Abstract
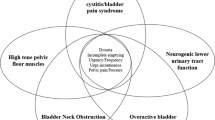
The American Urological Association recently developed guidelines to assist clinicians who evaluate and treat interstitial cystitis/bladder pain syndrome. Knowledge in this area continues to advance, and some of the guideline statements differ from what clinicians may have been previously taught. This review includes the 27 guideline statements, which address both evaluation and treatment. This review lists the guideline statements and, when applicable, comments on their practical implementation and the most recent research. Practical information includes the following: key questions that help in the differential diagnosis, when to perform cystoscopy and urodynamics, how to recognize and treat Hunner lesions, useful practical resources for patients and clinicians, information on elimination diet and stress management, initial selection of oral and intravesical medications, and description of advanced treatment options (limited to dedicated, experienced clinicians).

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
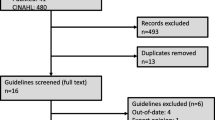
••Hanno PM, Burks DA, Clemens JQ, et al. AUA guideline for the diagnosis and treatment of interstitial cystitis/bladder pain syndrome. J Urol. 2011;185:2162–70. This is the AUA Guideline manuscript, on which this article is based. The document, algorithm, and slide presentation are available on the AUA Web site.
Tissot WD, Diokno AC, Peters KM. A referral center’s experience with transitional cell carcinoma misdiagnosed as interstitial cystitis. J Urol. 2004;172:478–80.
Braunstein R, Shapiro E, Kaye J, Moldwin R. The role of cystoscopy in the diagnosis of Hunner’s ulcer disease. J Urol. 2008;180:1383–6.
••Logadottir Y, Fall M, Kåbjörn-Gustafsson C, Peeker R. Clinical characteristics differ considerably between phenotypes of bladder pain syndrome/interstitial cystitis. Scand J Urol Nephrol. 2012; Epub ahead of print. This is the latest update on clinical differences between patients with and without Hunner lesions.
Koziol JA. Epidemiology of interstitial cystitis. Urol Clin N Am. 1994;21(1):7–20.
Novicki DE, Larson TR, Swanson SK. Interstitial cystitis in men. Urology. 1998;52:621–4.
http://my.clevelandclinic.org/Documents/Urology/Transcript_IC.pdf.
Cetinel S, Cetinel B, Ercan F, et al. Indomethacin-induced morphologic changes in the rat urinary bladder epithelium. Urology. 2003;61:236–42.
Buchbinder R, Forbes A, Kobben F, et al. Clinical features of tiaprofenic acid (surgam) associated cystitis and a study of risk factors for its development. J Clin Epidemiol. 2000;53:1013–9.
Ghose K. Cystitis and nonsteroidal antiinflammatory drugs: an incidental association or an adverse effect? N Z Med J. 1993;106:501–3.
Erickson DR. The placebo response. J Urol. 2009;181:945–6.
van Ophoven A, Pokupic S, Heinecke A, et al. A prospective, randomized, placebo controlled, double-blind study of amitriptyline for the treatment of interstitial cystitis. J Urol. 2004;172:533–6.
•Foster Jr HE, Hanno PM, Nickel JC, et al. Effect of amitriptyline on symptoms in treatment naïve patients with interstitial cystitis/painful bladder syndrome. J Urol. 2010;183:1853–8. At first glance, this article appears to show no benefit to amitriptyline, but it is important to note that all patients in this study received education, which was likely to contribute to symptom improvement in the placebo group.
Moldwin RM. The interstitial cystitis survival guide. Oakland: New Harbinger Publications; 2000.
••Friedlander JI, Shorter B, Moldwin RM. Diet and its role in interstitial cystitis/bladder pain syndrome (IC/BPS) and comorbid conditions. BJU Int. 2012;109:1584–91. This discussion of diet in IC/BPS includes practical steps for an elimination diet trial.
••Buffington CA. Idiopathic cystitis in domestic cats--beyond the lower urinary tract. J Vet Intern Med. 2011;25:784–96. This article discusses the role of the nervous system in feline IC, including a description of how the feline symptoms improve with environmental changes alone.
Thilagarajah R, Witherow RO, Walker MM. Oral cimetidine gives effective symptom relief in painful bladder disease: a prospective, randomized, double-blind placebo-controlled trial. BJU Int. 2001;87:207–12.
Hill JR, Isom-Batz G, Panagopoulos G, et al. Patient perceived outcomes of treatments used for interstitial cystitis. Urology. 2008;71:62–6.
Taneja R. Intravesical lignocaine in the diagnosis of bladder pain syndrome. Int Urogynecol J. 2010;21:321–4.
Parsons CL. Successful downregulation of bladder sensory nerves with combination of heparin and alkalinized lidocaine in patients with interstitial cystitis. Urology. 2005;65:45–8.
••Parsons CL, Zupkas P, Proctor J, et al. Alkalinized lidocaine and heparin provide immediate relief of pain and urgency in patients with interstitial cystitis. J Sex Med. 2012;9:207–12. In this single-dose trial, the lidocaine cocktail was more effective than placebo.
••Nickel JC, Moldwin R, Lee S, et al. Intravesical alkalinized lidocaine (PSD597) offers sustained relief from symptoms of interstitial cystitis and painful bladder syndrome. BJU Int. 2009;103:910–8. After five daily doses, alkalinized lidocaine was more effective than placebo.
Davis EL, El Khoudary SR, Talbott EO, et al. Safety and efficacy of the use of intravesical and oral pentosan polysulfate sodium for interstitial cystitis: a randomized double-blind clinical trial. J Urol. 2008;179:177.
••Lv YS, Zhou HL, Mao HP, et al. Intravesical hyaluronic acid and alkalinized lidocaine for the treatment of severe painful bladder syndrome/interstitial cystitis. Int Urogynecol J. 2012; Epub ahead of print. This three-arm trial included alkalinized lidocaine alone, hyaluronic acid alone, or both together. At week 4, all groups had approximately a 30 % response rate. At week 24, response rates were about 68 % for the two hyaluronic acid groups but only about 8 % for alkalinized lidocaine alone.
Welk BK, Teichman JM. Dyspareunia response in patients with interstitial cystitis treated with intravesical lidocaine, bicarbonate, and heparin. Urology. 2008;71:67–70.
Nickel JC, Steele SS, Lekstrom-Himes J, et al. Ascending dose cohort study of LiRIS® (lidocaine-releasing intravesical system) in women with moderate to severe interstitial cystitis [abstract 825]. Presented at the AUA 2012 Annual Meeting, Atlanta, Georgia, May 21, 2012.
•Quillin R, Hooper G, Erickson D. Intravesical bupivacaine for lidocaine-refractory patients with painful bladder syndrome/interstitial cystitis. Neurourol Urodyn. 2010;29:299. The important clinical message is not to give up if lidocaine fails; some of these patients will respond to bupivacaine.
Cole EE, Scarpero HM, Dmochowski RR. Are patient symptoms predictive of the diagnostic and/or therapeutic value of hydrodistention? Neurourol Urodyn. 2005;24:638–42.
Hanno PM, Wein AJ. Conservative therapy of interstitial cystitis. Semin Urol. 1991;9:143–7.
Erickson DR, Kunselman AR, Bentley CM, et al. Changes in urine markers and symptoms after bladder distention for interstitial cystitis. J Urol. 2007;177:556–60.
••Hanno PM. Bladder pain syndrome (Interstitial cystitis) and related disorders. In: Wein AJ, Kavoussi LR, Novick AC, et al., editors. Campbell-Walsh urology. 10th ed. Philadelphia: Saunders; 2012. p. 357–401. This is a superb comprehensive chapter.
Peeker R, Fall M. Toward a precise definition of interstitial cystitis: further evidence of differences in classic and nonulcer disease. J Urol. 2002;167:2470–2.
Parsons CL. Interstitial cystitis: clinical manifestations and diagnostic criteria in over 200 cases. Neurourol Urodyn. 1990;9:241–50.
Rofeim O, Hom D, Freid RM, et al. Use of the neodymium: YAG laser for interstitial cystitis: a prospective study. J Urol. 2001;166:134.
••Cox M, Klutke JJ, Klutke CG. Assessment of patient outcomes following submucosal injection of triamcinolone for treatment of Hunner’s ulcer subtype interstitial cystitis. Can J Urol. 2009;16:4536–40. This is the first published description of triamcinolone injection for Hunner lesions.
Mayer R. Beyond the front lines: what to consider when initial therapy just isn’t enough. ICA Update Spring 2012.
•Forrest JB, Payne CK, Erickson DR. Cyclosporine A for refractory interstitial cystitis/bladder pain syndrome: experience of three tertiary centers. J Urol. in press, 2012. Cyclosporine A was life-altering in some of the Hunner lesion patients, but adverse events included renal insufficiency and hypertension, and some patients stopped the drug due to adverse events. In contrast, patients without Hunner lesions had a low success rate.
Smith Jr JA. No good options. J Urol. 2011;185:8–9.
Hohenfeller M, Linn J, Hampel C, Thuroff JW. Surgical treatment of interstitial cystitis. In: Sant GR, editor. Interstitial cystitis. Philadelphia: Lippincott-Raven; 1997. p. 223–33.
Lotenfoe RR, Christie J, Parsons A, et al. Absence of neuropathic pelvic pain and favorable psychological profile in the surgical selection of patients with disabling interstitial cystitis. J Urol. 1995;154:2039–42.
American Urological Association Education and Research, Inc. Interstitial cystitis/bladder pain syndrome/ IC/BPS clinical guideline. Available at http://www.auanet.org/content/media/IC%20Slide%20Presentation.2011.ppsx. Accessed June 2012.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Quillin, R.B., Erickson, D.R. Practical Use of the New American Urological Association Interstitial Cystitis Guidelines. Curr Urol Rep 13, 394–401 (2012). https://doi.org/10.1007/s11934-012-0263-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11934-012-0263-z