Abstract
This article discusses the use of antibiotic prophylaxis in the treatment of three common conditions encountered by the pediatric urologist: 1) children with urinary infection and structurally and neurologically normal urinary tracts; 2) children with vesicoureteral reflux (VUR); and 3) children with prenatally diagnosed ureteropelvic and ureterovesical obstruction. The literature remains unclear and contradictory. Additional significant risk factors for recurrent infection are age, circumcision status in boys, and toileting function. The evidence for the use of prophylaxis is best in those with VUR, although not everyone with VUR must be on medication. In the absence of definitive evidence, the clinician must individualize the treatment of each patient and family.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Wan J, Kaplinsky R, Greenfield, SP: Toilet habits of children evaluated for urinary tract infection. J Urol 1995, 154:797–799.
Farhat W, Bagli DJ, Capolicchio G, et al.: The dysfunctional voiding scoring system: quantitative standardization of dysfunctional voiding symptoms in children. J Urol 2000, 164:1011–1015.
Conway PH, Cnaan A, Zaoutis T, et al: Recurrent urinary tract infections in children: risk factors and association with prophylactic antimicrobials. JAMA 2007, 298:179–186.
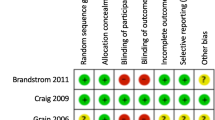
Craig JC, Simpson JM, Williams GJ, et al.: Antibiotic prophylaxis and recurrent urinary tract infection in children. NEJM 2009, 361:1748–1759.
• Williams G, Craig JC: Prevention of recurrent urinary tract infection in children. Curr Op Inf Dis 2009, 22:72–76. This was a large prospective study of children with and without reflux, showing a slight advantage to prophylaxis.
Mori R, Fitzgerald A, Williams C, et al.: Antibiotic prophylaxis for children at risk of developing urinary tract infection: a systemic review. Acta Paed 2009, 98:1781–1786.
Montini G, Rigon L, Zuchetta P, et al.: Prophylaxis after first febrile urinary tract infection in children? A multicenter, randomized, controlled noninferiority trial. Pediatrics 2007, 122:1064–1071.
Williams G, Wei L, Lee A, et al.: Long term antibiotics for preventing recurrent urinary tract infection in children (review). Cochrane Collaboration in the Cochrane Library 2009, John Wiley & Sons, Ltd pp 1–28.
Cascio S, Colhoun E, Puri P: Bacterial colonization of the prepuce in boys with vesicoureteral reflux who receive antibiotic prophylaxis. J Peds 2000, 139:160–162.
Fisch N, Ashkenazi S, Davidowitz M: Prophylactic antibiotics and evaluation scheme following febrile urinary tract infection in children: a nationwide Israeli survey. IMAJ 2009, 11:677–682.
Chevalier I, Benoit G, Gauthier M, et al.: Antibiotic prophylaxis for childhood urinary tract infection: a national survey. J Ped Child Health 2008, 44:572–578.
Cheng CH, Ming-Horng T, Yhu-Chering H, et al.: Antibiotic resistance patterns of community-acquired urinary tract infections in children with vesicoureteral reflux receiving prophylactic antibiotic therapy. Peds 2008, 122:1212–1217.
Lee SJ, Shim YH, Cho SJ, et al.: Probiotics prophylaxis in children with persistent primary vesicoureteral reflux. Pediatr Nephrol 2007, 22:1315–1320.
Greenfield SP, Ng M, Wan J: Experience with vesicoureteral reflux in children: clinical characteristics. J Urol 1997, 158:574–577.
Cooper CS, Chung BI, Kirsch AJ, et al.: The outcome of stopping prophylactic antibiotics in older children with vesicoureteral reflux. J Urol 2000, 163:269–273.
Garin EH, Olavarria F, Garcia NV, et al.: Clinical significance of primary vesicoureteral reflux and urinary antibiotic prophylaxis after acute pyelonephritis: a multicenter, randomized, controlled study. Peds 2006, 117:626–632.
Roussey-Kesler G, Gadjos V, Idres N, et al.: Antibiotic prophylaxis for the prevention of recurrent urinary tract infection in children with low grade vesicoureteral reflux: results from a prospective randomized study. J Urol 2008, 179:674–679.
Brandstrom P, Esbjorner E, Herthelius M, et al.: The Swedish reflux trial in children: I. Study design and study population characteristics. J Urol 2010, 184:274–279.
•• Brandstrom P, Esbjorner E, Herthelius M, et al.: The Swedish reflux trial in children: III. Urinary tract infection pattern. J Urol 2010, 184:286–291. The authors studied a well-defined group of children with grade 3 or 4 reflux who had a significant decrease in recurrent infections on prophylaxis.
•• Brandstrom P, Neveus T, Sixt R, et al.: The Swedish reflux trial in children: IV. Renal Damage. J Urol 2010, 184:292–297. The authors studied a well-defined group of children with grade 3 or 4 reflux who had significant prevention of new renal scarring while on prophylaxis.
Sillen U, Brandstrom P, Jodal U, et al.: The Swedish reflux trial in children: V. Bladder dysfunction. J Urol 2010, 184:298–304.
Al-Sayyad A, Pike J, Leonard MP: Can prophylactic antibiotics safely be discontinued in children with vesicoureteral reflux? J Urol 2005, 174:1587–1589.
Georgaki-Angelaki H, Kostaridou S, Daikos GL, et al.: Long-term follow-up of children with vesicoureteral reflux with and without antibiotic prophylaxis. Scand J Inf Dis 2005, 37:842–845.
Kitchens DM, Herndon A, Joseph DB: Outcome after discontinuing prophylactic antibiotics in children with persistent vesicoureteral reflux. J Urol 2010, 184:1594–1597.
•• Peters CA, Skoog SJ, Arant BS, et al.: Summary of the AUA guideline on management of primary vesicoureteral reflux in children. J Urol 2010, 184:1134–1144. This is the most comprehensive meta-analysis of the literature, with well-reasoned conclusions regarding therapy.
•• Keren R, Carpenter MA, Hoberman A, et al.: Rationale and design issues of the randomized intervention for children with vesicoureteral reflux (RIVUR) study. Peds 2008, 5(Suppl):5240–5250. This article provides a comprehensive discussion of the RIVUR trial and its aims.
• Greenfield SP, Chesney RW, Carpenter M, et al.: Vesicoureteral reflux: the RIVUR study and the way forward. J Urol 2008, 179:405–407. This article provides a succinct analysis of the shortcomings of the current literature and a brief description of the RIVUR trial.
Copp HL, Nelson CP, Shortliffe LD, et al.: Compliance with antibiotic prophylaxis in children with vesicoureteral reflux: results from a national pharmacy claims data base. J Urol 2010, 183:1994–2000.
Wan J, Greenfield SP, Talley M, et al.: An analysis of social and economic factors associated with followup of patients with vesicoureteral reflux. J Urol 1996, 156:668–672.
Ogan K, Pohl H, Carlson D, et al.: Parental preferences in the management of vesicoureteral reflux. J Urol 2001, 240–243.
Woodward M, Frank D: Postnatal management of antenatal hydronephrosis. BJU Int 2002, 89:149–156.
Lee JH, Choi HS, Kim JK, et al.: Nonrefluxing neonatal hydronephrosis and the risk of urinary tract infection. J Urol 2008, 179:1524–1528.
• Roth CC, Hubanks JM, Bright BC, et al.: Occurence of urinary tract infection in children with significant upper urinary tract obstruction. Urology 2009, 73:74–78. The authors studied a well-defined group of infants with prenatally diagnosed UPJO and UVJO who were followed off prophylaxis.
Greenfield SP, Deshmukh S, Williot P: Prenatally detected primary ureterovesical junction obstruction: are prophylactic antibiotics necessary? Presented at the Urology Section, American Academy of Pediatrics, Washington, DC October 2009.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Greenfield, S.P. Antibiotic Prophylaxis in Pediatric Urology: An Update. Curr Urol Rep 12, 126–131 (2011). https://doi.org/10.1007/s11934-010-0164-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11934-010-0164-y