Abstract
Purpose of Review
Male factor infertility is a complex and multifaceted problem facing the modern urologist and is identified in 30–40% of infertile couples. This review focuses on the use of ultrasound, as an adjunct screening tool, in the initial evaluation of male infertility.
Recent Findings
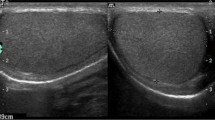
Access to male reproductive urologist for assessment of male infertility is limited and about a quarter of infertile couples do not complete the male component in their infertility assessment. Ultrasound evaluation of the infertile male is low-cost and non-invasive and helps uncover underlying pathologies that may be missed during the initial assessment. The addition of ultrasound allows the physician to accurately assess testicular anatomy and dimensions, as well as vascular environments, which may help guide treatment decisions.
Summary
Scrotal ultrasound evaluation, in conjunction with a semen analysis and as an adjunct to physical exam, can be offered in the initial assessment of men who present for infertility consultation given its low cost, non-invasive nature, and ability to detect and discriminate between various etiologies of male infertility. Further, when directed by physical exam and semen analysis findings, it provides a valuable tool to select men for referral to a reproductive urologist, especially for infertile couples who are only screened by reproductive endocrinologists and female infertility specialists.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Thoma ME, McLain AC, Louis JF, King RB, Trumble AC, Sundaram R, et al. Prevalence of infertility in the United States as estimated by the current duration approach and a traditional constructed approach. Fertil Steril. 2013;99(5):1324–31 e1. https://doi.org/10.1016/j.fertnstert.2012.11.037. 15.5% of couples struggle with fertility.
Chandra A, Martinez GM, Mosher WD, Abma JC, Jones J. Fertility, family planning, and reproductive health of U.S. women: data from the 2002 National Survey of Family Growth. Vital Health Stat. 2005;23(25):1–160.
Center for Disease Control and Prevention. Reproductive Health. https://www.cdc.gov/reproductivehealth/infertility/index.htm. Accessed 12 Jan 2018 2018.
Thonneau P, Marchand S, Tallec A, Ferial ML, Ducot B, Lansac J, et al. Incidence and main causes of infertility in a resident population (1,850,000) of three French regions (1988-1989). Hum Reprod. 1991;6(6):811–6.
Practice Committee of the American Society for Reproductive Medicine. Diagnostic evaluation of the infertile male: a committee opinion. Fertil Steril. 2015;103(3):e18–25. https://doi.org/10.1016/j.fertnstert.2014.12.103.
Sigman M. Infertility in the male. 4th ed. Cambridge University press; 2009.
Niederberger CS. Campbell-Walsh urology. 11th ed. Philadelphia: Elsevier.
• Hotaling JM. Genetics of male infertility. Urol Clin N Am. 2014;41(1):1–17. https://doi.org/10.1016/j.ucl.2013.08.009. Genetic and epigenetic perturbations play an important role in male infertility.
•• Eisenberg ML, Lathi RB, Baker VL, Westphal LM, Milki AA, Nangia AK. Frequency of the male infertility evaluation: data from the national survey of family growth. J Urol. 2013;189(3):1030–4. https://doi.org/10.1016/j.juro.2012.08.239. Access to male infertility specialist is disparate and limited in the USA and 18–27% of couples do not complete assessment of the male infertility component.
Mehta A, Nangia AK, Dupree JM, Smith JF. Limitations and barriers in access to care for male factor infertility. Fertil Steril. 2016;105(5):1128–37. https://doi.org/10.1016/j.fertnstert.2016.03.023.
Honig SC, Lipshultz LI, Jarow J. Significant medical pathology uncovered by a comprehensive male infertility evaluation. Fertil Steril. 1994;62(5):1028–34.
Kolettis PN, Sabanegh ES. Significant medical pathology discovered during a male infertility evaluation. J Urol. 2001;166(1):178–80.
Middleton WD, Thorne DA, Melson GL. Color Doppler ultrasound of the normal testis. AJR Am J Roentgenol. 1989;152(2):293–7. https://doi.org/10.2214/ajr.152.2.293.
Pinggera GM, Mitterberger M, Bartsch G, Strasser H, Gradl J, Aigner F, et al. Assessment of the intratesticular resistive index by colour Doppler ultrasonography measurements as a predictor of spermatogenesis. BJU Int. 2008;101(6):722–6. https://doi.org/10.1111/j.1464-410X.2007.07343.x.
Unsal A, Turgut AT, Taskin F, Kosar U, Karaman CZ. Resistance and pulsatility index increase in capsular branches of testicular artery: indicator of impaired testicular microcirculation in varicocele? J Clin Ultrasound. 2007;35(4):191–5. https://doi.org/10.1002/jcu.20331.
• Hillelsohn JH, Chuang KW, Goldenberg E, Gilbert BR. Spectral Doppler sonography: a noninvasive method for predicting dyspermia. J Ultrasound Med. 2013;32(8):1427–32. https://doi.org/10.7863/ultra.32.8.1427. The authors suggest that a testicular vascular resistive index of > 0.6 is associated with impaired spermatogenesis.
Balci A, Karazincir S, Gorur S, Sumbas H, Egilmez E, Inandi T. Long-term effect of varicocele repair on intratesticular arterial resistance index. J Clin Ultrasound. 2008;36(3):148–52. https://doi.org/10.1002/jcu.20439.
Biagiotti G, Cavallini G, Modenini F, Vitali G, Gianaroli L. Spermatogenesis and spectral echo-colour Doppler traces from the main testicular artery. BJU Int. 2002;90(9):903–8.
Sakamoto H, Ogawa Y. Does a clinical varicocele influence the relationship between testicular volume by ultrasound and testicular function in patients with infertility? Fertil Steril. 2009;92(5):1632–7. https://doi.org/10.1016/j.fertnstert.2008.08.105.
Sakamoto H, Yajima T, Nagata M, Okumura T, Suzuki K, Ogawa Y. Relationship between testicular size by ultrasonography and testicular function: measurement of testicular length, width, and depth in patients with infertility. Int J Urol. 2008;15(6):529–33. https://doi.org/10.1111/j.1442-2042.2008.02071.x.
Du J, Li FH, Guo YF, Yang LM, Zheng JF, Chen B, et al. Differential diagnosis of azoospermia and etiologic classification of obstructive azoospermia: role of scrotal and transrectal US. Radiology. 2010;256(2):493–503. https://doi.org/10.1148/radiol.10091578.
Moon MH, Kim SH, Cho JY, Seo JT, Chun YK. Scrotal US for evaluation of infertile men with azoospermia. Radiology. 2006;239(1):168–73. https://doi.org/10.1148/radiol.2391050272.
Hung AJ, King P, Schlegel PN. Uniform testicular maturation arrest: a unique subset of men with nonobstructive azoospermia. J Urol. 2007;178(2):608–12; discussion 12. https://doi.org/10.1016/j.juro.2007.03.125.
Sakamoto H, Saito K, Ogawa Y, Yoshida H. Testicular volume measurements using Prader orchidometer versus ultrasonography in patients with infertility. Urology. 2007;69(1):158–62. https://doi.org/10.1016/j.urology.2006.09.013.
Sakamoto H, Ogawa Y, Yoshida H. Relationship between testicular volume and testicular function: comparison of the Prader orchidometric and ultrasonographic measurements in patients with infertility. Asian J Androl. 2008;10(2):319–24. https://doi.org/10.1111/j.1745-7262.2008.00340.x.
Sakamoto H, Ogawa Y, Yoshida H. Relationship between testicular volume and varicocele in patients with infertility. Urology. 2008;71(1):104–9. https://doi.org/10.1016/j.urology.2007.08.019.
Diamond DA, Zurakowski D, Bauer SB, Borer JG, Peters CA, Cilento BG Jr, et al. Relationship of varicocele grade and testicular hypotrophy to semen parameters in adolescents. J Urol. 2007;178(4 Pt 2):1584–8. https://doi.org/10.1016/j.juro.2007.03.169.
•• Kurtz MP, Zurakowski D, Rosoklija I, Bauer SB, Borer JG, Johnson KL, et al. Semen parameters in adolescents with varicocele: association with testis volume differential and total testis volume. J Urol. 2015;193(5 Suppl):1843–7. https://doi.org/10.1016/j.juro.2014.10.111. Decreased testicular volume in adolescents with varicocele increases risk for lower sperm counts.
Herwig R, Tosun K, Schuster A, Rehder P, Glodny B, Wildt L, et al. Tissue perfusion-controlled guided biopsies are essential for the outcome of testicular sperm extraction. Fertil Steril. 2007;87(5):1071–6. https://doi.org/10.1016/j.fertnstert.2006.10.010.
Eytan O, Har-Toov J, Fait G, Yavetz H, Hauser R, Yogev L, et al. Vascularity index distribution within the testis: a technique for guiding testicular sperm extraction. Ultrasound Med Biol. 2001;27(9):1171–6.
Nowroozi MR, Ayati M, Amini E, Radkhah K, Jamshidian H, Delpazir A, et al. Assessment of testicular perfusion prior to sperm extraction predicts success rate and decreases the number of required biopsies in patients with non-obstructive azoospermia. Int Urol Nephrol. 2015;47(1):53–8. https://doi.org/10.1007/s11255-014-0856-1.
Altinkilic B, Pilatz A, Diemer T, Wolf J, Bergmann M, Schonbrunn S, et al. Prospective evaluation of scrotal ultrasound and intratesticular perfusion by color-coded duplex sonography (CCDS) in TESE patients with azoospermia. World J Urol. 2018;36(1):125–33. https://doi.org/10.1007/s00345-017-2039-z.
Gat Y, Zukerman Z, Chakraborty J, Gornish M. Varicocele, hypoxia and male infertility. Fluid mechanics analysis of the impaired testicular venous drainage system. Hum Reprod. 2005;20(9):2614–9. https://doi.org/10.1093/humrep/dei089.
Ali JI, Weaver DJ, Weinstein SH, Grimes EM. Scrotal temperature and semen quality in men with and without varicocele. Arch Androl. 1990;24(2):215–9.
Goldstein M, Eid JF. Elevation of intratesticular and scrotal skin surface temperature in men with varicocele. J Urol. 1989;142(3):743–5.
Zorgniotti AW, Macleod J. Studies in temperature, human semen quality, and varicocele. Fertil Steril. 1973;24(11):854–63.
Garolla A, Torino M, Sartini B, Cosci I, Patassini C, Carraro U, et al. Seminal and molecular evidence that sauna exposure affects human spermatogenesis. Hum Reprod. 2013;28(4):877–85. https://doi.org/10.1093/humrep/det020.
• Garolla A, Torino M, Miola P, Caretta N, Pizzol D, Menegazzo M, et al. Twenty-four-hour monitoring of scrotal temperature in obese men and men with a varicocele as a mirror of spermatogenic function. Hum Reprod. 2015;30(5):1006–13. https://doi.org/10.1093/humrep/dev057. Elevated scrotal temperature associated with varicocele negatively impacts sperm quality.
Gat Y, Bachar GN, Everaert K, Levinger U, Gornish M. Induction of spermatogenesis in azoospermic men after internal spermatic vein embolization for the treatment of varicocele. Hum Reprod. 2005;20(4):1013–7. https://doi.org/10.1093/humrep/deh706.
Gorelick JI, Goldstein M. Loss of fertility in men with varicocele. Fertil Steril. 1993;59(3):613–6.
Schauer I, Madersbacher S, Jost R, Hubner WA, Imhof M. The impact of varicocelectomy on sperm parameters: a meta-analysis. J Urol. 2012;187(5):1540–7. https://doi.org/10.1016/j.juro.2011.12.084.
•• Locke JA, Noparast M, Afshar K. Treatment of varicocele in children and adolescents: a systematic review and meta-analysis of randomized controlled trials. J Pediatr Urol. 2017;13(5):437–45. https://doi.org/10.1016/j.jpurol.2017.07.008. Compared to conservative treatment, there is improvement in semen parameters with varicocele repair.
Sakamoto H, Saito K, Ogawa Y, Yoshida H. Effects of varicocele repair in adults on ultrasonographically determined testicular volume and on semen profile. Urology. 2008;71(3):485–9. https://doi.org/10.1016/j.urology.2007.11.040.
Zucchi A, Mearini L, Mearini E, Fioretti F, Bini V, Porena M. Varicocele and fertility: relationship between testicular volume and seminal parameters before and after treatment. J Androl. 2006;27(4):548–51. https://doi.org/10.2164/jandrol.05200.
Kroese AC, de Lange NM, Collins J, Evers JL. Surgery or embolization for varicoceles in subfertile men. Cochrane Database Syst Rev. 2012;10:CD000479. https://doi.org/10.1002/14651858.CD000479.pub5.
Kohn TP, Kohn JR, Pastuszak AW. Varicocelectomy before assisted reproductive technology: are outcomes improved? Fertil Steril. 2017;108(3):385–91. https://doi.org/10.1016/j.fertnstert.2017.06.033.
• Esteves SC, Roque M, Agarwal A. Outcome of assisted reproductive technology in men with treated and untreated varicocele: systematic review and meta-analysis. Asian J Androl. 2016;18(2):254–8. https://doi.org/10.4103/1008-682X.163269. Varicocele repair may improve outcomes of assisted reproductive techniques.
Gat Y, Bachar GN, Zukerman Z, Belenky A, Gorenish M. Physical examination may miss the diagnosis of bilateral varicocele: a comparative study of 4 diagnostic modalities. J Urol. 2004;172(4 Pt 1):1414–7.
Hoekstra T, Witt MA. The correlation of internal spermatic vein palpability with ultrasonographic diameter and reversal of venous flow. J Urol. 1995;153(1):82–4. https://doi.org/10.1097/00005392-199501000-00029.
Schiff JD, Li PS, Goldstein M. Correlation of ultrasound-measured venous size and reversal of flow with Valsalva with improvement in semen-analysis parameters after varicocelectomy. Fertil Steril. 2006;86(1):250–2. https://doi.org/10.1016/j.fertnstert.2005.12.038.
•• Kim HJ, Seo JT, Kim KJ, Ahn H, Jeong JY, Kim JH, et al. Clinical significance of subclinical varicocelectomy in male infertility: systematic review and meta-analysis. Andrologia. 2016;48(6):654–61. https://doi.org/10.1111/and.12495. The authors revisit the significance of subclinical varicoceles and suggest that treatment of subclinical varicoceles may improve semen parameters and fertility.
Cantoro U, Polito M, Muzzonigro G. Reassessing the role of subclinical varicocele in infertile men with impaired semen quality: a prospective study. Urology. 2015;85(4):826–30. https://doi.org/10.1016/j.urology.2015.01.015.
Schoor RA, Elhanbly S, Niederberger CS, Ross LS. The role of testicular biopsy in the modern management of male infertility. J Urol. 2002;167(1):197–200.
Donkol RH. Imaging in male-factor obstructive infertility. World J Radiol. 2010;2(5):172–9. https://doi.org/10.4329/wjr.v2.i5.172.
Abdulwahed SR, Mohamed EE, Taha EA, Saleh MA, Abdelsalam YM, ElGanainy EO. Sensitivity and specificity of ultrasonography in predicting etiology of azoospermia. Urology. 2013;81(5):967–71. https://doi.org/10.1016/j.urology.2013.01.001.
Jarow JP, Sigman M, Kolettis L, Lipshultz LI, McClure D, Nangia A. AUA Best practice statements: the optimal evaluation of the infertile male: Americal Urological Association 2011.
Pezzella A, Barbonetti A, D'Andrea S, Necozione S, Micillo A, Di Gregorio A, et al. Ultrasonographic caput epididymis diameter is reduced in non-obstructive azoospermia compared with normozoospermia but is not predictive for successful sperm retrieval after TESE. Hum Reprod. 2014;29(7):1368–74. https://doi.org/10.1093/humrep/deu092.
Pezzella A, Barbonetti A, Micillo A, D'Andrea S, Necozione S, Gandini L, et al. Ultrasonographic determination of caput epididymis diameter is strongly predictive of obstruction in the genital tract in azoospermic men with normal serum FSH. Andrology. 2013;1(1):133–8. https://doi.org/10.1111/j.2047-2927.2012.00010.x.
Onur MR, Firdolas F, Onur R, Kocakoc E, Akpolat N, Orhan I. Scrotal ultrasonography: should it be used in routine evaluation of infertile men? Andrologia. 2008;40(1):58–61. https://doi.org/10.1111/j.1439-0272.2008.00812.x.
•• Hanson BM, Eisenberg ML, Hotaling JM. Male infertility: a biomarker of individual and familial cancer risk. Fertil Steril. 2018;109(1):6–19. https://doi.org/10.1016/j.fertnstert.2017.11.005. Infertility may be a biomarker for cancer and the detailed work-up of infertile males should be given significant consideration.
Paduch DA. Testicular cancer and male infertility. Curr Opin Urol. 2006;16(6):419–27. https://doi.org/10.1097/01.mou.0000250282.37366.d2.
Carmignani L, Gadda F, Mancini M, Gazzano G, Nerva F, Rocco F, et al. Detection of testicular ultrasonographic lesions in severe male infertility. J Urol. 2004;172(3):1045–7. https://doi.org/10.1097/01.ju.0000134892.10525.39.
Inhorn MC, Patrizio P. Infertility around the globe: new thinking on gender, reproductive technologies and global movements in the 21st century. Hum Reprod Update. 2015;21(4):411–26. https://doi.org/10.1093/humupd/dmv016.
World Health Organization. Infertility is a global public health issue. 2018. http://www.who.int/reproductivehealth/topics/infertility/perspective/en/. 2018.
Pierik FH, Dohle GR, van Muiswinkel JM, Vreeburg JT, Weber RF. Is routine scrotal ultrasound advantageous in infertile men? J Urol. 1999;162(5):1618–20.
Sakamoto H, Saito K, Shichizyo T, Ishikawa K, Igarashi A, Yoshida H. Color Doppler ultrasonography as a routine clinical examination in male infertility. Int J Urol. 2006;13(8):1073–8. https://doi.org/10.1111/j.1442-2042.2006.01499.x.
Healthcare Bluebook. https://www.healthcarebluebook.com/page_Default.aspx. Accessed March 2018.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Joseph M. Armstrong, Sorena Keihani, and James M. Hotaling each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Men’s Health
Rights and permissions
About this article
Cite this article
Armstrong, J.M., Keihani, S. & Hotaling, J.M. Use of Ultrasound in Male Infertility: Appropriate Selection of Men for Scrotal Ultrasound. Curr Urol Rep 19, 58 (2018). https://doi.org/10.1007/s11934-018-0810-3
Published:
DOI: https://doi.org/10.1007/s11934-018-0810-3