostatic hyperplasia and future perspectives. BMC Urol. 2016;16:58. https://doi.org/10.1186/s12894-016-0176-0. An excellent review of current treatments for BPH, recent advances in our understanding BPH pathophysiology, and potential therapeutic targets.
Kahokehr A, Vather R, Nixon A, Hill AG. Non-steroidal anti-inflammatory drugs for lower urinary tract symptoms in benign prostatic hyperplasia: systematic review and meta-analysis of randomized controlled trials. BJU Int. 2013;111:304–11. https://doi.org/10.1111/j.1464-410X.2012.11559.x.
Kozminski MA, Wei JT, Nelson J, Kent DM. Baseline characteristics predict risk of progression and response to combined medical therapy for benign prostatic hyperplasia (BPH). BJU Int. 2015;115:308–18. https://doi.org/10.1111/bju.12802.
Crawford ED, Wilson SS, McConnell JD, et al. Baseline factors as predictors of clinical progression of benign prostatic hyperplasia in men treated with placebo. J Urol. 2006;175:1422–7. https://doi.org/10.1016/S0022-5347(05)00708-1.
Djavan B, Nickel JC, De La Rosette J, Abrams P. The urologist view of BPH progression: results of an international survey. Eur Urol. 2002;84:1729–41. https://doi.org/10.1177/0040517514528565.
Mondul AM, Giovannucci E, Platz EA. A prospective study of obesity, and the incidence and progression of lower urinary tract symptoms. J Urol. 2014;191:715–21. https://doi.org/10.1016/j.juro.2013.08.110.
Trachtenberg J. Treatment of lower urinary tract symptoms suggestive of benign prostatic hyperplasia in relation to the patient’s risk profile for progression. BJU Int Suppl. 2005;95:6–11. https://doi.org/10.1111/j.1464-410X.2005.05488.x.
Martin S, Lange K, Haren MT, Taylor AW, Wittert G. Risk factors for progression or improvement of lower urinary tract symptoms in a prospective cohort of men. J Urol. 2014;191:130–7. https://doi.org/10.1016/j.juro.2013.06.018.
Torkko KC, Wilson RS, Smith EE, Kusek JW, Van Bokhoven A, Lucia MS. Prostate biopsy markers of inflammation are associated with risk of clinical progression of benign prostatic hyperplasia: findings from the MTOPS study. J Urol. 2015;194:454–61. https://doi.org/10.1016/j.juro.2015.03.103.
RC G, KS A, NW D, et al. 1277: the impact of acute or chronic inflammation in baseline biopsy on the risk of clinical progression of BPH: results from the MTOPS study. J Urol. 2005;173(4s):346. https://doi.org/10.1016/S0022-5347(18)35422-3.
• Nickel JC, Roehrborn CG, Castro-Santamaria R, Freedland SJ, Moreira DM. Chronic prostate inflammation is associated with severity and progression of benign prostatic hyperplasia, lower urinary tract symptoms and risk of acute urinary retention. J Urol. 2016. https://doi.org/10.1016/j.juro.2016.06.090 One of the largest studies, with long-term follow-up, that evaluates the association between prostatic inflammation and LUTS and confirms the relevance of inflammation as a potential therapeutic target.
Hong SJ, Ko WJ, Kim S II, Chung BH, Djavan B. Identification of baseline clinical factors which predict medical treatment failure of benign prostatic hyperplasia: an observational cohort study. Eur Urol. 2003;44:94–100. https://doi.org/10.1016/S0302-2838(03)00199-4.
Hong KP, Byun YJ, Yoon H, Park YY, Chung WS. Prospective factor analysis of alpha blocker monotherapy failure in benign prostatic hyperplasia. Korean J Urol. 2010;51:488–91. https://doi.org/10.4111/kju.2010.51.7.488.
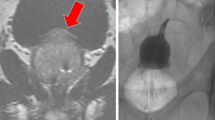
Hirayama K, Masui K, Hamada A, Shichiri Y, Masuzawa N, Hamada S. Evaluation of intravesical prostatic protrusion as a predictor of dutasteride-resistant lower urinary tract symptoms/benign prostatic enlargement with a high likelihood of surgical intervention. Urology. 2015;86:565–9. https://doi.org/10.1016/j.urology.2015.05.021.
• Kalkanli A, Tandogdu Z, Aydin M, Karaca AS, Hazar AI, Balci MBC, et al. Intravesical prostatic protrusion: a potential marker of alpha-blocker treatment success in patients with benign prostatic enlargement. Urology. 2016. https://doi.org/10.1016/j.urology.2015.11.029 Demonstrates that IPP is negatively associated with improvements in IPPS scores after taking alpha-blockers. We believe that patients with significant IPP are likely to benefit more from surgery than medical management.
Topazio L, Perugia C, De Nunzio C, et al. Intravescical prostatic protrusion is a predictor of alpha blockers response: results from an observational study. BMC Urol. 2018;18:6. https://doi.org/10.1186/s12894-018-0320-0.
Ahmed AF. Sonographic parameters predicting the outcome of patients with lower urinary tract symptoms/benign prostatic hyperplasia treated with alpha1-adrenoreceptor antagonist. Urology. 2016;88:143–8. https://doi.org/10.1016/j.urology.2015.11.017.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Zeynep G. Gul and Steven A. Kaplan each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Benign Prostatic Hyperplasia
Rights and permissions
About this article
Cite this article
Gul, Z.G., Kaplan, S.A. BPH: Why Do Patients Fail Medical Therapy?. Curr Urol Rep 20, 40 (2019). https://doi.org/10.1007/s11934-019-0899-z
Published:
DOI: https://doi.org/10.1007/s11934-019-0899-z