Abstract
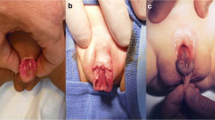
The exstrophy–epispadias complex is a rare congenital malformation of the genitourinary system, abdominal wall musculature, and pelvic bones. Historically, surgical outcomes in patients with classic bladder exstrophy, the most common presentation of the exstrophy–epispadias complex, were poor. However, modern techniques have increased the success of achieving urinary continence, satisfactory cosmesis, and improved quality of life. Still, recent studies recognize complications that may occur during management of these patients. This review provides readers with an overview of the exstrophy–epispadias complex, the modern management of bladder exstrophy, and potential surgical complications.
Similar content being viewed by others
Abbreviations
- EEC:
-
Exstrophy–epispadias complex
- CBE:
-
Classic bladder exstrophy
- OEIS:
-
Omphalocele, exstrophy, imperforate anus, spinal abnormalities
- VUR:
-
Vesicoureteral reflux
- MRI:
-
Magnetic resonance imaging
- CIC:
-
Clean intermittent catheterization
- MSRE:
-
Modern staged repair of exstrophy
- CPRE:
-
Complete primary repair of exstrophy
- BNR:
-
Bladder neck reconstruction
- CUD:
-
Continent urinary diversion
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Lattimer JK, Smith MJ. Exstrophy closure: a followup on 70 cases. J Urol. 1966;95(3):356–9.
Gambhir L et al. Epidemiological survey of 214 families with bladder exstrophy–epispadias complex. J Urol. 2008;179(4):1539–43.
Nelson CP, Dunn RL, Wei JT. Contemporary epidemiology of bladder exstrophy in the United States. J Urol. 2005;173(5):1728–31.
Wood HM, Babineau D, Gearhart JP. In vitro fertilization and the cloacal/bladder exstrophy–epispadias complex: a continuing association. J Pediatr Urol. 2007;3(4):305–10.
Muecke EC. The Role of the Cloacal Membrane in Exstrophy: The First Successful Experimental Study. J Urol. 1964;92:659–67.
Martinez-Frias ML et al. Exstrophy of the cloaca and exstrophy of the bladder: two different expressions of a primary developmental field defect. Am J Med Genet. 2001;99(4):261–9.
Ambrose SS, O'Brien III DP. Surgical embryology of the exstrophy–epispadias complex. Surg Clin North Am. 1974;54(6):1379–90.
Dodson JL et al. The newborn exstrophy bladder inadequate for primary closure: evaluation, management and outcome. J Urol. 2001;165(5):1656–9.
Baka-Jakubiak M. Combined bladder neck, urethral and penile reconstruction in boys with the exstrophy–epispadias complex. BJU Int. 2000;86(4):513–8.
Diamond DA et al. Normal urodynamics in patients with bladder exstrophy: are they achievable? J Urol. 1999;162(3 Pt 1):841–4. discussion 844-5.
Mathews R et al. Neural innervation of the newborn exstrophic bladder: an immunohistochemical study. J Urol. 1999;162(2):506–8.
Canning DA et al. The cephalotrigonal reimplant in bladder neck reconstruction for patients with exstrophy or epispadias. J Urol. 1993;150(1):156–8.
Mathews R, Hubbard JS, Gearhart JP. Ureteral reimplantation before bladder neck plasty in the reconstruction of bladder exstrophy: indications and outcomes. Urology. 2003;61(4):820–4.
Sponseller PD et al. The anatomy of the pelvis in the exstrophy complex. J Bone Joint Surg Am. 1995;77(2):177–89.
Stec AA et al. Evaluation of the bony pelvis in classic bladder exstrophy by using 3D-CT: further insights. Urology. 2001;58(6):1030–5.
Connolly JA et al. Prevalence and repair of inguinal hernias in children with bladder exstrophy. J Urol. 1995;154(5):1900–1.
Diamond DA, Jeffs RD. Cloacal exstrophy: a 22-year experience. J Urol. 1985;133(5):779–82.
•• Stec AA et al. Evaluation of pelvic floor muscular redistribution after primary closure of classic bladder exstrophy by 3-dimensional magnetic resonance imaging. J Urol. 2012;188(4 Suppl):1535–42. Utilizing safe and modern technology, 3D MRI imaging provides a new frontier for evaluating exstrophy–epispadias patients. Not only can specific dimensions of the soft tissue be associated with specific outcomes, but one may also use these dimensions to help guide current procedures and techniques.
Woodhouse CR, Hinsch R. The anatomy and reconstruction of the adult female genitalia in classical exstrophy. Br J Urol. 1997;79(4):618–22.
• Stec AA et al. Colorectal anomalies in patients with classic bladder exstrophy. J Pediatr Surg. 2011;46(9):1790–3. Colorectal anomalies occur in 1.6 % of CBE patients, a 72-fold increase compared to the general population. Physicians confronted with CBE should be aware of possible colorectal malformations and promptly evaluate and treat them.
Hurwitz RS et al. Cloacal exstrophy: a report of 34 cases. J Urol. 1987;138(4 Pt 2):1060–4.
Silver RI et al. Penile length in adulthood after exstrophy reconstruction. J Urol. 1997;157(3):999–1003.
• Ansari MS et al. The application of pelvic osteotomy in adult female patients with exstrophy: applications and outcomes. BJU Int. 2011;108(6):908–12. The six exstrophy–epispadias patients who had previously undergone bladder closure presented with uterine prolapse or concerns about the appearance of their genitalia or abdominal wall. This study provides details about the possible genitalia presentations in the exstrophy–epispadias complex that physicians should be acknowledge.
Cadeddu JA et al. Spinal abnormalities in classic bladder exstrophy. Br J Urol. 1997;79(6):975–8.
McLaughlin KP et al. Cloacal exstrophy: the neurological implications. J Urol. 1995;154(2 Pt 2):782–4.
Ebert AK et al. The exstrophy–epispadias complex. Orphanet J Rare Dis. 2009;4:23.
Gearhart JP et al. Criteria for the prenatal diagnosis of classic bladder exstrophy. Obstet Gynecol. 1995;85(6):961–4.
Mirk P, Calisti A, Fileni A. Prenatal sonographic diagnosis of bladder extrophy. J Ultrasound Med. 1986;5(5):291–3.
•• Goyal A et al. Antenatal diagnosis of bladder/cloacal exstrophy: challenges and possible solutions. J Pediatr Urol. 2012;8(2):140–4. The prospective study demonstrates that even with classic ultrasound characteristics of exstrophy, only 25 % of the newborns were diagnosed prenatally. Radiologists should be aware of these characteristics so that more children are diagnosed prenatally since 5 of 16 pregnancies with suspicion of exstrophy were terminated. MRI and karyotyping are other prenatal diagnostic modalities that can be explored.
Nelson CP et al. Bladder exstrophy in the newborn: a snapshot of contemporary practice patterns. Urology. 2005;66(2):411–5.
Ebert AK et al. Long-term follow-up of male patients after reconstruction of the bladder-exstrophy–epispadias complex: psychosocial status, continence, renal and genital function. J Pediatr Urol. 2010;6(1):6–10.
Baird AD, Nelson CP, Gearhart JP. Modern staged repair of bladder exstrophy: a contemporary series. J Pediatr Urol. 2007;3(4):311–5.
Novak TE et al. Failed exstrophy closure: management and outcome. J Pediatr Urol. 2010;6(4):381–4.
Mathews R. Achieving urinary continence in cloacal exstrophy. Semin Pediatr Surg. 2011;20(2):126–9.
Chan DY, Jeffs RD, Gearhart JP. Determinants of continence in the bladder exstrophy population: predictors of success? Urology. 2001;57(4):774–7.
Nelson CP et al. Economic impact of failed or delayed primary repair of bladder exstrophy: differences in cost of hospitalization. J Urol. 2008;179(2):680–3.
Gearhart JP et al. The multiple reoperative bladder exstrophy closure: what affects the potential of the bladder? Urology. 1996;47(2):240–3.
• Baradaran N et al. Effect of failed initial closure on bladder growth in children with bladder exstrophy. J Urol. 2011;186(4):1450–4. The authors determined that patients with failed bladder closures have significantly smaller cystographic capacities and slower bladder growth compared to children with successful primary closures. This data highlights the importance of succeeding in the closing the defect for the first time.
Oesterling JE, Jeffs RD. The importance of a successful initial bladder closure in the surgical management of classical bladder exstrophy: analysis of 144 patients treated at the Johns Hopkins Hospital between 1975 and 1985. J Urol. 1987;137(2):258–62.
McMahon DR et al. Vesical neck reconstruction in patients with the exstrophy–epispadias complex. J Urol. 1996;155(4):1411–3.
• Rubenwolf PC et al. Persistent histological changes in the exstrophic bladder after primary closure-a cause for concern? J Urol. 2013;189(2):671–7. Analyzing bladder biopsies, the authors found inflammatory, proliferative, and metaplastic in CBE patients undergoing primary bladder closure, secondary reconstructive procedures, and cystectomy for failed reconstruction. While dysplasia or neoplasia were not observes, patients may be at risk for bladder metaplasia and abnormal urothelial differentiation with a prolonged exstrophied bladder. Furthemore, these changes may persist after closure indicating that these patient may be at an increased risk for dysplasia or neoplasia.
Corica FA et al. Intestinal metaplasia is not a strong risk factor for bladder cancer: study of 53 cases with long-term follow-up. Urology. 1997;50(3):427–31.
Chalmers D, Ferrer F. Continent urinary diversion in the epispadias-exstrophy complex. Semin Pediatr Surg. 2011;20(2):102–8.
Woodhouse CR, North AC, Gearhart JP. Standing the test of time: long-term outcome of reconstruction of the exstrophy bladder. World J Urol. 2006;24(3):244–9.
Surer I et al. Continent urinary diversion and the exstrophy–epispadias complex. J Urol. 2003;169(3):1102–5.
Jeffs RD. Functional closure of bladder exstrophy. Birth Defects Orig Artic Ser. 1977;13(5):171–3.
Novak TE et al. Polyps in the exstrophic bladder. A cause for concern? J Urol. 2005;174(4 Pt 2):1522–6. discussion 1526.
Grady RW, Mitchell ME. Complete primary repair of exstrophy. J Urol. 1999;162(4):1415–20.
Mitchell ME, Bagli DJ. Complete penile disassembly for epispadias repair: the Mitchell technique. J Urol. 1996;155(1):300–4.
El-Sherbiny MT, Hafez AT. Complete repair of bladder exstrophy in boys: can hypospadias be avoided? Eur Urol. 2005;47(5):691–4.
Schaeffer AJ et al. Complete primary repair of bladder exstrophy: a single institution referral experience. J Urol. 2011;186(3):1041–6.
Husmann DA, Gearhart JP. Loss of the penile glans and/or corpora following primary repair of bladder exstrophy using the complete penile disassembly technique. J Urol. 2004;172(4 Pt 2):1696–700. discussion 1700-1.
Alpert SA et al. Bladder neck fistula after the complete primary repair of exstrophy: a multi-institutional experience. J Urol. 2005;174(4 Pt 2):1687–9. discussion 1689-90.
Shnorhavorian M et al. Long-term followup of complete primary repair of exstrophy: the Seattle experience. J Urol. 2008;180(4 Suppl):1615–9. discussion 1619-20.
Hammouda HM, Kotb H. Complete primary repair of bladder exstrophy: initial experience with 33 cases. J Urol. 2004;172(4 Pt 1):1441–4. discussion 1444.
Meldrum KK, Baird AD, Gearhart JP. Pelvic and extremity immobilization after bladder exstrophy closure: complications and impact on success. Urology. 2003;62(6):1109–13.
Gearhart JP et al. A combined vertical and horizontal pelvic osteotomy approach for primary and secondary repair of bladder exstrophy. J Urol. 1996;155(2):689–93.
Arlen AM et al. Safety and efficacy of spica casts for immobilization following initial bladder closure in classic bladder exstrophy. J Pediatr Urol. 2011;7(4):456–9.
Novak TE. Failed exstrophy closure. Semin Pediatr Surg. 2011;20(2):97–101.
Sponseller PD et al. Anterior innominate osteotomy in repair of bladder exstrophy. J Bone Joint Surg Am. 2001;83-A(2):184–93.
Conflict of Interest
Dr. Brian M. Inouye reported no potential conflicts of interest relevant to this article.
Dr. Eric Z. Massanyi reported no potential conflicts of interest relevant to this article.
Dr. Heather Di Carlo reported no potential conflicts of interest relevant to this article.
Dr. Bhavik B. Shah reported no potential conflicts of interest relevant to this article.
Dr. John P. Gearhart reported no potential conflicts of interest relevant to this article.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Inouye, B.M., Massanyi, E.Z., Di Carlo, H. et al. Modern Management of Bladder Exstrophy Repair. Curr Urol Rep 14, 359–365 (2013). https://doi.org/10.1007/s11934-013-0332-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11934-013-0332-y